Understanding Alzheimer's Disease and Caregiver Stress
This content explores the impact of Alzheimer's disease on individuals and caregivers, covering statistics, characteristics of cognitive stages, caregiver challenges, and the progressive nature of the disease. It emphasizes the need for appropriate intervention strategies and the significant stress faced by caregivers, including social isolation, fatigue, and emotional distress.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Cindy Kempf, MA, OTR/L cindy@rpistl.com Lisa Meyer, MBA,PT Schorb_meyer@yahoo.com
Participants will be able to identify the basic characteristics of early, middle, and late stage cognitive levels in relation to functional activities. Participants will be able to understand how to determine appropriate interventional strategies to optimize function in adults with dementia. Participants will be able to implement a person program. Participants will be able to identify the basic characteristics of early, middle, and late stage cognitive levels in relation to functional activities. Participants will be able to understand how to determine appropriate interventional strategies to optimize function in adults with dementia. Participants will be able to implement a person- -directed Best Ability to Function program. directed Best Ability to Function
In 2016, more than 5. 4millions Americans have been diagnosed with Alzheimer s 37% of adults with Alzheimer s are over the age of 85 Every 66 seconds, another American develops Alzheimer s The cost for caring for people with a diagnosis of Alzheimer s in 2016 is estimated to be $236 billion (increased from $183 billion just a few years ago) It is the 6thleading cause of death and the only cause in the top 10 that can t be prevented, cured or slowed Deaths from Alzheimer s increased 66% since 2000 while deaths from most other diseases decreased http://www.alz.org/downloads/facts_figures_2016.pdf
In 2015, 15.9 million family members and friends provided 18.1 billion hours of free care to people with Alzheimer s 70% of people with AD are living at home, cared for by family and friends 59% of family caregivers report high levels of stress in 2014 poll 40% of family caregivers report symptoms of depression in 2014 poll
Confusion Fear / Grief Depression Social Isolation Fatigue / need for relief / respite Stress Missed days of work / rejection of promotions Decrease in exercise
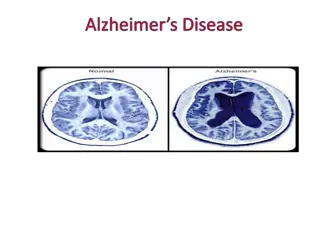
Progressive disease that destroys brain cells Problems with memory, thinking and behavior Alzheimer s is the most common form of dementia accounting for approximately 70% of dementia Alzheimer s disease is eventually fatal
Significant memory impairment with one or more of the following: Language disturbance (aphasia, dysnomia, dysfluency) Apraxia (impaired ability to carry out motor tasks) Agnosia (failure to recognize or identify objects) Executive Dysfunction (inability to organize and execute complex and / or multi-part behavioral sequences)
Lewy body visuospatial problems, extrapyramidal signs, visual hallucinations and fluctuations in alertness and attention. More common in men with onset in early 70 s Vascular preservation of episodic memory usually occurring within 3 months of a CVA. Abrupt onset. Lewy body: Combination of dementia with Vascular: executive impairment with relative
Frontotemporal Dementia late 50 s or early 60 s with prominent language, personality and behavioral changes. Memory usually is preserved until later in the course. Behavior interferes with the ability to interact with others Frontotemporal Dementia: young onset in
Delirium Delirium Dementia Dementia Depression Depression Onset Abrupt Slow, insidious Recent, may be associated with loss Stable, may be worse in the morning Usually normal Duration Hours to days Months to years Attention Impaired Normal, except severe cases Clear Consciousness Reduced, fluctuating Clear Silverstein & Maslow, 2006
Forgetfulness Word finding difficulty Apathy Poor attention Difficulty with complex tasks Depression Work trouble
Disorientation Increased memory loss Confusion Insomnia Wandering Speech difficulty Restlessness Difficulty with IADLs
Agnosia Apraxia Agression Agitation Incontinence Assist with basic ADLs Gait disturbance
Age: for every 5 year age group beyond 65, the % of people with AD doubles Family History : strong genetic component for some forms of dementia Gender: more common in women Life exposure factors Head trauma High cholesterol Lack of intellectual stimulation / education
Misidentification of early stages as part of normal aging Social skills are often maintained early in the disease Denial and lack of insight by the resident Social stigma associated with the diagnosis Lack of definitive screening and diagnostic tests
Clock Drawing Test Mini-Cog (recall of 3 non-related items) The AD-8: 8 Yes / No questions 2 or more yes responses present high correlation with the presence of dementia Functional Assessment The FAQ tests functional limitations / changes rather than cognitive changes Short Blessed Test
Test functional limitations / changes rather than just testing cognitive skills Sensitivity and specificity comparable to the MMSE Rating functional abilities over the past 4 weeks Not Applicable Normal Some difficulty but does by self Needs Assistance Dependent
Writing checks, paying bills, balancing checkbooks Assembling tax records, business affairs or papers Shopping alone for clothes, household necessities or groceries Playing a game of skill, working on a hobby Heating water, making a cup of coffee, turning off stove Preparing a balanced meal Keeping track of current events Paying attention to, understanding, discussing a TV show, book, magazine Remembering appointments, family occasions, holidays, medications Traveling out of neighborhood, driving, arranging to take buses
Problems with judgment Less interest in hobbies / activities Repeats the same things (questions, stories, statements) Trouble learning how to use a tool, appliance, gadget Forgets correct month or year Trouble handling complicated financial affairs Trouble remembering appointments Daily problems with thinking and / or memory
Questions are read to the respondent or given to them on the clipboard Best to administer to an informant but can also be given to the resident Respondent rates changes in the resident Rate as Yes a change , No change or don t know Add the total number of yes a change . 0 1: Normal cognition 2 or greater: Cognitive impairment is likely to be present Adapted from Galvin JE et al, The AD8, a brief informant interview to detect dementia
Cognitive Disability Model (Allen, 1985) Performance of activities in a safe and efficient way is influenced by the information processing ability of the individual Measures level of body functions Six cognitive level scales Leather lacing person asked to replicate 3 different stitches of increasing complexity with variations in the level of instruction to determine cognitive level/deficits Placemat replicates simple design on placemat Marum
Allen one can predict the ability to perform an ADL independently by using the cognitive levels as assessed by the ACLS Standardized, reliable and valid Provides quick estimate of the level of assistance required to perform both routine and new or unusual task Allen suggests that the ability to adjust to physical disability is dependent upon cognitive level
Receive, Process and Comprehend, Respond AD impacts ability to communicate Expressive: damage to key language areas hinders the expression of language Dysnomia Word substitutions Dysfluency, halting speech Word Salad Receptive: Fails to understand all or part of what is said or demonstrated
Fatigue Changes in routine, environment, caregiver Demands exceed functional skills Multiple / competing stimuli Responses to perceived loss of control Physical stress: Pain, medication, etc.
Unable to understand / follow instructions Cannot report pain, symptoms, needs Cannot ask for help Compromised capacity for relationships with caregivers Delayed response
Attention one item / idea at a time Executive - simple, 1 2 step tasks Orientation may not recognize familiar places Language simple, direct language Wait for a response up to 10 seconds
Words account for 7% of communication Tone of voice accounts for 38% of communication Body language accounts for 55% of communication
Approach slowly with open posture and a smile. Avoid standing over the person. Identify yourself (even if they have met you before) and call them an acceptable name Use touch only when there is clear recognition of your presence and identity Speak slowly and clearly Only raise your voice when necessary for hearing
Stick to your core message Take your time Keep sentences short and to the point Use physical gestures to promote comprehension when possible Don t just rephrase yourself or put words in the client s mouth
Your name and function I ve come to see how you are I need your advice I need your help What do you think I was wondering Could we do this together
Make eye contact Address your remarks to the resident When family members or caregivers are present, keep your open posture towards the resident Validate the resident s perspective, even if you don t agree Its OK to apologize for your lack of understanding so as to maintain positive rapport
residents with dementia deserve respect residents may be limited in their ability to understand Involve the family / caregivers when possible Validate the resident s feelings Ask about family / caregiver s feelings
Behavior may sometimes be inappropriate Most behaviors are a nuisance but not a problem Provide unconditional, positive regard Remain non-judgmental about appropriateness of behavior Intervene if the behavior poses threats to safety Try to identify the trigger or cause
Physical discomfort Overstimulation Unfamiliar surroundings Complicated tasks Frustrating interactions (Inability to communicate effectively) Fear or uncertainty Touch or invasion of personal space Lack of attention to needs / wishes
Anger / agitation Sleep problems Paranoia / delusions Resistance to ADLs Inappropriate social / sexual behavior Sundowning Repetitive Actions Rummaging Wandering / looking for people / home Crying out loud Incoherent verbalizations
Inclusion Attachment Occupation Comfort Love Identity Address Physical Needs Psychosocial Needs Environment
Step into their reality Re-direct Participate in activities Watch how family members approach and model if effective Use effective communication Simplify tasks Try to follow their routine Adapt the environment
Validate their feelings I understand that you miss your mom. Tell me something about your mom. Validate the person s reality of what is happening Your mom is probably shopping (or at home doing laundry, etc.)
Focus their attention away from the situation Use food, conversation, alternative activity Engage the person to share their social history Encourage participation in activity
Stay calm Assess person s emotional state Build rapport Do not try to reason Watch your non-verbal communication Give them space and try again later
Keep the resident calm Manage agitation Prevent wandering / elopement Accommodate need to explore Prevent / reduce falls Promote function Meet needs
May be triggered by: Delirium Disturbed Sleep Acute Illness (UTI) Medications Pain Impaired Sensory system
Wants to go home Stressed / anxious / in pain Related to previous lifestyle Looking for security, something familiar
Look for wandering patterns / talk with family Identify residents that are at risk for wandering Keep resident s purse, suitcase, coat, etc. out of sight Ask family to bring in comfort items from home Keep resident in room that is away from the exit and in view of others Assess for pain, keep resident warm Use distraction
Dementia / confusion Decreased mobility Recent weight loss Chewing or swallowing problems Poorly fitting dentures Arthritis Depression Lack of understanding of diet restrictions
Different eating patterns Crave sweets Confusion regarding utensils Drug interactions Fatigue
Common in persons with Parkinsons, CVA, dementia Swallowing rate slows Medications may suppress cough In later stages of AD, the person may pocket food, forget to swallow
Assess self-feeding ability Use appropriate diet consistency based on Speech Therapy recommendations Partner with family regarding food preferences Provide small / frequent meals Consider finger food diet Cut food into appropriate size Present one item at a time Bring to table only when food is served
Mirroring Multi-sensory cueing Hand over hand assist Opening mouth Simplify tray Reduce noise / clutter
Upright position Proper head position (i.e. chin tuck, etc.) Avoid eating in bed If resident must be fed in bed, raise HOB to 90 degrees Encourage sitting up for at least 30 minutes after meal Position food so resident can reach the tray Transfer into regular chair if possible