Appropriate Use Criteria for Lumbar Puncture in Alzheimer's Disease Diagnosis
Clinicians traditionally diagnose Alzheimer's Disease (AD) based on clinical criteria, but cerebrospinal fluid (CSF) AD biomarkers offer more reliable detection earlier in the disease course. This article discusses the criteria for lumbar puncture and CSF analysis in the diagnosis of AD, highlighting the importance of CSF biomarker testing in patient selection for treatment trials.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Appropriate Use Criteria for Lumbar Puncture and Cerebrospinal Fluid Analysis in the Diagnosis of Alzheimer s Disease Leslie M Shaw Department of Pathology & Laboratory Medicine Perelman School of Medicine, University of Pennsylvania
Introduction Traditionally clinicians have diagnosed AD using primarily clinical criteria CSF AD biomarkers are effective surrogates for neuropathology Their use provides for reliable detection of AD earlier in the disease course compared to clinical diagnosis alone Reliability of CSF AD biomarker testing for amyloid and tau proteins has advanced considerably within- and across platforms, increasing the likelihood of broad clinical use internationally including in USA where this is typically done in the research realm CSF biomarker testing has IVD status in some European countries: in routine clinical practice for patient selection in international treatment trials
Introduction An international Workgroup, convened by the Alzheimer s Association to: Assist healthcare practitioners with guidance-based on: evidence and the experience of the workgroup members, and ethical standards for patient care-on the Appropriate and Inappropriate use of LP and CSF AD biomarker testing to support optimal patient safety & care. Builds on the AUC for amyloid PET (Johnson, 2013, #5), these criteria are intended to support clinicians in consistently identifying appropriate patients for LP and CSF testing, while considering the cost-effective use of limited healthcare resources. It is hoped that these AUC will be an important resource for policy makers & 3rdparty payers These AUC do not: Provide recommendations for the research use of CSF biomarker testing Rule out conditions other than AD or MCI-AD as possible causes of cog decline Recommendations for the appropriate use of CSF are made in the context of the many other diagnostic tools in use.
Evidence discussion In Feb 2017 the Workgroup was convened by Alz Assn to develop these AUC Avalere Health provides technical & editorial assistance for this process Teleconference calls, biweekly, through December, 2017; FTF at the London AAIC meeting, July 2017 Members include 4 Neurologists, one Neuro-Ethicist, one Lab Medicine physician, one Path & Lab Medicine biomarker researcher Each member had considerable publications on topics relevant to the use of LP, including dementia research, biomarker test validation & clinical utilities, patient care & ethics The workgroup defined the scope & parameters of the AUC & key research questions to guide systematic review of published evidence on LP & CSF for AD diagnosis using the PICOTS (population, interventions, comparisons, outcomes, timing & settings) framework (Whitlock, #33) The Workgroup then developed a list of 14 clinical indications based on key patient groups that are encountered in clinical practice and in whom the use of LP and CSF may be considered as part of the diagnostic process.
AUC Workgroup Members Workgroup Member Affiliation Jalayne Arias University of California, San Francisco; Atlantic Fellow, Global Brain Health Institute Kaj Blennow Department of Psychiatry & Neurochemistry, University of Gothenberg, Sweden Maria Carrillo Alzheimer s Association, Chicago Douglas Galasko Department of Neuroscience, UCSD Jose Luis Molinuevo Barcelonabeta Brain Research Center, Barcelona, Spain Stephen Salloway Memory and Aging Program, Butler Hospital, Brown University Suzanne Schindler Department of Neurology, Washington University Leslie M Shaw; Chair Department of Pathology & Laboratory Medicine, University of Pennsylvania Responsible for the scope of evidence reviews & determination of Indications for CSF testing and vote on appropriateness or inappropriateness of the Indications. All declared conflicts of interest, if any, according to a written policy, developed by the Alzheimer s Association, and are included in the AUC document.
Five Key Research Questions(KQ1-5) Key Research Questions KQ#1 KQ#2 Safety of Lumbar Puncture in individuals undergoing evaluation for suspected AD What is the diagnostic accuracy In persons experiencing cog impairment of CSF A 42 & tau (t-tau, p-tau) or ratios of analytes as indicators of AD pathology presence or absence? In persons with little or no cognitive impairment, what is the diagnostic accuracy(sensitivity, specificity) of LP & CSF in assessing CSF amyloid(A 42) and tau levels or ratios as indicators of AD pathology presence or absence? What is the accuracy of CSF amyloid (A 42) and tau levels(t-tau, p-tau) or ratios of analytes for predicting progression from MCI to AD? Does the literature report rates of progression from MCI to AD (in individuals with MCI who are found to have amyloid and tau levels in high risk of AD ranges)? What are the effects of CSF testing for suspected AD on both clinical outcomes (diagnosis) and intermediate outcomes (e.g., management with medications)? KQ#3 KQ#4 KQ#5
KQ#1: KQ#1: Safety of Lumbar Puncture Safety of Lumbar Puncture CSF can be collected safely & reliably by LP Documented in >7,000 AD patients in 10 studies Consistent with documented safety record in >30,000 patients with a wide array of neurologic disorders Key to maximizing patient safety is recognition of Pt- & LP-related risk factors including: contraindications such as use of anticoagulant meds, recent seizures, blood clotting disorders, intracranial lesions, others Additional best practices to ensure LP safety: Use of atraumatic narrow bore needle-less risk for PLPH Avoidance of repeated attempts in difficult cases to reduce risk for lower back pain Avoidance of collection of >30 mL Fear of the LP procedure is an independent risk factor that can be influenced by the attitude of the clinical staff & can be decreased by providing sensitive, matter-of-fact, verbal communication about the procedure by clinicians familiar and comfortable with LP
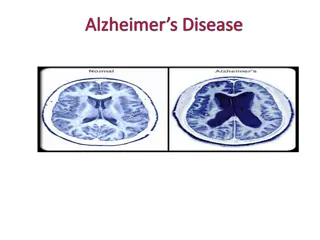
KQ#2 KQ#2: In persons experiencing cognitive impairment, what is the In persons experiencing cognitive impairment, what is the diagnostic accuracy diagnostic accuracy of LP & CSF A of LP & CSF A 42 & tau levels(t ratios as indicators of AD pathology presence or absence? ratios as indicators of AD pathology presence or absence? Assessment of accuracy of a test depends on the trueness of the reference standard the test is compared against. For many disease conditions, an accurate reference is not available & the assessment depends on expert clinical diagnosis or consensus clinical diagnosis. For AD, diagnostic accuracy based on clinical criteria is not optimal: sensitivity & specificity are ~80% & 70%, respectively, at expert centers. At earlier disease stages the accuracy is substantially lower eg, at the MCI stage: clinical symptoms overlap with those of other NDs co-pathologies add to the uncertainty. More objective detection of AD disease presence or absence is obtained using amyloid PET or neuropathologic evaluation Amyloid PET ligands have been approved by the FDA & EMA to identify/rule out brain amyloidosis based on validation against brain autopsy 19 studies using amyloid PET as reference standard were identified (N=3,697) There were 5 studies that used autopsy diagnosis as the reference standard (N=764) 42 & tau levels(t- -tau & p tau & p- -tau181) or tau181) or
KQ#2: KQ#2: In persons experiencing cognitive impairment, what is the In persons experiencing cognitive impairment, what is the diagnostic accuracy diagnostic accuracy of LP & CSF A of LP & CSF A 42 & tau levels(t ratios as indicators of AD pathology presence or absence? ratios as indicators of AD pathology presence or absence? 42 & tau levels(t- -tau & p tau & p- -tau181) or tau181) or Sensitivity & specificity; Area-Under-ROC CURVE(AUC) across the studies: 88-93% & 84-85%; AUC= 0.90-0.93, 96% & 88-91%; AUC=0.93-0.96, 92.1 & 86.3; 91.1 & 89.8; for A 42 alone for A 42/A 40 for t-tau/A 42 for p-tau181/A 42 [N=1,453] [N=3,094] [N=515] [N=1,526] AUC=0.95 AUC=0.96
KQ#3 KQ#3: : In persons with little of no cognitive impairment, what is the diagnostic In persons with little of no cognitive impairment, what is the diagnostic accuracy(sensitivity, specificity) of LP & CSF in assessing CSF amyloid(A accuracy(sensitivity, specificity) of LP & CSF in assessing CSF amyloid(A 42) and tau levels or ratios as indicators of AD pathology presence or absence? tau levels or ratios as indicators of AD pathology presence or absence? 42) and Accuracy for detection of AD presence or absence in persons with little or no cognitive impairment is comparable to that described in KQ2, although in a smaller number of study subjects
KQ#4: KQ#4: What is the accuracy of CSF amyloid (A What is the accuracy of CSF amyloid (A 42) and tau levels(t analytes analytes for predicting progression from MCI to AD? Does the literature report rates of for predicting progression from MCI to AD? Does the literature report rates of progression from MCI to AD (in individuals with MCI who are found to have amyloid and progression from MCI to AD (in individuals with MCI who are found to have amyloid and tau levels in high risk of AD ranges)? tau levels in high risk of AD ranges)? 42) and tau levels(t- -tau, p tau, p- -tau) or ratios of tau) or ratios of When MCI is associated with AD pathology based on positive AD biomarkers, the risk for progression to a clinical diagnosis of AD dementia is higher than when CSF A 42 and tau biomarkers are normal. Conversely, individuals whose CSF A 42 and tau biomarkers are non-pathologic have a high likelihood of remaining free from AD dementia over the time of observation, up to 10 years thus far. The wide range of specificity values across studies that document predictive performance of these CSF biomarkers likely due to: Differences in longitudinal observation time ranging from 1 to 10+ years from time of MCI diagnosis to the time limit of the study Patient age and disease heterogeneity likely impact rates of progression in an individual patient Prolonged follow-up studies for at least 5 years, and ideally longer, are needed to provide robust estimates of predictive performance in clinical practice.
KQ#5: KQ#5: What intermediate outcomes? intermediate outcomes? No study reports on the effects of CSF testing on clinical outcomes or use of medications What are the effects of are the effects of CSF CSF testing for suspected AD on clinical and testing for suspected AD on clinical and Further studies across diverse patient populations are required to more fully document impact of CSF AD biomarker test results on diagnostic decision making and effects on patient outcomes. Rating of clinical indications: - Score of 7 to 9, Appropriate - Score of 4 to 6, Uncertain - Score of 1 to 3, Inappropriate When an indication received all seven Workgroup members ratings in a single category of Appropriate, Uncertain, or Inappropriate, that indication was considered to have reached consensus rating.
# Indication Ratings 1 Cognitively unimpaired and within normal range functioning for age as established by objective testing; no conditions suggesting high risk and no subjective cognitive decline or expressed concern about developing Alzheimer s disease. Inappropriate 2 Cognitively unimpaired patient based on objective testing, but considered by patient, family informant, and/or clinician to be at risk for AD based on family history Inappropriate 3 Patients with subjective cognitive decline (cognitively unimpaired based on objective testing) who are considered to be at increased risk for AD Appropriate 4 Patients with subjective cognitive decline (cognitively unimpaired based on objective testing) who are not considered to be at increased risk for AD Inappropriate 5 Mild cognitive impairment that is persistent, progressing, and unexplained Appropriate 6 Patients with symptoms that suggest possible AD Appropriate 7 Mild cognitive impairment or dementia with an onset at an early age (<65) Appropriate 8 Meeting core clinical criteria for probable Alzheimer s disease with typical age of onset Appropriate 9 Symptoms of REM sleep behavior disorder Inappropriate 10 Patients whose dominant symptom is a change in behavior (e.g., Capgras Syndrome, paranoid delusions, unexplained delirium, combative symptoms, and depression) indication and where Alzheimer s disease diagnosis is being considered Appropriate 11 Use to determine disease severity in patients having already received a diagnosis of Alzheimer s disease Inappropriate 12 Individuals who are APOE 4 carriers with no cognitive impairment Inappropriate 13 Use of LP in lieu of genotyping for suspected autosomal dominant mutation carriers Inappropriate 14 Autosomal dominant mutation carriers, with or without symptoms Inappropriate
Clinical Indications for Appropriate Use of LP in the Diagnosis of AD and MCI Clinical Indications for Appropriate Use of LP in the Diagnosis of AD and MCI- -AD AD Rating of the clinical indications: # Indication Ratings Cognitively unimpaired and within normal range functioning for age as established by objective testing; no conditions suggesting high risk and no subjective cognitive decline or expressed concern about developing Alzheimer s disease. Inappropriate 1 Cognitively unimpaired patient based on objective testing, but considered by patient, family informant, and/or clinician to be at risk for AD based on family history Inappropriate 2 Patients with subjective cognitive decline (cognitively unimpaired based on objective testing) who are considered to be at increased risk for AD Appropriate 3 Patients with subjective cognitive decline (cognitively unimpaired based on objective testing) who are not considered to be at increased risk for AD Inappropriate 4
Clinical Indications for Appropriate Use of LP in the Diagnosis of AD and MCI Clinical Indications for Appropriate Use of LP in the Diagnosis of AD and MCI- -AD AD # Indication Ratings Appropriate Mild cognitive impairment that is persistent, progressing, and unexplained 5 Appropriate Patients with symptoms that suggest possible AD 6 Appropriate Mild cognitive impairment or dementia with an onset at an early age (<65) 7 Appropriate 8 Meeting core clinical criteria for probable Alzheimer s disease with typical age of onset Inappropriate Symptoms of REM sleep behavior disorder 9
Clinical Indications for Appropriate Use of LP in the Diagnosis of AD and MCI Clinical Indications for Appropriate Use of LP in the Diagnosis of AD and MCI- -AD AD # Indications Ratings Patients whose dominant symptom is a change in behavior (e.g., Capgras Syndrome, paranoid delusions, unexplained delirium, combative symptoms, and depression) indication and where Alzheimer s disease diagnosis is being considered Appropriate 10 Use to determine disease severity in patients having already received a diagnosis of Alzheimer s disease Inappropriate 11 Inappropriate Individuals who are APOE 4 carriers with no cognitive impairment 12 Inappropriate Use of LP in lieu of genotyping for suspected autosomal dominant mutation carriers 13 Inappropriate Autosomal dominant mutation carriers, with or without symptoms 14
Implementation of these AUC Discussion of appropriateness or inappropriateness of Indications intended to: assist dementia experts on decisions regarding testing and assist primary or other providers in determining when to refer to a dementia expert for more specialized testing. Workgroup(WG) described 6 clinical Indications where CSF biomarker testing is believed to be appropriate; these are largely consistent with those proposed by the PET amyloid imaging AUC: WG recommends Appropriate for CSF biomarker testing for pts. With progressive & unexplained MCI Pts with possible AD where co-morbidities often make diagnosis uncertain In cases with early onset (<65 yrs) MCI and dementia WG also describes 3 appropriate Indications that differ from the AUC for amyloid PET: Pts meeting core clinical criteria for probable AD with typical age of onset Individuals experiencing SCD but who score within normal range on cog. Testing & considered to be at increased risk for AD o The following features are associated with increased risk in an individual with SCD: persistent decline in memory rather than other cognitive domains; onset in the last 5 years; age at onset > 60 years; concerns (worries) associated with SCD; feeling of worse performance than others of the same age group and confirmation of cognitive decline by an informant and presence of the APOE 4 genotype. Pts whose dominant symptom is a change in behavior & where an AD diagnosis is being considered. We adopt the recommendation that CSF testing should be conducted by dementia experts.
Further research questions Studies using next-generation CSF biomarker assays will have less center to center variability, together with large sets of comparisons to amyloid PET & autopsy brain examination: More precise sensitivity/specificity, more consistent cut-points and gray-zones around them Optimization of pre-analytical factors is a key requirement to achieve the above Further studies of ratios in comparison to A 42 alone are warranted Candidate new biomarkers Long-term follow-up with CSF biomarker positive and negative needed Studies to determine added value of CSF biomarkers analogous to the amyloid PET IDEAS study Acceptability of LP in diverse settings Estimations of risks of future cognitive decline in persons who test positive needed as prevention trials for AD are pursued.