Overview of Eye, Ear, Nose, and Throat Infections by Nenad Pandak
In this comprehensive guide by Nenad Pandak, various aspects of eye, ear, nose, and throat infections are discussed. The content covers infections such as conjunctivitis, keratitis, pharyngitis, otitis media, and sinusitis. It also delves into causes, clinical presentations, and diagnosis of these infections, making it a valuable resource for ophthalmologists, ENT specialists, infectious disease specialists, and general practitioners.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Eye, Ear, Nose, and Throat Infections Nenad Pandak
Why ? Ophthalmologist ENT specialist ID specialist & GP Familiar with these infections Preliminary empiric therapy
Task Eye infections Conjuctivitis Keratitis Endophtalmitis Throat infections Pharyngitis Epiglottitis
Task Ear infections Otitis externa Otitis media Mastoiditis Sinus infections Sinusitis
Conjuctivitis Inflammation of conjuctiva Doesn t threaten the vision Rapid respond to therapy
Conjuctivitis Direct contact with the environment Tears Antibacterial agents Lysozyme, IgA, IgG Decresed tear production Recurrent infections
Clinical presentation Vessel dilatation red eye Pus formation Eyelid swelling Itching, pain Glued eyelid shut (dried purulent exudate)
Causes Bacteria Viruses Staph. aureus Str. pneumoniae H. influenzae M. catarrhalis N. gonorrhoeae N. meningitidis P. aeruginosa C. trachomatis Adenoviruses Enteroviruses HSV VZV Measles
Causes Fungi Parasites Candida Blastomyces Sporothrix schenckii Trichinella spiralis Taenia solium Schistosoma haematobium Lola loa Onchocerca volvulus
Causes Viral The most common Highly contagious Spread to the 2ndeye in 24-48 hrs Bacterial Highly contagious Profuse pus formation
Causes Allergic and toxic Pollens Symmetrical Itching Systemic diseases Reiter syndrome Vasculitis SLE
Diagnosis History & examination Severe cases Swab or scraping: Gram stain & culture Viral: mononuclear cell exudate Allergic: eosinophils Bacterial: PMNs
Treatment ANd9GcQplxbp_eigv6CRGbCiYCAZ9SIwG1F_ZVQKQzYWJwnrQ_Afo_wSPQ_dZ8SWgQ Topical antibiotics? To do or not to do? Are your eyelids glued in the morning?(+5) Does your eye itch? (-1) Do you have recurrent conjuctivitis?(-2) Score: 5 bacterial 77% 2 bacterial 2%
Treatment Prefered therapy Moxifloxacin 0.5% sol TID 7 days Alternate therapy Gentamycin Tobramycin Polymyxin B / bacitracin Neomycin / polymixin
Keratitis Inflammation of cornea Prompt treatment Corneal perforation blindness
Predisposing conditions Minimal injury of cornea Trauma Contact lens abrasion Eye surgery Impaired tear production Diabetes mellitus Immunosupression Comatose patient
Causes Bacteria 65-90% Some produce toxins and enzymes Penetration without epithelial disruption Hypopyon is the rule Perforation
Causes Staph. aureus P. aeruginosa (contact lenses) N. gonorrhoeae N. meningitidis H. influenzae
Causes Viruses HSV recurrent keratitis Unilateral Dendritic lesion Erythema, pain, foreign body sensation HSV-fluor
Causes Fungi After organic material injury (tree branch) Prolonged corticoid eye drop therapy Aspergillus Protoza Unsterilized tap water for contact lens cleaning Acanthamoeba
Clinical presentation Eye pain Foreign body sensation Corneal edema impaired vision Photophobia Reflex tearing
Diagnosis Medical history & exam Swab or scraping Gram stain, Giemsa stain, methenamine silver stain, culture Therapy Emergently Experienced ophthalmologist
Endophthalmitis Serious infection Ocular chamber & adjacent structures Involving all tissue layers: panophthalmitis Often leads to blindness
Predisposing conditions Posttraumatic Staph. aureus and epidermidis Str. spp Bacillus cereus Fungi Organic matter penetrating injuries
Predisposing conditions Hematogenous Any source of bacteremia 2/3 right eye Candida albicans G + and G bacteria Bacillus cereus IDU
Predisposing conditions Contiguous spread Uncontrolled keratitis Delays in antibiotic therapy
Predisposing conditions Ocular surgical procedures Staph. aureus and epidermidis Str. spp Early 1 5 days after the surgery Delayed Weeks to months after the surgery Opportunistic pathogens
Clinical presentation Eye pain Eye redness Photophobia Reduced vision Fever, algic syndrome
Diagnosis and therapy Cultures and smears Systemic broad spectrum antibiotics Intravitreal antibiotic injection 1/10 patients enucleation Experienced ophthalmologist
Pharyngitis Common infectious disease Usually self-limiting Antibiotics malpractice
Causes Viruses Rhino, corona, adeno, HSV, EBV, CMV, influenza, parainfluenza, coxsackie A, HIV Bacteria Group A streptococci (GAS) Children 50% of all cases Adults 10%
Diagnosis Centor clinical criteria Tonsillar exudates Tender anterior cervical adenopathy Fever Abscence of cough
Diagnosis 3-4 criteria Positive predictive value 40-60% 3-4 criteria absent Negative predictive value 80% Adding age 3 14 y/o: +1 >45 y/o: -1
Therapy Penicillin the drug of choice Oral Penicillin VK 10 days Benzathine penicillin 1.2-2.4 MU im once Penicillin-allergic patients Clarithromycin, clindamycin, cephalosporins 10 days, azithromycin 3 days
Peritonsillar abscess Symptoms worsening despite antibiotics Medial displacement of uvula Soft palate bulging Surgical intervention Recurrent abscess tonsillectomy
Epiglottitis High fever Difficulty swallowing Drooling Difficulty breathing Indirect laryngoscopy Swollen, cherry-red epiglottis
Epiglottitis High risk of airway obstruction Children Mortality 80% Adult Closely monitored Endotracheal intubation
Epiglottitis Causes H. influenzae Str. pneumoniae Staph. aureus Therapy 3rd generation cephalosporins iv 7-10 days
Otitis externa Immunocompetent Mild disease Immunocompromised Possible life threatening
Otitis extrena Local itching and pain Redness and swelling of the external canal skin Tenderness of the auricula
Causes Gram-negative bacteria P. aeruginosa the most prevalent Staph. epidermidis or aureus Candida or Aspergillus
Therapy Polymyxin neomicin sol. + Hydrocortison sol. Clotrimazol or miconazol
Malignant otitis externa Immunocompromised Severe pain Spreading of necrotizing infection Skull, meninges, brain CT scan, MRI Gallium scan P. aeruginosa almost always! Systemic therapy 6 weeks + surgical debridement
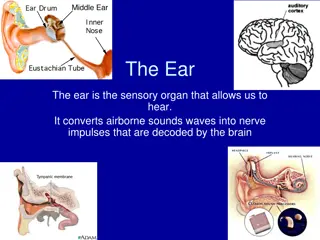
Otitis media Most commonly in childhood Up to 3 y/o 2/3 of children at least 1 episode Consequence of the Eustachian tube obstruction
Otitis media Viral upper respiratory infection Serous fluid accumulation Eustachian tube obstruction 5-10 days later fluid infected with mouth flora