Understanding Medicaid and Medicare Programs in Seattle-King County Coalition on Homelessness Training
Gain insights into the complexities of Medicaid and Medicare programs with a focus on eligibility, requirements, applications, and the intersection between the two. Learn about MAGI and Classic Medicaid, Medicare Savings Program, and how to avoid benefit pitfalls. Discover the nuances of Washington Apple Health programs and be informed about systemic racism in public benefits policies.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
SEATTLE KING COUNTY COALITION ON HOMELESSNESS MEDICAID AND MEDICARE PROGRAM OVERVIEW TRAINING JULY 21, 2022 THE BASICS IN UNDERSTANDING ELIGIBILTY, REQUIREMENT, APPLICATION AND THE INTERSECTIION BETWEEN MEDICAID AND MEDICARE Will Ross, Benefits Attorney Hannah Rosenberger, Benefits Attorney Benefits Legal Assistance Sara Robbins, Seattle King County Coalition on Homelessness solid-ground.org 206.694.6700
Before we begin Remember that public benefits laws and policies are steeped in systemic racism. http://theconversation.com/how-racism-has-shaped-welfare-policy-in-america- since-1935-63574 https://slate.com/human-interest/2018/06/trump-administrations-fixation-on- work-requirements-for-snap-benefits-is-part-of-a-long-racist-policy- history.html Be aware of the impact of casual racism and stereotypes when speaking about recipients of public benefits. https://www.npr.org/sections/codeswitch/2018/06/08/616684259/why-more- white-americans-are-opposing-government-welfare-programs https://www.huffingtonpost.com/entry/americans-welfare-perceptions- survey_us_5a7880cde4b0d3df1d13f60b solid-ground.org 206.694.6700
Topics Covered MAGI Medicaid Categorically Needy Medicaid Medically Needy and Spenddown Brief Overview of Medicare Medicare Savings Program Long Term Challenges Benefit Pitfalls and How to Avoid them How to Appeal? How to Refer a case to Solid Ground! solid-ground.org 206.694.6700
MEDICAID=WASHINGTON APPLE HEALTH solid-ground.org 206.694.6700
THERE ARE TWO WASHINGTON APPLE HEALTH (MEDICAID) PROGRAMS MAGI Medicaid: Adult, Children s, Family and Pregnancy MAGI stands for Modified Adjusted Gross Income which is your adjusted gross income (AGI) on your Tax Form 1040 plus or minus some other types of income. Classic (Non-MAGI) Medicaid: Long Term Care/Aged, Blind, Disabled (ABD) Program Classic Medicaid is for people who are aged, blind or disabled. solid-ground.org 206.694.6700
MAGI and Classic Medicaid at a Glance MAGI Medicaid Classic Medicaid Age 64 & younger Not eligible for Medicare Low Income: Children Adults Pregnant Persons Parents/Caretakers of Medicaid eligible child under 19 yrs. Low Income individuals who meet any of the following: Age 65+ Blind Disabled by Social Security Administration (SSA) Standards solid-ground.org 206.694.6700
Who can get Medicaid under the MAGI program? Pregnant women. Children under 19. Parents/Caretaker relatives (people who live with their own child, grandchild or another relative or step-relative, under age 18 or under 19 if a full time student). Childless adults ages 19-64, including disabled individuals who are NOT on Medicare. Those who are on a family planning services program. solid-ground.org 206.694.6700
What type of income counts towards MAGI Medicaid eligibility? Wages. Taxable interest. Dividends. Unemployment Benefits. Pensions IRA distributions. Alimony. Income from self-employment. State income tax refunds. Rental income. Social Security Benefits (this is true even if your benefits are not taxable). solid-ground.org 206.694.6700
What income does not count towards MAGI Medicaid eligibility? Worker s Compensation. Veterans Administration benefits. Child Support. Certain scholarship income American Indian income. Gift or inheritance money. solid-ground.org 206.694.6700
What are the income limits for the MAGI Program? Category Federal Poverty Level Limit (MAGI Income) 1 Person Household 2 Person Household 3 Person Household New Adult (Age 19 65) 133% FPL $1507 $2030 $2553 Pregnant Persons 193% FPL $2187 $2945 $3704 Apple Health for Kids (no premiums) 210% FPL $2379 $3205 $4031 Apple Health for Kids ($30 premium) 312% FPL $3534 $4761 $5988 Family Planning Program 260% $2945 $3968 $4990 solid-ground.org 206.694.6700
Does MAGI allow deductions from income? Yes! The following deductions are allowed: Alimony paid. Certain moving expenses. Student loan interest. Self-employed health insurance contributions. Self-employment tax. IRA deductions. Money contributed to a flex spending plan solid-ground.org 206.694.6700
Whose income is counted to determine MAGI? Income is counted from everyone in the Medicaid tax household. A Medicaid tax household typically consist of the applicant, their spouse and dependents who are required to file tax returns. This is not the same as applicant household However, like all rules there are exceptions. An important exception is for children claimed as dependents by parents. If a child has enough income to require that child to file a tax return then the child s income is counted in the household. Dependent children must file income tax if they earn more than $12, 550.00 through employment and/or more than $1,100 in unearned income If the child is NOT required to file a tax return then the child s income is NOT counted in the household. This is true even if the child chooses to file a tax return. solid-ground.org 206.694.6700
Example of Household Income Jake and Kimberly Whitney are married with two mutual children, ages 11 and 15. Kimberly has a 17 son from a previous marriage that lives with them. Jake s 18 and 21 year old daughters live with them as well. Jake and Kimberly own a landscaping business. Their 15 child works full time for their parents during the summer earning $4000 for the year, based on the income tax they filed. The 11 year old child receives $110.00/ month in SSI benefits. Kimberly s 17 year son receives $8000 annually in tribal money. Jake s 18 daughter is at the UW on a partial scholarship and works part time earning $1100/ month. His 21 year daughter has just graduate from college and is about to start her first full time job. Whose income must be counted? solid-ground.org 206.694.6700
Whose Income and What Income Counts Jake s and Kimberly s income from their business is included as self employment The 11 year old SSI income The earned income of Jake s 18 year daughter because she is under the age of 19 and is a student, her scholarship money may be excluded The 17 year olds son s income is excluded because it is money from the tribe The 15 year old son s income is excluded because he earns less than $12,550/year and is not required to file income tax The 21 year daughter income would not be included and she would need to be eligible for her own separate Medicaid case. solid-ground.org 206.694.6700
MAGI and Assets and Income Changes ASSETS Limits to MAGI Medicaid is based on SSI standards Eligibility for Medicaid is determined for twelve months and will not change if the recipient s income increases during the eligibility period solid-ground.org 206.694.6700
MAGI Medicaid asset limits is based on SSI standards with a caveat. The Affordable Care Act simplifies Medicare eligibility and enrollment for millions of Americans. Qualifying with MAGI simplifies the application process. The administrative burden of identifying assets is set aside, although this is not true if you are seeking long-term nursing home care or if you are seeking cash or food benefits. Consequently asset-rich people, especially those with investments or real estate, may still technically meet MAGI criteria. Eligibility for Medicaid is determined for twelve months and will not change if the recipient s income increases during the eligibility period solid-ground.org 206.694.6700
Tips for Advocates Managed Care Organization Most Washington Medicaid members will be enrolled in an Apple Health Managed Care Plan. Managed care means that you have a set doctor network to choose from, which means that your doctors and specialists are more likely to have a line of communication with each other and you are more likely to get the best care possible. The plans are not all available in every area. All WA Medicaid plans include the same basic benefits, but each plan offers extras that may convince you to join one over another. Example of some extras may include: free cellphone, free Boys and Girls Club membership, GED testing, electric breast pump, acupuncture treatments, rides to medical appointments solid-ground.org 206.694.6700
Managed Care Organizations in Washington State There are five separate managed care plans: 1. Amerigroup Washington, 2. Coordinated Care of Washington, 3. Community Health Plan of Washington, 4. Molina Healthcare of Washington, and 5. United Healthcare Community Plan. solid-ground.org 206.694.6700
How To Help Clients Choose the MCO that is Best for Them Determine the specific medical needs of your clients and the individual needs of each family member. This may include foreseeable medical needs. Determine what resources or assistance your client could utilize to improve their wellness, examples could include family coaching or disability advocacy Apple Health, the Washington Medicaid Program: Ultimate Guide https://www.medicareplanfinder.com/medicaid-by-state/washington- medicaid/#plan describes what each MCO offers as extras Utilize the healthcare navigator on HealthPlanFinder https://www.wahealthplanfinder.org/ solid-ground.org 206.694.6700
Navigator Search Healthplanfinder has a network of support across Washington State. Please use the search fields below to find a Navigator who, at no additional cost, can help you find, compare and select a health plan. ORGANIZATION NAME LAST NAME ZIP SERVICE LANGUAGE(S) HELP REQUEST TYPE Notice: You must create a Washington Healthplanfinder account and provide your contact information in the "About You" screen in order for the Navigator that you select to be able to contact you. Alternatively, you can contact the Navigator using their contact information provided on screen.
How to Apply for Washington Apple Health Apply for or renew your Apple Health coverage if you are: An adult age 18 to 64 years old. Applying for children. A parent or caretaker applying with children. Pregnant or applying for someone who is pregnant. You can apply for Washington Apple Health through DSHS, particularly when applying for other benefits such as SNAP and TANF: https://www.washingtonconnection.org/home/ Customer Service 1-877-501-2233 You can also apply for Washington Apple Health through Washington HealthPlanFinder : Online: Go https://www.wahealthplanfinder.org/ - select the "Apply Now" button. Mobile app: Download the WAPlanfinder app select sign in or create an account . Phone: Call the Washington HealthPlanFinder Customer Support Center at 1-855-923-4633. Paper: Submit an Application for health care coverage (18-001P). In-person: Local resources who, at no additional cost, can help you apply for health coverage: Health Benefit Exchange Navigator solid-ground.org 206.694.6700
What You Will Need When You Apply Your household monthly income. Your immigration information, if that applies to you. Dates of birth for each member of your household. Social Security numbers (SSN) for each household member who is applying for coverage and has a SSN. Domestic Violence survivors may not be required to provide SSN. solid-ground.org 206.694.6700
Questions? solid-ground.org 206.694.6700
CLASSIC MEDICAID PROGRAMS solid-ground.org 206.694.6700
Classic Medicaid Eligible for Classic Medicaid if: 65 or older. Disabled. Blind. Have Medicaid with a Spenddown. Receive SSI. Go through the Medicaid Buy-In for Working People with Disabilities under the age of 65. At times, this is shortened to MBI-WPD. Have a Medicare Savings Program. Have Disabled Adult children. solid-ground.org 206.694.6700
Categorically Needy Program This is a Classic Medicaid Program A person who receives federal cash benefits under the Supplemental Security Income (SSI) program is automatically eligible to receive the Categorical Needy (CN) Medicaid Program The same income and resource for SSI apply to this program solid-ground.org 206.694.6700
Categorically Needy SSI-Related Program This program provides CN coverage to individuals who meet the SSI income and resource limits as well as one of the following requirements: 65 years old or older (aged), or Blind (as defined by the Social Security Administration and determined by DSHS), or Disabled (as defined by the Social Security Administration and determined by DSHS). This is the coverage for most people on ABD solid-ground.org 206.694.6700
Categorically Needy SSI Related Income & Resource Limits Household Size Monthly Income Limit Resource Limit Effective January 1, 2022 1 $841 $2,000 2 $1,261 $3,000 solid-ground.org 206.694.6700
How to Apply for Categorically Needy? When a person is approved for SSI or ABD (Aged, Blind Disabled) they may be auto-enrolled but as a precaution the client can apply below Apply for SSI through the Social Security Administration https://www.ssa.gov/locator/ Apply for ABD and Categorically Needy through DSHS https://www.washingtonconnection.org/home/ Customer Service 1-877-501-2233 In Person - https://www.dshs.wa.gov/office-locations solid-ground.org 206.694.6700
Questions? solid-ground.org 206.694.6700
Medically Needy Program The Medically Needy (MN) program provides Medicaid health care coverage for aged, blind, or disabled persons, institutionalized individuals, hospice individuals, pregnant women, children, and refugees with income above Categorically Needy (CN) standards and countable resources below the applicable MN resource standard. An individual may qualify for the MN program with or without spenddown. solid-ground.org 206.694.6700
Eligibility for Medically Needy Program Blind, aged, pregnant, disabled, a child, or the parent of a minor child. Have income that is too high for regular Medicaid eligibility Have medical expenses significant enough that when subtracted from the person's income, it brings the after- medical-expense income down to a level that the state deems eligible for Medicaid under its medically needy program. Limited assets (typically around $2,000 for a single individual). solid-ground.org 206.694.6700
Medically Needy Income and Resources Standards Household Size Monthly Income Standard Household Size Resource Limit 1 $2000 1 $841 2 $3000 2 $841 3 $3050 3 $841 4 $3100 4 $841 5 $3150 5 $858 6 $3200 6 $975 solid-ground.org 206.694.6700
How Medically Needy Program Works If you are eligible for the MN program, you can get Medicaid coverage once you incur a certain amount of medical expense during a specific period. This is called a spenddown amount or just a spenddown. Excess income is the amount of your countable income that exceeds the amount of your income set aside for non-medical expenses. The amount of monthly excess income you have will be used to determine your spenddown amount. solid-ground.org 206.694.6700
How Medically Needy Program Works cont. A base period is the time period used to calculate your spenddown amount. (3-6 months) DSHS will calculate your spenddown amount by multiplying the number of months in your base period by the amount of your monthly excess income. EX: Individual has $40 excess income and has a 3-month base period, their spenddown amount is $120 ($40*3). Once they have incurred $120 in medical expenses, their Medicaid coverage starts! solid-ground.org 206.694.6700
S P E N D D O W N
Medicaid Spend Down Example Sam gets $1200/month in Social Security Disability Sam gets a $20 deduction for unearned income so countable income is $1180 $1200-$20 = $1180 Sam gets to subtract $841 for non-medical expenses* (dollar amount changes annually) Sam s excess income is $339 $1180-$841 = $339 Sam choose a 3-month Base Period Spenddown Amount is = $339*3 = $1,017 As soon as Sam incurs medical bills for $1,017, Sam can start getting Medicaid coverage and Medicaid will pay bills for the rest of the 3 months! solid-ground.org 206.694.6700
Somethings to Remember about Spenddown The spend down and eligibility period is for three to six months. If a recipient has a 6-month eligibility period from January to June, the spenddown amount must be met before June. Medicaid will only pay the remaining balance of medical expenses through the end of June. In July, a new eligibility and spend down period will begin anew. Clients submit copies of bills to DSHS to go towards the spenddown amount. solid-ground.org 206.694.6700
Somethings to remember cont. The medical bills do not have to be paid, just incurred! Medical expenses which third parties are liable for do not count as part of spend down. Classic example are medical bills that auto insurance companies are liable for, even when it is the recipient s own insurer. For an expense to be allowed towards spenddown, the expense must have been prescribed by a licensed provider. solid-ground.org 206.694.6700
How to Apply for Medically Needy? Apply for Medically Needy Coverage through DSHS https://www.washingtonconnection.org/home/ Customer Service 1-877-501-2233 In Person - https://www.dshs.wa.gov/office-locations Once enrolled, submit proof of medical expenses to DSHS! Can submit copies of bills in person at the local CSO, mail or fax to DSHS Spenddown Unit solid-ground.org 206.694.6700
Questions solid-ground.org 206.694.6700
WHAT IS MEDICARE? Medicare is the federal health insurance program for: People who are 65 or older Certain younger people with disabilities People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD) Recipients of SSI Unlike Medicaid, Medicare has premium cost solid-ground.org 206.694.6700
Who Can Get Medicare? Medicare is a federal health insurance program administered by the Social Security Administration (SSA) and the Centers for Medicare and Medicaid Services (CMS). Medicare provides health care coverage for people who: Have worked under the Social Security or Railroad Retirement systems (for more Railroad Retirement information, see Worker Responsibilities, section 2 below) and: Are age 65 or older; or Have been receiving Social Security or Railroad disability benefits for at least 24 months; or Need continuing dialysis for permanent renal failure; or Have received a kidney transplant within the last thirty-six months; or Are receiving Supplemental Security Income (SSI) and; Meet the citizenship and alien status requirements in chapter 388-424; and Are age 65 or older or can draw Medicare based on having sufficient work quarters on their own or through a disabled parent. solid-ground.org 206.694.6700
WHAT ARE THE DIFFERENT PARTS OF MEDICARE? Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. Medicare Part D (prescription drug coverage) Helps cover the cost of prescription drugs (including many recommended shots or vaccines). solid-ground.org 206.694.6700
Medicare Premium Cost Most people have no premium for Medicare Part A The standard Part B premium amount is $170.10 (or higher depending on your income). The Part C monthly premium varies by plan. Compare costs for specific Part C plans https://www.medicare.gov/plan- compare/#/?year=2022&lang=en The Part D monthly premium varies by plan (higher-income consumers may pay more). Compare at link above solid-ground.org 206.694.6700
Medicare Part A Part A - Hospital Insurance Part A is free for people who have worked and: Have earned the required number of work quarters, or Have a spouse who has earned the required number of work quarters. Part A is also available at a cost for Medicare-entitled individuals who do not have the required number of work quarters for free Medicare Part A solid-ground.org 206.694.6700
Medicare Part B Part B - Health Insurance (doctor s visits) Everyone who enrolls in Part B must pay a monthly premium. solid-ground.org 206.694.6700
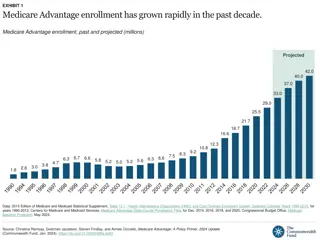
Part C - Optional Supplemental Health Insurance Part C is called Medicare Advantage and means a managed care plan. Medicare beneficiaries that choose Medicare Advantage (Part C) must be entitled to Medicare Part A and Medicare Part B or they cannot enroll in a Part C plan. Medicare Advantage (Part C) beneficiaries must pay a monthly premium in addition to Part A and Part B premiums when they enroll in a Part C plan. Several Part C plans doing business in Washington do not charge a monthly premium. Healthcare Authority (HCA) no longer pays Part C premiums. solid-ground.org 206.694.6700
Medicare Part D - Prescription Drug Program Part D benefits are available to all Medicare beneficiaries. To be eligible for Part D, the beneficiary must be enrolled in Medicare Part A or Part B. CMS automatically enrolls dual-eligible (i.e., eligible for both Medicaid and Medicare) and MSP individuals into a Part D plan. Dual-eligible individuals begin receiving most of their prescription drug benefits through Medicare and not Medicaid when they gain dual-eligibility status (CN or MN plus Medicare). Dual-eligible and MSP individuals may change to a different Part D plan every month if they choose. The requirement to purchase drugs through a Medicare Part D plan begins as soon as Medicaid (HCA) is notified of Medicare eligibility. Medicare has contracted with Limited Income Net (Humana) to provide prescription drug coverage for Medicaid individuals newly entitled to Medicare and not yet enrolled in a Part D plan. solid-ground.org 206.694.6700
Medicare Part D - Prescription Drug Program Cont. Pharmacies can bill the Limited Income Net (Humana) plan when a Medicaid individual has not yet enrolled in a Part D plan. Medicaid individuals must show proof of Medicaid eligibility and Medicare entitlement to the pharmacist. A Medicaid award letter is sufficient proof of Medicaid and a Medicare card or letter from SSA stating the effective date of Medicare is sufficient proof of Medicare entitlement. The Limited Income Net (Humana) plan can be reached at 1-800-783-1307. Dual-eligible and MSP individuals have copayment cost sharing for Part D covered drugs. Institutionalized and Home & Community Service waivered individuals are exempt from paying Part D copayments. If an HCBS waiver individual is still being charged Part D copayments at their pharmacy, refer the individual to contact CMS at 206-615-2354. For more information specific to long-term care individuals, see Medicare and Long-term Care. Medicaid continues to pay for some drugs that Medicare excludes under Medicare Part D rules solid-ground.org 206.694.6700