Understanding the Differences Between Fibrolamellar Carcinoma (FLC) and Hepatocellular Carcinoma (HCC)
Fibrolamellar Carcinoma (FLC) and Hepatocellular Carcinoma (HCC) are distinct liver cancers with important differences in age of onset, underlying causes, diagnostic markers, metastatic patterns, symptoms, treatment options, and outcomes. FLC primarily affects young and healthy individuals with no known risk factors, while HCC is more common in elderly individuals with liver disease. Diagnosis, treatment, and prognosis vary significantly between these two types of liver cancer.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
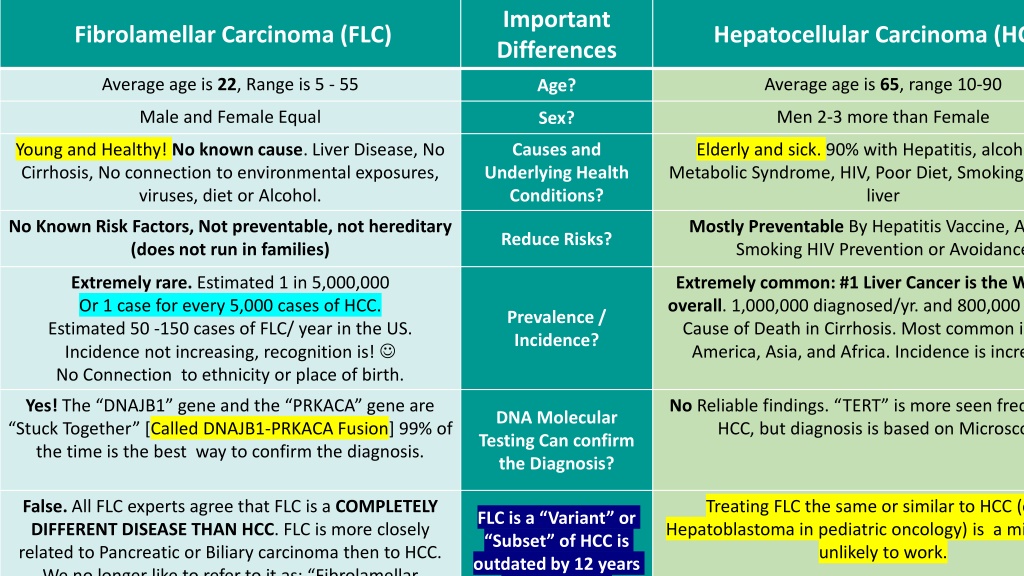
Important Differences Fibrolamellar Carcinoma (FLC) Hepatocellular Carcinoma (HCC) Average age is 22, Range is 5 - 55 Average age is 65, range 10-90 Age? Male and Female Equal Men 2-3 more than Female Sex? Young and Healthy! No known cause. Liver Disease, No Cirrhosis, No connection to environmental exposures, viruses, diet or Alcohol. Causes and Underlying Health Conditions? Elderly and sick. 90% with Hepatitis, alcoholism, Metabolic Syndrome, HIV, Poor Diet, Smoking, or other liver No Known Risk Factors, Not preventable, not hereditary (does not run in families) Mostly Preventable By Hepatitis Vaccine, Alcohol, Smoking HIV Prevention or Avoidance Reduce Risks? Extremely rare. Estimated 1 in 5,000,000 Or 1 case for every 5,000 cases of HCC. Estimated 50 -150 cases of FLC/ year in the US. Incidence not increasing, recognition is! No Connection to ethnicity or place of birth. Extremely common: #1 Liver Cancer is the World/4 overall. 1,000,000 diagnosed/yr. and 800,000 die/yr. #1 Cause of Death in Cirrhosis. Most common in North America, Asia, and Africa. Incidence is increasing. Prevalence / Incidence? Yes! The DNAJB1 gene and the PRKACA gene are Stuck Together [Called DNAJB1-PRKACA Fusion] 99% of the time is the best way to confirm the diagnosis. No Reliable findings. TERT is more seen frequently in HCC, but diagnosis is based on Microscopy DNA Molecular Testing Can confirm the Diagnosis? False. All FLC experts agree that FLC is a COMPLETELY DIFFERENT DISEASE THAN HCC. FLC is more closely related to Pancreatic or Biliary carcinoma then to HCC. We no longer like to refer to it as: Fibrolamellar Treating FLC the same or similar to HCC (or as Hepatoblastoma in pediatric oncology) is a mistake and unlikely to work. FLC is a Variant or Subset of HCC is outdated by 12 years and incorrect.
Important Differences Fibrolamellar Carcinoma (FLC) Hepatocellular Carcinoma (HCC) AFP almost Always normal. If elevated typically < 100. Vitamin B12 can be Elevated in approximately 3 out of 4 cases. Ammonia levels maybe Elevated, as well. Additionally we find many with increased Procalcitonin and IL-6. Circulating Tumor DNA monitoring (Signatera) has shown to be a reliable marker in the majority of cases. AFP (Alpha-Feto Protein) Almost always elevated 100, is a reliable marker in HCC. Vitamin B12 not elevated. Tumor Markers? Interestingly we find some cases with spread to the lungs, and others only to the abdominal region. Still trying to understand why this is. Rarely bone or head. More likely to Spread to Abdomen then Lungs in FLC. Metastasis Spread to Lungs and Abdomen Equally More Rapid Onset of Extreme Fatigue, loss of weight, shoulder pain, loss of muscle mass, perhaps elevated ammonia, headaches, night sweats gynecomastia (breast growth) in males (tumor producing estrogen). Gradual onset of Jaundice, Ascites, Blood Clots, Weight Loss, Portal Hypertension. Symptoms? Rarely Curative. However we have seen multiple cases of long term successes. If metastatic disease was present at time of transplant along with the need to remain on immunosuppressive drugs the recurrence rates are extremely high. Transplant should be carefully evaluated for risk vs. benefit. This is the type of case our group of Liver Transplant? Can be Curative in HCC.
Important Differences Fibrolamellar Carcinoma (FLC) Hepatocellular Carcinoma (HCC) False. FLC is a Systemic Disease. Except in very rare, stage 1 cases, FLC cannot be cured by surgery alone. Systemic therapy is needed. True. HCC can be cured by Surgery if all visible tumor is removed. It s a Surgical Disease. Chemotherapy Immunotherapy Doesn t Work False. FibroFighters Has Shown 4 different Chemotherapy Regimens can be Highly Effective. Mostly True. Modest improvements with a few regimes is seen. Atezolizumab (Tecentriq) / Bevacizumab (Avastin) Does Not work in FLC. Modest Improvement in Survival (4 -7 months) If given with other agents may benefit some patients Does Not work in FLC. Combinations with at least 2 other drugs with Lenvatinib, and the addition of a CPI can create synergies not found when using any monotherapy. Monotherapies, such as Sorafenib, Lenvatinib Modest Benefit to Some Patients, ie increased survival by 1-2 months. Does not work in FLC unless combined with vaccine, gemcitabine or capecitabine. Additionally radiation or some form of ablation can also prime the immune system. Works best when stimulating the immune microenvironment. Ipilimumab and Nivolumab Some Modest Benefit in Some Patients Surgery is not an option 50-75% of Unresectable FLC, become resectable. Typically remains unresectable
Take Home: ENGAGE WITH EXPERTS IN FLC. Knowledge and expertise in HCC does not translate into experience or knowledge of FLC. Multi-disciplinary care involving oncology, surgical, interventional radiology, radiation oncology and patient advocates with experience of living with FLC is necessary. Nothing is 100% in Cancer. Here are some rare exceptions to the rules listed above. There is a subset of cancers that share HCC and FLC characteristics- typically women age 35-55, with a BAP-1 mutation, some with, some without the DNAJB1-PRKACA fusion. We don t have a good name for these cancers yet, but we recommend treating them like FLC. There are very rarely biliary or pancreatic cancers with DNAJB1-PRKACA fusion. We also recommend treating these like FLC. There is an extremely rare condition called Carney Syndrome where FLC occurs In 180+ patients we have not yet seen it.