Respiratory Care in FSHD: Guidelines and Management Overview
Comprehensive overview of respiratory care in Facioscapulohumeral Muscular Dystrophy (FSHD) based on the American Academy of Neurology guidelines. Covers incidence of respiratory insufficiency, assessment of lung function, treatment options including noninvasive ventilation, and strategies for maintaining lung health. Emphasis on the association of respiratory insufficiency with factors like scoliosis, obesity, muscle weakness, and comorbidities. Details on pulmonary assessment, sleep disordered breathing causes, and symptoms. Essential information for healthcare professionals and individuals affected by FSHD.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
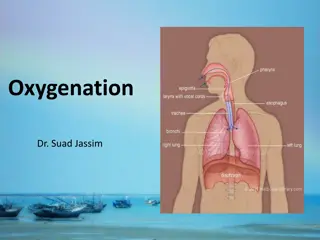
Respiratory Care in FSHD Lee Guion MA, RRT, FAARC FSHD Family Day Conference July 15, 2017
Respiratory Care in FSHD: Overview American Academy of Neurology Guidelines (2015) Incidence of respiratory insufficiency in FSHD Assessment of lung function (recommendations) Treatment/management options (2015 AAN) Chronic nocturnal respiratory insufficiency Noninvasive bi-level positive pressure ventilation (NIV) Acute respiratory failure (2017 ERS/ATS) Noninvasive bi-level positive pressure ventilation (NIV) Strategies for lung health (2017 LRG) 7 Steps to healthy lungs
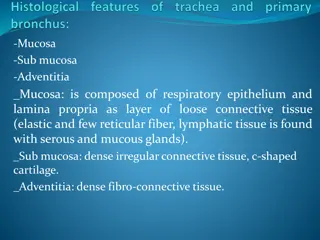
Respiratory Care in FSHD American Academy of Neurology Guidelines (2015) Systematic review of medical literature focused exclusively on FSHD by panel of clinicians with FSHD expertise following AAN process (quality of research) Respiratory abnormalities Decreased lung function Daytime symptoms of nocturnal hypoventilation Frequency of respiratory insufficiency 1.25% - 13% Severity also difficult to estimate
Respiratory Care in FSHD American Academy of Neurology Guidelines (2015) Respiratory insufficiency associated with: Scoliosis or kyphoscoliosis Obesity with abdominal distension Severe proximal weakness Wheelchair dependence Co-morbidities: chronic pulmonary or cardiac disease Respiratory muscle weakness (diaphragm)
Respiratory Care in FSHD American Academy of Neurology Guidelines (2015) Pulmonary assessment Baseline spirometry on ALL patients Monitor routinely if abnormal or with Spinal abnormalities (scoliosis/kyphoscoliosis) Decreased mobility or inability to ambulate Lung or heart disease Reported daytime symptoms of sleep disordered breathing
Respiratory Care in FSHD American Academy of Neurology Guidelines (2015) Sleep disordered breathing (SDB) Causes Weakened breathing muscles shallow breathing increased carbon dioxide/decreased oxygen fragmented sleep decreased REM sleep Symptoms Awakening unrefreshed Feeling sleepy during the day and needing naps Frequent nocturnal arousals Morning headaches
Respiratory Care in FSHD American Academy of Neurology Guidelines (2015) Recommendations for respiratory insufficiency (FVC <60% of predicted) or reported symptoms of SDB Referral to pulmonologist or sleep medicine specialist Treatment with noninvasive positive pressure ventilation (NIV) at night to rest lung muscles during the day if needed
Respiratory Care in FSHD Recommendations for acute hypercarbic ( CO2) or hypoxemic ( O2) respiratory failure Noninvasive ventilation (NIV) (European Respiratory Society/American Thoracic Society Guidelines 2017) Recommendations for extubation and preventing reintubation Noninvasive ventilation (NIV) (American Thoracic Society/American College of Chest Physicians Guidelines 2017)
Respiratory Care in FSHD Lee s 7 steps to lung health STEP 1 Attend a multidisciplinary muscular dystrophy clinic Consistent, coordinated, integrated, compassionate care One stop shop Neurologist, RT, PT, OT, SW, representatives from support organizations (MDA) Research participation opportunities
Respiratory Care in FSHD STEP 2 Vaccinations Pneumococcal polysaccharide pneumonia vaccine (PPSV23 Pneumovax) Pneumococcal conjugate vaccine (PCV13 Prevnar) Annual influenza vaccine (you and family members) Avoid infective agents (hand washing, distance, masks) Practice good oral hygiene. Get recommendations for adaptations from OT if brushing/flossing is difficult
Respiratory Care in FSHD STEP 3 Treat symptoms of upper respiratory tract infection and seasonal rhinitis (to help reduce chances of lower airway infection) Learn about early detection of lower respiratory tract infection (fever, malaise, prolonged lethargy) Seek medical attention early and do not delay
Respiratory Care in FSHD STEP 4 Good hydration Maintain healthy electrolyte balance Positive and negative ion exchange (largely sodium and chloride) will assist with normal mucus production, natural mucosal reabsorption and removal of lower respiratory tract secretions
Respiratory Care in FSHD STEP 5 Maximize nutrition Malnutrition increases risk of infection (immunosuppression) Increased work of breathing/increased respiratory rate = more calories/energy consumed by breathing Nutritional supplements if recommended Smaller, more frequent meals Consult nutritionist
Respiratory Care in FSHD STEP 6 Movement and Safe Exercise Stretching (reduces stiffness, improves circulation) Moderation (do not overwork muscles, rest weak muscles) Coordinate exercise/movement with breath work Benefits Increases blood neutrophil counts and Helps maintain lymphocyte counts to improve immune function and response to infection Improves gas exchange (oxygen/carbon dioxide) Psychological/emotional benefits
Respiratory Care in FSHD STEP 7 Get a good night s sleep Quantity (aim for 8 to 9 hours) Quality (restorative sleep) Awakening refreshed Ability to be alert throughout the day Address barriers to sleep Shallow breathing and drops in oxygen Pain or discomfort Difficulty repositioning Worry and intrusive thoughts
Respiratory Care in FSHD Thank You! guionlr@gmail.com Neurology Evidence-based guideline summary: Evaluation, diagnosis, and management of