Pediatric Burn Patient Airway Management Overview
Understand the critical aspects of early intubation in pediatric burn patients, including challenges with facial and chest burns, appropriate airway placement strategies, respiratory compromise, and mechanical ventilation strategies for optimal outcomes. Explore a case study of a 4-year-old male with extensive burns and the importance of prompt intervention in such cases. Learn about the prevalence and mortality rates associated with burns in young children and the unique respiratory challenges circumferential burns pose. Anticipate difficult airways due to edema and thermal injury complicating the intubation process.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
G Nicole Sinclair, MD Pediatric Critical Care Medicine Covenant Healthcare
Understand the indications for early intubation in a burn patient Discuss the difficulties of intubation with facial, neck, and chest burns Examine the strategies for successful placement of an airway Understand the respiratory compromise in a burn patient Discuss mechanical ventilation strategies to improve ventilation and oxygenation
4 yo previously healthy male CC- Burns to face, neck, torso, and chest HPI-EMS was called to a residence after a child caught on fire after playing with a candle. He had visible burns to approx60% of his body surface area. He was drowsy with loud airway sounds. He was placed on a 100% NRB with sats in the low 90 s. He was brought to the community ER for management of his airway prior to transfer to burn center.
Vital signs-HR 150, RR-45, BP 100/60, sats 91% Neuro-GCS 10 (E3, V3, M4) Resp-Raspy, coarse BS with poor air exchange CV-Cool distally with delayed cap refill, tachycardic Skin-2ndand 3rddegree burns to face, neck, anterior, posterior chest, arms, and upper thighs
150,000 per year with 60,000 under the age of 5 Leading cause of death at home Maybe intentional vs accidental Mortality rates: Burns alone < 2% Smoke inhalation < 7% Burns + Smoke inhalation 29%
Circumferential burns to the thorax and abdomen Restriction of air movement and chest rise Tachypnea and hypoxemia Children are particularly susceptible due to their respiratory mechanics
Anticipate a difficult airway secondary to edema and direct thermal injury above the cords Laryngospasm/edema can occur rapidly and peak at 1-2 days If severe neck burn with contracture, cricoid pressure is difficult Chest burn can also lead to contracture and difficulty in bagging/ventilation
Leading cause of death, ~80% occur at the scene of the fire Mechanism of injury through: Thermal injury Asphyxiation Chemical irritants
Occurs via the combination of oxygen depletion, rising carbon monoxide and cyanide levels Less than 10% O2 in air leads to neurologic and physical impairment Cumulative effect with presence of CO and CN
Released during the combustion on any product Lethal level around 50%, can reach toxic levels (15-20%) within in 5 min of heavy smoke exposure Binds hemoglobin preferentially over oxygen shifting the hgb- O2 curve to the left (250- fold affinity)
Supplemental oxygen Hyperbaric oxygen for HgbCO> 25% Intubation when there is depressed mental status
Produced by the incomplete combustion of nitrogen containing products (carpets, insulation, furniture, appliances etc) Lethal serum levels > 3.0 mg/L, found in 70% of burn patients Binds to the cytochrome system causing uncoupling of OP in the mitochondria. This leads to profound tissue hypoxia and severe lactic acidosis
Supplemental oxygen Nitrates-form metHbwhich competes for cytochrome with CN, goal is 25-40% metHb Sodium thiosulfate-forms less toxic thiocyanate DicobaltEDT-binds CN Hydroxocobalamin-binds CN Intubation for severely depressed MS
Thermal occurs above the cords leading to upper airway edema>>>> laryngospasm and direct injury to the glottis Chemical below the cords leading to mucous membrane and alveolar damage, bronchospasm, surfactant deficiency, and ARDS
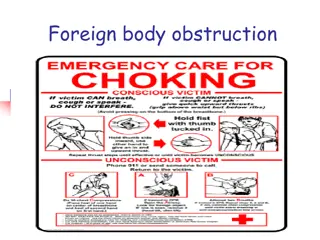
Attempt repositioning of airway Racemic epinephrine Heliox(if oxygen is not limiting) Secure upper airway with intubation if evidence of stridor, drooling, and obstruction No steroids Intubation usually short duration
Aerosols with albuterol and epinephrine High humidity, no passive humidifiers DNA aerosols? With intubation, frequent endotracheal lavage/suction Therapeutic bronchoscopies Typically longer intubation time
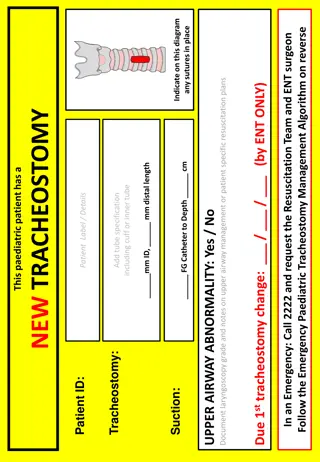
Glide scope at bedside Adequate sedation with a paralytic Cuffed and larger tubes for below the cord injury Uncuffedand smaller tube for above the cord injury Anesthesia present if substantial burns present Cric kit (if all else fails)
Ohnishi et al (2017) studied 205 burn patients, 80 were found to have inhalation injury and 34 were intubated They found that face/neck burns, TBSA affected (>27%), use of accessory muscles, and carboxyhemoglobinlevels were predictive of early intubation Singed nasal hair was not predictive
Lung protective ventilation with low tidal volumes (5-6 ml/kg), high PEEP, permissive hypercarbiahave been beneficial in treating ARDS secondary to chemical/SIRS lung injury Refractory hypoxia can be managed with HFOV ECMO has shown some survival benefit in patients that have failed maximal ventilator therapy