Tuberculosis as a Risk Factor for Viral Non-Suppression in Patients Switched to Dolutegravir-Based Therapy
The study investigates the impact of incident tuberculosis on viral non-suppression among patients transitioning to Dolutegravir-based therapy in Zambia. It aims to identify factors associated with viral non-suppression and describe clinical outcomes in the context of tuberculosis occurrence. The research explores the relationship between tuberculosis and treatment outcomes, shedding light on challenges in managing HIV/AIDS in resource-constrained settings.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
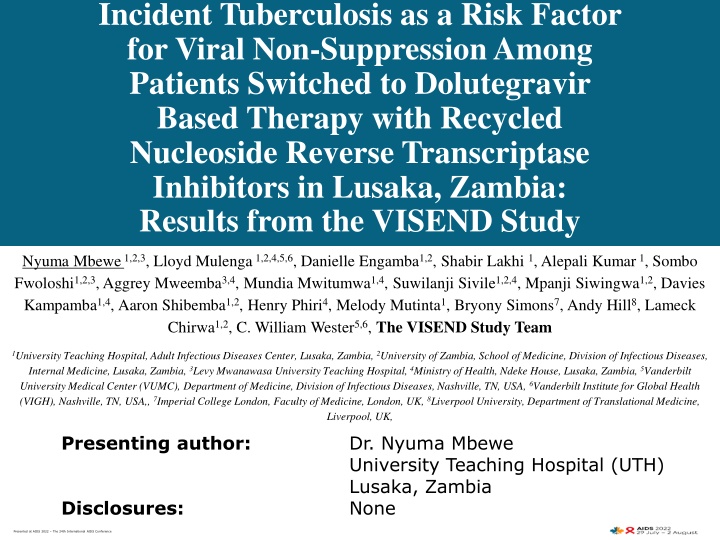
Incident Tuberculosis as a Risk Factor for Viral Non-Suppression Among Patients Switched to Dolutegravir Based Therapy with Recycled Nucleoside Reverse Transcriptase Inhibitors in Lusaka, Zambia: Results from the VISEND Study Nyuma Mbewe 1,2,3, Lloyd Mulenga 1,2,4,5,6, Danielle Engamba1,2, Shabir Lakhi 1, Alepali Kumar 1, Sombo Fwoloshi1,2,3, Aggrey Mweemba3,4, Mundia Mwitumwa1,4, Suwilanji Sivile1,2,4, Mpanji Siwingwa1,2, Davies Kampamba1,4, Aaron Shibemba1,2, Henry Phiri4, Melody Mutinta1, Bryony Simons7, Andy Hill8, Lameck Chirwa1,2, C. William Wester5,6, The VISEND Study Team 1University Teaching Hospital, Adult Infectious Diseases Center, Lusaka, Zambia, 2University of Zambia, School of Medicine, Division of Infectious Diseases, Internal Medicine, Lusaka, Zambia, 3Levy Mwanawasa University Teaching Hospital, 4Ministry of Health, Ndeke House, Lusaka, Zambia, 5Vanderbilt University Medical Center (VUMC), Department of Medicine, Division of Infectious Diseases, Nashville, TN, USA, 6Vanderbilt Institute for Global Health (VIGH), Nashville, TN, USA,, 7Imperial College London, Faculty of Medicine, London, UK, 8Liverpool University, Department of Translational Medicine, Liverpool, UK, Presenting author: Disclosures: Dr. Nyuma Mbewe University Teaching Hospital (UTH) Lusaka, Zambia None Presented at AIDS 2022 The 24th International AIDS Conference
Background There is a growing body of evidence on the utility of Dolutegravir (DTG)- based therapy in resource-constrained settings with the use of recycled nucleoside reverse transcriptase inhibitors1 Concerns remain for the emergence of DTG resistant virus with factors such as suboptimal adherence, non-B subtypes, and drug-drug interactions2 Concerns also for occurrence of tuberculosis (TB) associated IRIS with widespread use of integrase strand transfer inhibitors3 o More rapid HIV-1 RNA (viral) suppression and CD4 cell count recovery 1 Paton 2022 NEJM (NADIA) 2. Mahomed, K. et al. (2020) Southern African Journal of HIV Medicine 3. Wijting, I. et al. (2016) 16th European AIDS Conference. Presented at AIDS 2022 The 24th International AIDS Conference
Study Objectives Primary Objective Describe factors associated with viral non-suppression at 48 weeks in patients with a baseline viral load > 1,000 copies/mL when switched from Tenofovir disoproxil fumarate (TDF)/Lamivudine (3TC)/Efavirenz (EFV) to Dolutegravir-based therapy with recycled NRTIs or to standard boosted Protease Inhibitor-containing 2nd line regimen. Secondary Objectives: To characterise incident TB cases among patients in this study cohort. To determine the time to event for clinical manifestations of TB from the time of regimen switch. To describe the clinical outcomes of patients who develop incident TB. Presented at AIDS 2022 The 24th International AIDS Conference
Methodology Sub-study of the 144-week randomised, open-label, noninferiority study in Zambia: A1: TLD (n=209) Arm A (<1,000 cp/mL) A2: TAFED (n=209) n = 1,201 Participants B1a: TLD (n=208) B1b: TAFED (n=211) Arm B ( 1,000 cp/mL) B2a: AZT/3TC+LPVr (n=167) B2b: AZT/3TC+ATVr (n=197) Treatment experienced PLHIV >18 years of age on TDF/XTC/EFV (NVP) for more than 6 months randomized to TDF/3TC/DTG (TLD), TAF/FTC/DTG (TAFED), AZT/3TC/boosted LPV/r (boosted ATV/r). Participants screened (clinical, bacteriologic, radiographic) for active TB at baseline and visits at week 12, 24, 48, 72, 96, and 144. Relevant covariates collected during each study visit. Presented at AIDS 2022 The 24th International AIDS Conference
Table 1: Baseline Characteristics of Arm B Study Participants PI-Based Second line AZT/3TC/LPV-r or ATV-r (n=364) DTG-Based TLD or TAFED (n=419) n (%) n (%) Baseline CD4 cell count (cells/mm3) < 50 50 200 > 200 Sex Male Female Age (years of age), mean (SD) < 20 20 60 >60 Systolic blood pressure (SBP), mean (SD) Employment Working Full Time Working Part time Working Occasionally Full-time student Not working because of ill/poor health Not working / unemployed Duration of previous ART (years), mean (SD) Baseline Laboratory parameters Hemoglobin (gr/dL) White Blood Count (WBC) count, (x 109/L) Alanine transaminase (AST) (IU/L) Creatinine (umol/L) Body Mass Index (BMI) (kg/m2) Viral Load (HIV-1 RNA) (copies/mL) 1 (0.3) 63 (20) 251 (79.6) 1 (0.24) 67 (16.2) 345 (83.5) 138 (37.9) 226 (62.1) 37.4 (9.8) 16 (4.4) 339 (94.2) 5 (1.4) 123.5 (19.8) 162 (3.7) 257 (61.3) 38.4(10.6) 20 (4.8) 387 (93.3) 8 (1.9) 124.0 (20.4) 152 (56.3) 8 (3.0) 5 (1.9) 8 (3.0) 4 (1.5) 93 (34.4) 5.6 (4.4) 170 (48.6) 8 (2.3) 4 (1.1) 12 (3.4) 0 (0.0) 156 (44.6) 6.2 (4.3) 12.9 (2.1) 4.4 (1.4) 65.2 (20.3) 25.8 (24.2) 22.9 (4.6) 210,062.5 (630822.1) 12.8 (2.5) 4.5 (2.0) 60.3 (17.3) 22.9 (12.6) 22.2 (4.6) 100,569.1 (219459.6) Presented at AIDS 2022 The 24th International AIDS Conference
Table 2: Factors Associated with Viral Non-Suppression on DTG- based Therapy (Arms B1a+B1b) Crude Odds Ratio Adjusted Odds Ratio (aOR) p-value 95% CI p-value 95% CI Age (years) < 20 years 20-59 years of age Sex Male Female 1 1 2.78 0.049 1.00 -7.75 3.44 0.021 1.20-9.86 1 1.91 0.03 1.07-3.42 CD4 cell count (cells/mm3) 1 1 < 50 cells/mm3 50 200 cells/mm3 9.73 0.004 2.03-46.7 8.32 0.012 1.58-44.7 > 200 cells/mm3 21.6 <0.001 4.59-102.1 18.43 3.57-95.3 0.001 Body mass index (BMI) (kg/m2) Underweight (< 18.5) Normal (18.5 25) 1 1.46 0.343 0.67-3.21 Overweight (25-30) 2.42 0.129 0.77-7.56 Obese (> 30) Tuberculosis No Yes Hemoglobin (8.5 gm/dL) 3.05 0.106 0.79-11.77 1 1 0.32 0.90 0.03 0.04 0.11-0.89 0.81-1.00 0.33 0.045 0.11-0.97 0.93 0.24 0.82-1.05 White blood cell count (x 109/L) 0.93 0.097 0.86-1.01 Creatinine (umol/L) 1.004 0.51 0.99-1.02 Presented at AIDS 2022 The 24th International AIDS Conference
Characteristics of Incident TB Cases Incident TB: 3 incident TB cases in Arm A vs. 32 incident TB cases in Arm B 14 (3.3%) of 419 patients receiving DTG-based therapy (Arms B1a + B1b) 18 (4.9%) of 364 patients receiving PI-based therapy (Arms B2a + B2b) Viral Suppression: Viral suppression rates (48 weeks) by Treatment Arm (reported previously) 94% among patients receiving DTG-based therapy vs. 87% among patients receiving boosted PI therapy Viral Non-Suppression: 6% among patients receiving DTG-based therapy vs. 13% among patients receiving boosted PI therapy had viral loads greater than 1000 copies/mL at week 48 2 (9.5%) of 21 non-suppressed patients on boosted PI arm had incident TB 3 (11%) of 27 non-suppressed patients on DTG-based arm had incident TB - This included one case of extra-pulmonary TB (TB meningitis) hence prolonged course of ATT Mortality: Four patients during the trial died by week 48 3 (75%) of these 4 deaths were attributed to TB Presented at AIDS 2022 The 24th International AIDS Conference
Time to TB Event Presented at AIDS 2022 The 24th International AIDS Conference
Characteristics of TB Cases2 Death TB treatment completed Previous TB Total cases 0 2 4 6 8 10 12 14 16 18 20 DTG based PI based Presented at AIDS 2022 The 24th International AIDS Conference
Discussion In western countries, low occurrence of IRIS but low TB burden and excluded advanced HIV disease3,4 African cohorts saw no difference in virological suppression and TB outcomes5,6 Occurrence of TB in patients on DTG-based therapy is concerning for the possibility of emergent DTG resistance2,7 Strengths: o Largest cohort of patients with recycled NRTI on DTG Limitations: o Unable to characterize IRIS and no drug levels measured to be assured of adherence o Not all TB was microbiologically confirmed 3. Wijting, I et al 2017 European AIDS Conference 4. Hill, A. et al. (2017) Current Opinion in HIV and AIDS 5. Modongo, C. et al. (2019) JAIDS 6. Dooley, E. et al (2020) CID 7. Oosterhout, J. et al. (2022) Presented at AIDS 2022 The 24th International AIDS Conference
Conclusions & Recommendations Conclusions 4% of the total study cohort developed incident TB by 48 weeks, with a significant mortality rate (12.5%) including one case of extrapulmonary (CNS TB) Most of the cases of TB manifested in the first three months post transition Recommendations Encourage thorough screening for TB among patients being transitioned to TLD/TAFED with recycled NRTIs ? Need to routinely perform urinary LAM testing or computer aided detection (CAD) at time of regimen switch in all patients Availability of alternative regimens, e.g., Rifabutin PK studies for TAFED with Rifampicin needed Presented at AIDS 2022 The 24th International AIDS Conference
References 1. Paton NI, et al. (2021) Dolutegravir or Darunavir in Combination with Zidovudine or Tenofovir to Treat HIV ,New England Journal of Medicine (NEJM), 385(4), 330 341. doi: 10.1056/nejmoa2101609. Mahomed K, et. al. Case report: Emergence of dolutegravir resistance in a patient on second- line antiretroviral therapy. South African Journal of HIV Medicine. 2020;21(1), a1062. https://doi.org/10.4102/ sajhivmed.v21i1.1062. Wijting IEA, Wit FWNM, Rokx C, et al. Use of integrase inhibitors is an independent risk factor for immune reconstitution inflammatory syndrome (IRIS) in HIV-1 late presenters: an ATHENA cohort study. In 16th European AIDS Conference, Milan, Italy 2017; 25: 313s. Hill AM, et al. (2017). Risks of cardiovascular or central nervous system adverse events and immune reconstitution inflammatory syndrome, for dolutegravir versus other antiretrovirals. Current Opinion in HIV and doi:10.1097/COH.0000000000000445 Modongo C., et al. (2019) Clinical and Virological Outcomes of TB/HIV Coinfected Patients Treated with Dolutegravir-Based HIV Antiretroviral Regimens: Programmatic Experience from Botswana. Journal of Acquired Immune Deficiency Syndromes, 82(2), 111 115. doi: 10.1097/QAI.0000000000002126. Dooley, KE. et al (2020) Dolutegravir-based Antiretroviral Therapy for Patients Coinfected With Tuberculosis and Human Immunodeficiency Virus: A Multi-Center, Non-comparative, Open-label, Randomized Trial. Clinical Infectious Diseases. 2020 Feb 3;70(4):549-556.doi: 10.1093/cid/ciz256. Oosterhout J., et al. (2022) Dolutegravir Resistance in Malawi s National HIV Treatment Program Open Forum Infectious Diseases. doi.org/10.1093/ofid/ofac148. Downloaded from https://academic.oup.com/ofid/article/9/5/ofac148/6563877 by guest on 22 June 2022. 2. 3. 4. AIDS. 2018 Mar;13(2):102-111. 5. 6. 7. Presented at AIDS 2022 The 24th International AIDS Conference
Acknowledgements - All the study participants - Viatris (Mylan) Laboratories, Limited and the Zambian Ministry of Health through the Global Fund to Fight AIDS, Tuberculosis and Malaria (GFATM) (Study Sponsors)