Airway Management in the NeuroICU: Importance and Strategies
Understanding the crucial role of airway management in the NeuroICU is essential for preventing secondary brain injury and addressing respiratory complications in neurologically-injured patients. This presentation covers the significance of airways, common issues, evaluation techniques, adjuncts, and pharmacological interventions. Neurological respiratory failure, ARDS, and non-neurologic complications in severe TBI patients are discussed to emphasize the need for comprehensive airway care. An overview of neural control and respiratory anatomy is provided to enhance clinicians' understanding of managing airways effectively in the critical care setting.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
AIRWAY MANAGEMENT IN THE ICU Rachel Garvin, MD Assistant Professor, Neurosurgery Neurocritical Care October 5, 2012
Goals of this Lecture To give you some comfort level with airways and tips to help your patient
Topics to be covered Why airway is so important Why patients with neurologic injury have airway issues Airway Anatomy Causes of compromised airway Airway Evaluation Airway Adjuncts Drugs
Why is airway management so important in the NeuroICU? Hypoxemia contributes to secondary brain injury Brain injured patients have numerous reasons to have airway compromise You should have an understanding of basic airway management to aid in your patient s care
Study by Rincon et al looked at ARDS/ALI in TBI Prevalence of 22% with mortality of 28% Significant increase in prevalence over the past 20 years More common in young white males
Neural control Corticobulbar tract Lower CN s Nucleus ambiguus Several respiratory centers Dorsal medulla Ventral medulla Dorsal rostral pons C-spine/Upper T-spine
Why do neuro patients have respiratory failure? As a result of their primary injury Due to secondary injury Other injuries Development of respiratory infection Development of ARDS
Corral et al looked at non-neurologic complications in severe TBI patients Respiratory infections in 68% of severe TBI patients Mortality not increased but hospital LOS, time on mechanical ventilation increased
Why is it important to understand airway anatomy? Airway Obstruction where is it? Will my rescue devices work? What is happening in laryngospasm? What if I need to crich someone?
Conditions that can compromise airway Degree of wakefulness Aspiration Body habitus Concurrent injuries Medications Co-morbidities
Airway Evaluation Facial Features Beard, no teeth, buck teeth, dentures, recessed jaw Neck Short neck, landmarks unclear Limited Mobility C-collar, arthritis
Quick Assessment: Mouth: how much can they open it? Tongue: how much can they protrude it? Jaw: mobility Neck: mobility
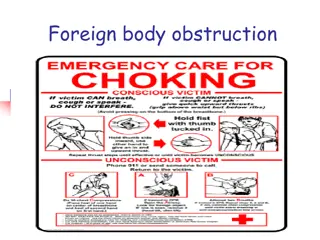
Airway Adjuncts what you can do before calling anesthesia Positioning Plastic in orifices Preoxygenate Jaw Thrust Check sedation
Placing a nasal trumpet Placed with bevel towards turbinates Left sided goes in angled down Right sided goes in facing upward and then turned
Placing an Oral Airway Pick the appropriate size 3-4 for small adult, 4-5 medium, 5-6 large Insert facing upward and then rotate down Do not use in an awake patient
Oxygen Delivery: High vs Low Flow Nasal Cannula Simple Face Mask Nonrebreather Face Mask Venti Mask Flow does NOT = FiO2
What drugs do you want? Sedatives Paralytics
Sedatives Etomidate Propofol Ketamine
Etomidate GABA like effects Minimal effect on BP; can lower ICP Can reduce plasma cortisol levels Hepatic metabolism; renally excreted Dose 0.3mg/kg
Propofol Anesthetic agent Respiratory and CV depressant can drop BP by as much as 30% Vasodilation and negative inotropic effect Dose is 1-1.5mg/kg
Ketamine Anesthetic and dissociative agent Hepatic metabolism Can cause laryngeal spasm, hypertension Emergence reaction give benzo with it 1-2mg/kg
Paralytics Succinylcholine Vecuronium Rocuronium Cisatricurium If you don t think you can BVM someone, don t paralyze them!!
Succinylcholine Only depolarizing NMB Avoid in hyperkalemia, 24 hour post major burn, neuromuscular disease, patients with several days of ICU critical illness Onset in 60 seconds and lasts around 5 minutes 1-1.5mg/kg
Rocuronium Nondepolarizing Onset about 90 seconds and last 30-40 minutes Lasts longer in those with hepatic impairment Dose is 0.6-1mg/kg Effect is dose dependent
Vecuronium Similar to rocuronium Slower onset time (up to 4 minutes) Lasts 40-60 minutes 0.08-0.1mg-kg
Conclusion Appropriate airway management is crucial in patients with brain injury Remember your airway anatomy and assessment in patient evaluation Use your adjuncts to help you Be vigilant in the drugs being given to your patients if intubation is required
References Corral L, Casimiro JF, Ventura JL, Marcos P, Herrero JI, Manez R. Impact of non-neurologic complications in severe traumatic brain injury outcome. Critical Care 2012; 16:R44. Karanjia N, Nordquist D, Stevens R, Nyquist P. A Clinical Descriuption of Extubation Failure in Patients with Primary Brain Injury. Neurocritical Care 2011; 15:4-12. Rincon F, Ghosh S, Dey S, Maltenfort M, Vibbert M, Urtecho J, McBride W, Moussouttas M, Bell R, Ratliff J, Jallo J. Impact of Acute Lung Injury and Acute Respiratory Distress Syndrome After Traumatic Brain Injury in the United States. Neurosurgery 2012; 71:795-803. Wong E, Yih-Yng Ng. The Difficult Airway in the Emergency Department. Int J Emerg Med, 2008: 1:107-111.