Physiology: The Body as an Organized Solution
Physiology is the science of living organisms and their functions, exploring the intricate processes within the body. It delves into the importance of body fluid balance, cell function, and the vital role of water. Understanding how the body is organized at a cellular level provides insights into maintaining health and well-being
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Physiology The Body as an Organized "Solution Lecture:1 Dr. Shaimaa Munther
Physiology The science that is concerned with the function of the living organism and its parts, and of the physical and chemical processes involved.
General Principles : The Body as an Organized "Solution The cells that make up the bodies of all but the simplest multicellular animals, exist in an "internal sea" of extracellular fluid (ECF) enclosed within the integument of the animal. The ECF is more dilute than present-day seawater, but its composition closely resembles that of the primordial oceans. From this fluid, the cells take up O2 and nutrients; into it, they discharge metabolic waste products
Water, (the primary body fluid) is the most important nutrient for life. 40-75% of human body weight is water. Loss of 10% body fluid = 8% weight loss SERIOUS Loss of 20% body fluid = 15% weight loss FATAL Fluid gained each day should = fluid lost each day (2 -3L/day average)
Functions of Body Fluid Medium for transport Needed for cellular metabolism Solvent for electrolytes and other constituents Helps maintain body temperature Helps digestion and elimination Acts as a lubricant
Body Fluid Compartments In lean adults, body fluids constitute 55% of female and 60% of male total body mass these divided into: Intracellular fluid (ICF) inside cells About 2/3 of body fluid Extracellular fluid (ECF) outside cells divided into : 1. Interstitial fluid ( fluid between cell) is 80% of ECF 2. Intravascular fluid (Plasma in blood )is 20% of ECF
During transfer on nutrients (chemicals) an average 24 liters of fluid moves out of plasma each day; 85% is reabsorbed & the remainder (4L) is the lymph fluid that accumulates At the capillary level have 2 separate forces at work: Hydrostatic pressure --- pushes fluid out of vessels Colloid osmotic pressure --- pushes fluid into vessels
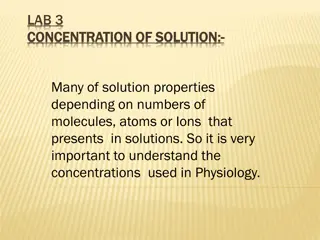
Composition of body fluids In addition to water, the body contains solutes; substances that separate in solution Solution = Solute + Solvent Solution = the fluid compartment (ICF or ECF) Solvent = water Solutes: Electrolytes Charged inorganic ions They dissolve in water They can conduct an electric current Major cations: ECF = sodium ICF = potassium Major anions: ECF = chloride, bicarbonate ICF = proteins neg charge Non-electrolytes Polar = those that are water soluble (sugars, proteins) Non-polar = those that are water insoluble (lipids)
Water Water (molecular formula H2O) is an essential part of all living organisms, making up 70% or more of the weight of most organisms. It consists of an oxygen atom connected to two hydrogen atoms by polar covalent bonds. It is considered to be the universal solvent for many reasons including its structural, chemical and physical properties. These properties result in the many unique characteristics of water.
Properties of water Very polar Oxygen is highly electronegative H-bond donor and acceptor High boiling point , melting point, heat of vaporization, surface tension
Polarity of Water In a water molecule two hydrogen atoms form single polar covalent bonds with an oxygen atom. Gives water more structure than other liquids Because oxygen is more electronegative, the region around oxygen has a partial negative charge. The region near the two hydrogen atoms has a partial positive charge. A water molecule is a polar molecule with opposite ends of the molecule with opposite charges.
Water dissolves polar compounds solvation shell or hydration shell
Hydrogen Bonding of Water Hydrogen bonds hold water molecules together. Each water molecule can form a maximum of 4 hydrogen bonds. The hydrogen bonds joining water molecules are weak, about 1/20thas strong as covalent bonds. They form, break, and reform with great frequency
Ionization of Water H20 + H20 H3O++ OH- H20 H+ + OH- [H+] [OH-] Keq = [H2O] -16M Keq=1.8 X 10 [H2O] = 55.5 M [H2O] Keq = [H+] [OH-] [H+] [OH-] = (1.8 X 10-16)(55.5 ) Kw =[H+] [OH-] = 1.0 X 10-14 If [H+] = [OH-] then [H+] = 1.0 X 10-7
Electrolytes Electrolytes are ions capable of carrying an electric charge. They are classified as anions or cations based on the type of charge they carry. CATIONS (+) ANIONS (-) (e.g, NaCl) are molecules that dissociate in water to their cation (Na+) and anion (Cl ) equivalents. Because of the net charge on water molecules, these electrolytes tend not to re associate in water. There are many important electrolytes in physiology, notably Na+, K+, Ca2+, Mg2+, Cl , and HCO3 . It is important to note that electrolytes and other charged compounds (eg, proteins) are unevenly distributed in the body fluids . These separations play an important role in physiology
Electrolytes Cations Anions Positively charged Negatively charged Sodium Na+ Potassium K+ Calcium Ca++ Magnesium Mg++ Chloride Cl- Phosphate PO4- Bicarbonate HCO3-
Electrolyte Functions Electrolytes are an essential component in numerous processes, including: Volume and osmotic regulation (Na, Cl & K) Myocardial rhythm and contractility (K, Mg & Ca2). Cofactors in enzyme activation (e.g., Mg, Ca). Regulation of adenosine triphosphatae, (ATPase) ion pumps (Mg) Acid-base balance (HCO3, K & Cl) Blood coagulation (Ca, Mg). Neuromuscular excitability (K, Ca, Mg). The production and use of ATP from glucose (Mg,PO4).
pH & The body Buffering System Buffers are compounds that resist changes in pH upon the addition of limited amounts of acids or bases. Buffer systems are usually composed of a weak acid or base and its conjugate salt. The components act in such a way that addition of an acid or base results in the formulation of a salt causing only a small change in pH. The maintenance of a stable hydrogen ion concentration ([H+]) in body fluids is essential to life. The pH of a solution is defined as the logarithm to the base 10 of the reciprocal of the H+ concentration ([H+]), ie, the negative logarithm of the [H+]. The pH of water at 25 C, in which H+ and OH ions are present in equal numbers, is 7.0
pH Scale Devised by Sorenson (1902) [H+] can range from 1M and 1 X 10-14M Using a log scale simplifies notation pH = -log [H+] Range is from 0 - 14 Neutral pH = 7.0 If [H+] is high, the solution is acidic; pH < 7 If [H+] is low, the solution is basic or alkaline ; pH > 7
In the plasma of healthy individuals, pH is slightly alkaline, maintained in the narrow range of 7.35 to 7.45. Conversely, gastric fluid pH can be quite acidic (on the order of 2.0) and pancreatic secretions can be quite alkaline (on the order of 8.0).
Weak Acids and Bases Equilibrium Molecules that act as H + donors in solution are considered acids, while those that tend to remove H+ from solutions are considered bases. Strong acids (eg, HCl) or bases (eg, NaOH) dissociate completely in water and thus can most change the [H+] in solution e. g. (HCl , NaOH). Weak acids / bases disassociate only partially e. g. (Acetic acid, Carbonic acid)
Acid/conjugate base pairs HA + H2O A-+ H3O+ HA A-+ H+ HA = acid ( donates H+) (Bronstad Acid) A-= Conjugate base (accepts H+) (Bronstad Base) Ka = [H+][A-] [HA] pKa = - log Ka Ka& pKavalue describe tendency to loose H+ large Ka= stronger acid small Ka= weaker acid
Henderson-Hassel bach Equation HA A-+ H+ HA = weak acid 1) Ka = [H+][A-] [HA] A- = Conjugate base 2) [H+] = Ka [HA] [A-] 3) - log [H+] = - log Ka - log [HA] * H-H equation describes the relationship between pH, pKa concentration [A-] and buffer 4) - log [H+] =- log Ka + log [A-] [HA] 5) pH =pKa + log [A-] [HA]
Similarly, the dissociation constant, or Kb value, of a weak base is given by the equation: and the buffer equation for weak bases, which is derived from this relationship, may be expressed as:
The Body Buffering System Enzymatic activity and protein structure are frequently sensitive to pH; in any given body or cellular compartment, pH is maintained to allow for maximal enzyme/protein efficiency. Body pH is stabilized by the buffering capacity of the body fluids. A buffer is a substance that has the ability to bind or release H+ in solution, thus keeping the pH of the solution relatively constant despite the addition of considerable quantities of acid or base. Of course there are a number of buffers at work in biological fluids at any given time. All buffer pairs in a homogenous solution are in equilibrium with the same [H+]; a great deal about all of the biological buffers in that system.
The Body Buffering System Normal acid-base balance is achieved through number of buffer systems : 1- Bicarbonate-carbonic acid buffer system 2- Phosphate buffer system 3- Protein buffer systems ( Amino acids & Hb )
Bicarbonate/Carbonic Acid Buffer Bicarbonate /Carbonic Acid Buffer is the most important buffering system in the body . Carbonic acid is a weak acid , that only partly dissociated into H and bicarbonate. A unique feature of bicarbonate is the linkage between its buffering ability and the ability of lung to remove carbon dioxide from the body. Bicarbonate Carbon dioxide Carbonic acid Excreted by lungs Excreted in urine
Maintenance of normal protein and electrolyte concentrations controls water distribution in the body compartments Water passes freely across cell membranes Ions and proteins cannot freely diffuse across most cell membranes Water moves passively in response to changes in solute concentration All monitors to homeostatic balance occur in ECF and not ICF Fluid shifts occur between ICF & ECF in response to changes only in ECF Key to equilibrium is maintaining solute concentration (osmolality ) 1. 2. 3. 4. Note: water follows salt ,thus, regulation of fluid balance & electrolyte balance are intertwined
Osmolality Osmolality is physical property of a solution that is based on the concentration of solute in term of miliosmoles per kilogram of solvent (w/w) & is the ability of that solution to cause osmosis between ICF & ECF. A low serum osmolality means a higher than usual amount of water in relation to the amount of particles dissolved in it ( over hydration or edema ) An increased serum osmolality indicate deficient fluid volume. Measurment of serum osmolality gives information about the hydration status within the cells because of the osmotic equilibrium that is constantly being maintained on either side of the cell membrane . If change to hypertonic ECF, then water into ECF If change to hypotonic ECF, then water into ICF
Movement of water between two compartments by a membrane permeable to water but not to solute Water moves from low solute to high solute concentration , requires no energy
Determining the osmolality is important because it indicates the water& electrolytes balance of the body. To determine the state of body water balance, one can measure plasma osmolality. Osmolality normal values Plasma : 275-295 mOsm/Kg 24 hour urine : 300-900 mOsm/Kg urine/serum ratio : 1.0-3.0 A solution that has HIGH osmolality is one that is > plasma osmolality = HYPERTONIC solution A solution that has LOW osmolality is one that is < plasma osmolality = HYPOTONIC solution A solution that has equal osmolality as plasma = ISOTONIC solution
Osmolality of ECF is controlled by : Hypothalams by osmoreceptor via : 1. Thirst Mechanism Regulation of vasopressin ( antidiuretic hormone ADH) The Kidney via the control of Na concentration & regulation of blood volume (Renin-angiotensin-aldosterone system) 2.
To maintain a normal plasma osmolality ( 275 295 mOsm/kg of plasma H2O), osmoreceptors in the hypothalamus respond quickly to small changes in osmolality. A 1% 2% increase in osmolality causes a fourfold increase in the circulating concentration of ADH, and a 1% 2% decrease in osmolality shuts off ADH production. ADH acts by increasing the reabsorption of water in the collecting tubules. glucose (mg/dl) BUN (mg/ dl) Osmolality = 2Na + + 18 2.8 BUN = Blood urea nitrogen
Normally, cells neither shrink or swell because intracellular and interstitial fluids have the same osmolality Increasing osmolality of interstitial fluid draws water out of cells and cells shrink Decreasing osmolality of interstitial fluid causes cells to swell
Hypotonic Isotonic Hypertonic