Parathyroid Carcinoma Misdiagnosed as Thyroid Lesion: A Case Study
Parathyroid carcinoma (PC) is a rare malignancy often challenging to differentiate from benign thyroid nodules. This case study highlights a 50-year-old male patient whose nonfunctioning sporadic PC was initially misidentified as a follicular thyroid nodule. Despite preoperative evaluations, including ultrasound and fine-needle aspiration cytology, the parathyroid nature of the lesion went unnoticed until definitive histology and immunostaining revealed the true diagnosis. The study underscores the importance of considering PC in the differential diagnosis of neck lesions and the limitations of traditional diagnostic methods in distinguishing parathyroid tumors from thyroid nodules.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Are thyroid and parathyroid lesions wrongly reported in a thyroid pathology sample? Does ultrasound help to differentiate adenoma lesions from parathyroid carcinoma?
Parathyroid carcinoma is rare, representing<1% of primary hyperparathyroidism cases. Parathyroid carcinoma (PC) is an uncommon malignancy, less than 1000 recorded cases reported in literature since described by de Quervain in 1904
We report a 50-year-old male patient who was referred to our department for a right thyroid nodule, incidentally detected on carotid Doppler ultrasound scan, with a fine-needle aspiration cytology showing a follicular lesion. At the time of our evaluation, neck ultrasound showed a 1.3 cm right hypoechoic thyroid nodule with irregular margins and the absence of enlarged bilateral cervical lymph nodes. Thyroid function tests were normal. Serum calcium was normal and plasma PTH slightly above the upper limit of the normal range. The patients underwent right lobectomy. The intraoperative frozen-section pathological examination raised the suspicion of a PC. Definitive histology showed a markedly irregular infiltrative growth of the tumor with invasion of the thyroid tissue and cervical soft tissues.
Immunostaining for thyroglobulin was negative, whereas staining for chromogranin A and PTH showed a strong reactivity. Based on the microscopic findings and the immune histochemical profile, the tumor was diagnosed as a PC. Postoperative serum calcium and phosphate levels were in the normal range. This is the first case of a nonfunctioning sporadic PC misdiagnosed prior of surgery as a follicular thyroid nodule. The parathyroid nature of the neck lesion could not be suspected before surgery. Fine-needle aspiration cytology (FNAC) may fail to distinguish a parathyroid tumor from a benign thyroid nodule because at FNAC, parathyroid and thyroid lesions have some morphological similarities. Histological criteria are not always sufficient for the differential diagnosis, which can definitely be established using immunohistochemistry.
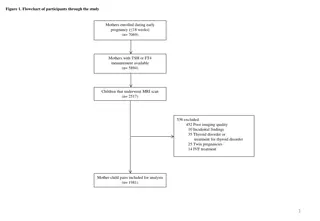
Retrospective data of patients referred for evaluation of parathyroid disease between 2001 and 2018 were reviewed. The goal was to describe the clinical presentation, histopathologic characteristics, and treatment outcomes of parathyroid carcinoma.
patients were managed for hypoparathyroidism, and 30 patients were found to have normal parathyroid function. Of the 175 patients with hyperparathyroidism, 149 individuals had primary hyperparathyroidism, including 9 patients with parathyroid carcinoma; 22 cases were secondary hyperparathyroidism; 3 were tertiary hyperparathyroidism; one patient had familial hypocalciuric hypercalcemia. Of the parathyroid cancer cases, one was excluded as the pathology sample from another institution was not available for review.
We identified 8 cases of parathyroid carcinoma from the outpatient practice of a quaternary care Endocrine Oncology practice in Toronto, Canada.
The clinical presentation was as follows: 5/8 cases (62.5%) of symptomatic hypercalcemia and 3/8 cases (37.5%) of a suspicious thyroid nodule. Hypercalcemia was evident in all 7 case with pre-operative calcium measurements. Histopathologic features included: vascular invasion in 7/8 cases (87.5%) and immunohistochemical loss of either parafibromin,retinoblastoma, or p27 in all 8 cases. Additional treatment included: external beam radiotherapy in 5/8 cases (62.5%), chemotherapy for 2/8 patients (25%), and additional surgery for 3/8 patients (37.5%). Only 2 patients (25%) had long-term remission following surgical treatment, and the others had either persistent (3 patients) or recurrent disease(3 patients). Five patients developed metastatic disease, all involving lung. In one of two patients treated with Sorafenib there was evidence of regression of lung metastases. One patient died of disease progressin.
If PC is pre-operatively suspected, FNA should be avoided due to the risk of tumor dissemination along the needle tract, with higher risk of recurrence;biopsy has resulted in capsular rupture and PT tissue diffusion.
Ultrasonography showed that parathyroid carcinomas tend to be large, inhomogeneous, hypoechoic masses with lobulated contours. In contrast, parathyroid adenomas were small, homogeneous, hypoechoic masses with smooth borders. The mean (range) DW ratios for parathyroid carcinomas were 1.21 (0.91-2.5) and 0.64 (0.33- 1.47) for adenomas; the difference was statistically significant (p<0.0001). The DW ratio was 1 in 15 (94%) of the 16 cases of carcinoma, whereas only 3(5%) of the 61 adenomas had a similar ratio.
Ultrasonographic examination is useful not only for preoperative localization but also for differentiating parathyroid carcinoma from adenoma. Parathyroid tumors with irregular margins, inhomogeneous echogenicity, and a DW ratio 1 are likely to be malignant.
A 53-year-old female was referred for the exclusion of metabolic bone disease. She presented with low back pain that had persisted for the past 6 months and elevated serum alkaline phosphatase (1,253 IU/L). Four years previously, she had been diagnosed at a local hospital with a 2.3-cm thyroid nodule, which was determined to be pathologically benign. Radiofrequency ablation was performed at the same hospital because the nodule was still growing during the follow-up period 2 years before the visit to our hospital, and the procedure was unsuccessful in reducing the size of the nodule.
The results of the laboratory tests in our hospital were as follows: serum calcium, 14.6 mg/dL; phosphorus, 3.5 mg/dL; and intact parathyroid hormone (iPTH), 1,911 pg/mL. Neck ultrasonography and 99mTc sestamibi scan detected a 5-cm parathyroid neoplasm in the left lower lobe of the patient s thyroid; left parathyroidectomy was performed. This case indicated that thyroid ultrasonographers and pathologists need to be experienced enough to differenti- ate a parathyroid neoplasm from a thyroid nodule; 99mTc sestamibi scan, serum calcium, and iPTH levels can help to establish the diagnosis of parathyroid neoplasm
Parathyroid adenomas are frequently mistaken cytologically for a follicular lesion of the thyroid. Most patients with a parathyroid adenoma have hypercalcemia, which is a clue to the correct diagnosis. Immunohistochemistry for thyroglobulin and parathyroid hormone can be helpful if a non thyroid origin is suspected.