Approach to Critically Ill Patient: Primary Survey and Airway Management
This material provides a structured approach to managing critically ill patients, focusing on the primary survey steps including airway and cervical spine control. It covers assessment techniques, interventions, and guidelines for ensuring patient safety, particularly in cases of potential airway compromise or cervical spine injury. The content emphasizes the importance of effective airway management and prompt evaluation of cervical spine integrity in critical care scenarios.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Approach To The Critically Ill Patient Ahmed Mohamed Abdelazeem Critical Care Medicine Department Benha University 2019
PRIMARY SURVEY 1. Airway and cervical spine control 2. Breathing and ventilation 3. Circulation with hemorrhage control 4. Disability 5. Exposure/Environmental control
Airway and Cervical Spine Control
Assessment 1. Airway Patency Have the patient speak If the patient talks to you normally, the airway is clear. If there is no response to speech, perform a more detailed assessment of the airway Look, listen and feel Look tracheolaryngeal fractures for secretions, blood, vomit, foreign bodies, facial, mandibular, or Listen for upper airway noises Gurgling caused by fluids (secretions, blood or vomit) in the oropharynx Snoring partial airway obstruction at the pharyngeal level Stridor high-pitched inspiratory sound, may be associated with partial airway obstruction at the level of the larynx (inspiratory stridor) or the trachea (expiratory stridor) Hoarseness caused by partial laryngeal obstruction associated with oedema Absent breath sounds indicates either complete airway obstruction or absence of breathing Feel air flow
2. Airway Protection Testing the gag reflex or the ability to swallow 3. Assume Injury To The Cervical Spine In Any Patient With The Following Findings: Multi-system or major trauma Altered level of consciousness Blunt injury above the clavicles Concerning mechanism of injury Neck pain, ecchymosis or deformity Neurologic deficits A normal neurologic exam does not exclude cervical spine injury
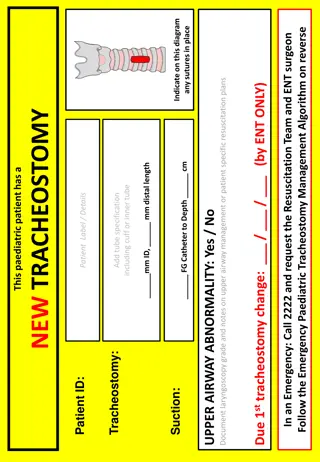
Interventions 1. General Guidelines Protection of the cervical spine All trauma victims should be placed in a protective cervical spine collar Prevention of aspiration Suctioning of the lower pharynx and oropharynx A vomiting patient should be rolled to the left lateral decubitus position and the entire spine properly protected so that the airway can be cleared.
2. Simple Maneuvers Head tilt/chin lift: contraindicated if neck injury is suspected Jaw thrust: the preferred method for patients with possible cervical spine injury 3. Airway Adjuncts Oropharyngeal airway (unconscious patient) Nasopharyngeal airway (semiconscious patient) Do not use a nasopharyngeal airway if you suspect a skull base fracture Laryngeal mask airway 4. Tracheal Intubation
Breathing and Ventilation
Assessment 1. Physical Examination Inspection: Observe the chest wall for symmetric rise as well as for paradoxical movement suggestive of flail chest Palpation: position of the trachea in the suprasternal notch, Subcutaneous Emphysema, for crepitus and rib tenderness Auscultation: provides clues to possible causes of respiratory arrest or distress, including pneumothorax, congestive heart failure (CHF), pulmonary edema, or pleural effusions
2. Monitoring pulse oximeter, end-tidal CO2 monitor 3. Diagnostics arterial blood gas, portable chest radiograph (+ pelvic and cervical spine views in multiply injured).
Interventions 1. Administration Of Supplemental Oxygen Nasal cannula: delivers oxygen at concentrations of 25% 45% at a flow rate of 1 6 L/min Simple face mask: delivers oxygen at concentrations of 40% 60% at a flow rate of 6 10 L/min Venturi mask: delivers oxygen at concentrations of 65% 75% at a flow rate of 12 15 L/min Non rebreather mask: delivers oxygen at concentrations of 24% 60% at a flow rate of 2 15 L/min Bag-mask: delivers oxygen at concentrations of 90% 97% at a flow rate of 12 15 L/min, while the previous methods require spontaneous respirations the BVM is used for apneic patients Mechanical positive-pressure ventilation
2. Treatment Of The Cause Needle thoracostomy Chest tube thoracostomy Thoracocentesis Furosemide
Circulation with Hemorrhage Control
Assessment 1. Physical Examination Pulse palpable carotid, femoral, radial, dorsalis pedis pulse = SBP > 60, 70, 80, 90 mm hg Neck veins Level of consciousness Skin temperature and color Capillary refill time Heart sounds Blood pressure Urine output
2. Monitoring Continuous electrocardiographic monitoring and noninvasive blood pressure monitoring 3. Diagnostics ECG, POCUS
Interventions 1. Establishing Intravenous Access 2. Take Initial Blood Samples For Blood Grouping, Full Blood Count, Coagulation Studies, Electrolytes, Kidney Functions, Liver Functions 3. Fluid Resuscitation, Blood Products, Vasopressors, Inotropes 4. Treatment Of The Cause needle decompression followed by tube thoracostomy for tension pneumothorax needle pericardiocentesis for cardiac tamponade thrombolytics for pulmonary embolism Cardioversion pacing
Assessment 1. Level Of Consciousness: AVPU/GCS 2. Pupillary Examination: Size, equality, reactivity to light In structural causes of coma the light reflex is usually absent, in metabolic causes it is usually present A difference in pupil diameters >1 mm suggests A structural cause 3. Movement Of Extremities And Lateralization 4. Check The Blood Glucose
Interventions 1. Anticonvulsants For Seizures 2. Dextrose For Hypoglycemia 3. Antidote For Drug Overdose
Exposure/ Environmental Control
Assessment Fully Undress The Patient To Examine The Patient s Skin Surface
Interventions 1. Remove All Wet Or Contaminated Clothing 2. Keep The Patient Warm By Applying warm blankets Ventilating with warm humidified air Administering warmed IV fluids
SECONDARY SURVEY 1. Subjective 2. Objective 3. Assessment and plans
Subjective Subjective
1. Chief Complaints Demographics Name Age Gender Admission date Source of referral Relevant comorbidities Complaining of
2. History Of Present Illness Presenting scenario (A brief summary of significant data only subjective, objective, assessment, plan in a chronological order, first during Pre hospital course then during ED/floor hospital course and finally during ICU course) Relevant Systems Review, Past History, Personal and Social History, Family History, Allergies, Medications
3. Systems Review Neurological Cardiovascular Respiratory Gastrointestinal Genitourinary Infectious Diseases Hematological Endocrinal Musculoskeletal
4. Past History Medical Surgical Ob/Gyn 5. Personal And Social History Occupation Marital status Living conditions Habits Tobacco, Alcohol, Illicit drugs
6. Family History 7. Allergies 8. Medications Indication Dose Duration Side effects
1. Physical Exam General Vitals (Height, Weight, Temperature, Heart Rate, Blood Pressure, Central Venous Pressure, Respiratory Rate, Oxygen Saturation, 24 hr Urine Output, Net Fluid Balance) HEENT Head, Eyes, Ears, Nose and sinuses, Throat Neck Cardiovascular Respiratory Abdominal Neurological Extremeties Skin
2. Laboratory Data ABG, CBC, Coagulation studies, electrolytes Na, K, Ca, Mg, Ph , Kidney functions, Liver functions, Thyroid function, Adrenal function, CRP, PCT, Cultures, Antibiotic levels, Troponins, Ck-Mb, others 3. Imaging Data X Ray, CT, MRI, US, ECG, ECHO, others
Assessment and Plans
1. Summary Statement with Synthesized Problem List Demographics (Name, Age, Gender, Admission date, Source of referral), Relevant comorbidities, Presented complaining of, Found to have main problems in descending order of importance 2. System Based/Problem - Based Assessment and Plans (Diagnostic, Therapeutic)
Problem list Disease Syndrome Symptom, Sign, Lab Finding, Imaging Finding
Daily Presentation 1. 2. 3. Summary Statement with Synthesized Problem List Major events during the last 24 h System - Based Assessment and Plans (Diagnostic, Therapeutic): Neurological (SOAP) Cardiovascular (SOAP) Respiratory (SOAP) Renal (24 hr Urine Output, Dialysis, Urea, Creatinine), Fluids (Net Fluid Balance, Cumulative Fluid Balance), Electrolytes (Na, K, Ca, Mg, Ph) Gastrointestinal (SOAP), Nutrition (Albumin, Tolerance) Genitourinary (SOAP) Infectious diseases (Temperature, TLC, CRP, PCT, Cultures, Antibiotic levels) Hematological (CBC, PT, PTT, Fibrinogen, FDPs, D-dimer, Peripheral blood smear, Blood products transfusion) Endocrinal (Glycemic control, Thyroid function, Adrenal function) FAST HUGS SLR: Feeding, Analgesia, Sedation, Thromboembolic prophylaxis, Head of bed elevation, Ulcer prevention, Glycemic control, Skin breakdown Wounds, Bedsores , Stool, Lines/catheters/drains, Readiness to wean Physical Therapy Discharge Planning
Summary Primary Survey Airway and cervical spine control Breathing and ventilation Circulation with hemorrhage control Disability Exposure/Environmental control Secondary Survey Subjective Objective Assessment and plans