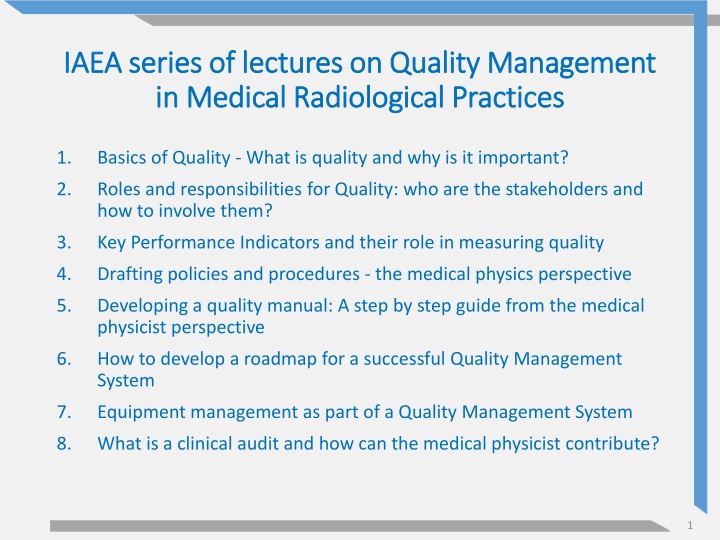
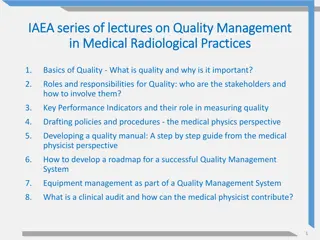
IAEA series of lectures on Quality Management in Medical Radiological Practices
Quality management in medical radiological practices is crucial for ensuring the delivery of high-quality healthcare services. This series of lectures covers topics such as the basics of quality, roles and responsibilities, key performance indicators, drafting policies, developing a quality manual, and more. Understanding quality in healthcare, managing, evaluating, and measuring quality are key components discussed in these lectures. The importance of conformance to requirements and defining quality in healthcare are emphasized to enhance healthcare outcomes effectively.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
IAEA series of lectures on Quality Management IAEA series of lectures on Quality Management in Medical Radiological Practices in Medical Radiological Practices 1. Basics of Quality - What is quality and why is it important? 2. Roles and responsibilities for Quality: who are the stakeholders and how to involve them? 3. Key Performance Indicators and their role in measuring quality 4. Drafting policies and procedures - the medical physics perspective 5. Developing a quality manual: A step by step guide from the medical physicist perspective 6. How to develop a roadmap for a successful Quality Management System 7. Equipment management as part of a Quality Management System 8. What is a clinical audit and how can the medical physicist contribute? 1
Basics of Quality - What is quality and why is it important? Quality Management in Medical Radiological Practices (Diagnostic Radiology, Nuclear Medicine and Radiotherapy) 2
Objective The objectives of this presentation are to: understand the basics of quality and why it important in a radiation medicine department learn what are processes for managing, monitoring, evaluating and measuring the quality of a healthcare service at different levels and in different domains.
Content What is quality in healthcare? Why is quality in healthcare important? What are the key principles of managing, evaluating and measuring quality in healthcare? 4
Quality is defined as conformance to requirements Philip Crosby 5
What is quality in healthcare? On a broad level, quality can be defined as the degree to which a set of inherent characteristics of an object fulfils requirements . Using this definition: object= healthcare service requirements= needs or expectations from the healthcare service, which are implied or obligatory International Organization for Standardization. ISO 9000:2015. Quality management systems fundamentals and vocabulary. 2015. 6
What is quality in healthcare? Quality in healthcare can also be defined as the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge. Institute of Medicine (US) Committee to Design a Strategy for Quality Review and Assurance in Medicare. Medicare A Strategy for Quality Assurance. Editor: Kathleen N. Lohr. Washington (DC): National Academies Press (US); 1990. 7
What is quality in healthcare? All definitions of quality incorporate: Setting appropriate targets; Determining the degree to which we achieve those targets, i.e. how close we are to reaching them. Best outcomes 8
Pause and Ponder What targets do you currently have at your medical radiological practice and who determines them? 9
Why is quality important? Quality ensures that the healthcare service meets its targets of being: 1. Effective; 2. Efficient; 3. Accessible; 4. Acceptable/patient-centred; 5. Equitable; 6. Safe. quality badge by Free Icon Pack is licensed under CC0 1.0 World Health Organization. (2006). Quality of care: a process for making strategic choices in health systems. World Health Organization. 10
Quality: Effective Evidence-based practice and scientific knowledge should be used to decide on appropriate clinical pathways. Healthcare services should be offered to all who could benefit rather than those not likely to benefit, avoiding underuse and overuse. arrow decision outline by Material Design Icons is licensed under Apache Licence 2.0 11
Quality: Efficient The healthcare system should use all its resources at maximum capacity, avoiding waste in: Time; Money; Human capital; Equipment/supplies; Energy; Ideas. recycle by Carbon Icons is licensed under Apache Licence 2.0 12
Quality: Accessible Delays should be avoided for both those who receive and those who deliver healthcare services. Healthcare services should be offered within a reasonable distance from where people live. Skills and resources should be appropriate to the clinical need. timer by OpenMoji Emoji Set is licensed under CC BY 4.0 ambulance by BoxIcons Set is licensed under CC BY 4.0 Tablets by Font Awesome Icons is licensed under CC BY 4.0 13
Quality: Acceptable/patient-centred Healthcare services should be respectful and responsive to the patients Preferences; Needs; Values; Culture. Patients should be involved in clinical decisions. family practice by Medical Icon Set is licensed under MIT License 14
Quality: Equitable The provision of healthcare should not vary in quality on account of: Gender; Race; Ethnicity; Geographical location; Socioeconomic status. balance scale by OpenMoji Emoji Set is licensed under CC BY 4.0 15
Quality: Safe The doctrine first do no harm should be fundamental to the ethos of healthcare services. The risk and harm to all healthcare service users should be minimized. Although safety tends to refer to patients, the safety of healthcare providers must also be considered. Warning alt filled by Carbon Icons is licensed under Apache Licence 2.0 16
Pause and Ponder Out of the quality criteria listed, where do you currently place emphasis at your medical radiological practice? 17
How can we manage quality? Quality Management is the strategic framework and all the activities that are in place to manage and assure quality in a healthcare service. Quality Management incorporates seven principles: Customer focus; Leadership; Engagement of people; Process approach; Improvement; Evidence-based decision making; Relationship management. International Organization for Standardization. ISO 9000:2015. Quality management systems fundamentals and vocabulary, 2015. For more details, refer to the lecture on how to develop a roadmap for a successful quality management system 18
Quality is teamwork Quality requires leadership support but: Quality is everyone s responsibility. Quality is not the responsibility of only the quality lead or quality department. The quality management process requires the engagement of all individuals who are part of the healthcare service. For more details, refer to the lecture on roles and responsibilities for quality and safety: who are the stakeholders and how to involve them People team by Fluent UI System Icons is licensed under MIT License 19
What is Quality Improvement? Quality Improvement is part of Quality Management. Quality Improvement is the systematic, planned and extensive approach to monitor, study and improve the quality of the healthcare system. Quality is a progressively improving state, therefore quality improvement should be continuous. High bars by Health Icons is licensed under MIT License 20
What is Quality Assurance? Quality Assurance is the set of activities and processes set in place to ensure that the healthcare service meets appropriate quality standards. Quality Assurance monitors and ensures compliance against certain necessary standards whereas Quality Improvement is a continuous improvement process further and beyond standards. 21
What is Quality Control? Quality Control is the set of operational activities used to assess and verify that appropriate quality standards are met. Quality Control is part of the Quality Assurance framework. Quality Assurance is a proactive process whereas Quality Control is reactive. Tasks App by Fluent UI System Icons is licensed under MIT License 22
QM, QA and QC relationship Quality Management (QM) Quality Management (QM) Strategy and all activities used to manage quality Quality Assurance (QA) Quality Assurance (QA) Proactive process to ensure quality Quality control (QC) Quality control (QC) Reactive process to evaluate quality Adapted from: Delis H, Christaki K et al. Moving beyond quality control in diagnostic radiology and the role of the clinically qualified medical physicist. Phys Med. 2017 Sep;41:104-108. 23
Example 1: Hand Hygiene Hand hygiene is recognized as the cornerstone of infection control in healthcare. The World Health Organization has published guidelines on how and when to apply hand hygiene. Compliance with hand hygiene guidelines can be measured and audited. wash hands by OpenMoji Emoji Set is licensed under CC BY 4.0 24
Example 1: QM vs QA vs QC Quality Management of hand hygiene in a hospital Quality Control: monitor clinical operations to evaluate that hand hygiene targets are met. Quality Assurance: framework of policies, procedures, training and quality control to ensure that hand hygiene targets are met. Quality Management: Organizational strategy and activities aiming at continuous Quality Improvement of hand hygiene beyond targets by e.g. empowering champions in each clinical area to suggest actions. 25
Example 2: Radiological Equipment The IAEA Basic Safety Standard describes the responsibility of radiological equipment users to develop a quality assurance programme for medical radiological equipment Regulatory documents, international standards and professional guidelines provide information on criteria and methods to be used in performance and safety assessment of equipment. ct scan by OpenMoji Emoji Set is licensed under CC BY 4.0 INTERNATIONAL ATOMIC ENERGY AGENCY, Radiation Protection and Safety of Radiation Sources: International Basic Safety Standards, General Safety Requirements, 2014. (paragraph 3.171) 26
Example 2: QM vs QA vs QC Quality Management of medical radiological equipment Quality Control: tests and audits of radiological equipment performance and safety throughout its lifetime. Quality Assurance: the organizational framework, including committees, policies, procedures, manuals, work instructions and checklists describing the responsibilities of staff, the type of quality control performed, its frequency and the planned response to findings. Quality Management: Organizational strategy and activities aiming at continuous Quality Improvement in the use of medical radiological equipment by e.g. emphasizing quality performance criteria at procurement stage. 27
Pause and Ponder Can you think of any cases at your medical radiology practice where the terms Quality Control and Quality Assurance may be used incorrectly? 28
How can we evaluate quality? The quality of a healthcare service can be evaluated in the following domains: Structure; Process; Outcomes. hospital by Health Icons is licensed under MIT License process by Unicorns Icon Set is licensed under Apache Licence 2.0 Donabedian, A. Explorations in Quality Assessment and Monitoring, Volume 1: The Definition of Quality and Approaches to Its Assessment. Ann Arbor, Michigan: Health Administration Press. 1980. Heart Pulse by Fluent UI System Icons is licensed under MIT License 29
Quality: Structure The structure of a healthcare service provides information about its capacity to provide high quality care. Examples of structure-related information: Number of PET-CT systems installed; Number of radiography technologists available per shift; Availability of electronic patient medical records. 30
Quality: Process The process of a healthcare service provides information about its actions to maintain and improve the quality of care. Examples of process-related information: Patient waiting times to get exam or treatment; Time required after an exam to get results; Number of patient safety incidents; Percentage of patients requiring repeat exams. 31
Quality: Outcomes The outcomes of a healthcare service provide information about its impact on the health status of patients. Examples of outcome-related information: Number of breast cancers detected with mammography; Survival rates and quality of life after radiotherapy treatment; Patient satisfaction from the healthcare service. 32
Quality evaluation domains Structure (capacity) Process (actions) Outcomes (impact) Continuous quality improvement on a local level typically focuses on the process domain. Measuring outcomes can be challenging when looking at a local (department) rather than a national (country) level. 33
How can we measure quality? Key Performance Indicators (KPIs) are tools used for measuring and monitoring the quality of a healthcare service. KPIs can be linked to the three quality domains (structure, process, outcomes) and/or the six healthcare targets (effective, efficient, accessible, acceptable/patient-centred, equitable and safe). Published literature and professional guidelines, provide examples of KPIs for healthcare services, including medical radiological practices. 34
What are the best KPIs? KPIs should focus on what is important for a healthcare service rather than what is easy to measure. KPIs should be Specific, Measurable, Attainable, Relevant and Time-bound (SMART). For more details, refer to the lecture on Key Performance Indicators and their role in measuring quality 35
Pause and Ponder What type of evidence would you provide to demonstrate that your medical radiological practice adheres to quality and safety standards? 36
Patient safety program Patient safety is fundamental to delivering quality healthcare services. The patient safety program should be designed to reduce risks, errors and harm that occur to patients during provision of health care. Procedures by Font Awesome Icons is licensed under CC BY 4.0 37
Risk management program The risk management program identifies risk factors and implements processes to either prevent those risks or minimize their impact. The program includes risks to patients, visitors, staff members, the department and hospital. high risk users by Carbon Icons is licensed under Apache Licence 2.0 38
Risk management and quality Risk management can come as a response to quality and safety incidents but is ideally a proactive approach. Risk management includes identifying limitations of current practice, monitoring of issues and planning for improvements. Risk management also allows for safety and quality issues to be brought to the attention of decision makers for appropriate prioritization of resources. Risks can impact on both quality and safety. 39
Example 1: quality and safety Risk of not being able to recruit staff in radiology Safety issue: Overworking current staff will result in fatigue, which will lead to patient management errors and safety incidents. Quality issue: Reducing work hours of current staff will result in longer waiting times for patients, late treatment of diagnosed conditions and patient dissatisfaction. 40
Example 2: quality and safety Risk of incorrect patient identification at registration Safety issue: Errors in patient identification, if undetected, will result in radiation safety incidents of accidental and unintended medical exposures. Quality issue: If patient identification errors are detected before the medical exposure but late in the patient journey, they can result in exam rescheduling, patient dissatisfaction and waste of time and resources. 41
Pause and Ponder How are safety incidents reported and tracked at your medical radiological practice? Are risk assessments documented and submitted to senior management? 42
Is quality cost-effective? Good health is the foundation of a country s human capital, and no country can afford low quality or unsafe healthcare. Low quality healthcare increases the financial burden on the service provider and on patients. Healthcare professionals can be motivated beyond financial incentives to provide a high-quality service. World Health Organization, Organisation for Economic Co-operation and Development & International Bank for Reconstruction and Development. (2018). Delivering quality health services: a global imperative for universal health coverage. World Health Organization. money by Windows Icons is licensed under CC BY 3.0 43
Quality in healthcare and the IAEA The IAEA has always played an important role in risk management and patient safety in relation to the use of ionizing radiation in healthcare. The IAEA Basic Safety Standard describes the responsibility of registrants and licensees to establish comprehensive programmes of quality assurance for medical exposures, with the help of multidisciplinary teams and international standards. INTERNATIONAL ATOMIC ENERGY AGENCY, Radiation Protection and Safety of Radiation Sources: International Basic Safety Standards, General Safety Requirements, 2014 44
Quality in healthcare and the IAEA The IAEA provides audit tools for quality improvement of healthcare services using ionizing radiation: Comprehensive Clinical Audits of Diagnostic Radiology Practices: A Tool for Quality Improvement; QUANUM 3.0: An Updated Tool for Nuclear Medicine Audits; Comprehensive Audits of Radiotherapy Practices: A Tool for Quality Improvement | IAEA 45
Quality in healthcare and the IAEA IAEA publications also provide overview on equipment quality management systems for different modalities: Nuclear Medicine Physics Handbook; Diagnostic Radiology Physics Handbook; Radiation Oncology Physics Handbook. 46
Summary There are processes for managing, monitoring, evaluating and measuring the quality of a healthcare service at different levels and in different domains. Quality is a key attribute of a healthcare service and a key contributor to the success of a healthcare service. 47
A word from around the world to describe the added value of a Quality Management System in the clinical routine 48
In the 1950s, Deming transformed industry with his work on improving quality. Unfortunately healthcare did not take advantage of this and many practices are very dated even today. Medicine is evidence-based but it would seem that management and quality are left in the 1950 s despite much proof of its huge impact. I am not sure why more do not study and implement quality management and improvement; let us look at the benefits: Quality is everyone s responsibility and if you empower all staff to improve the service, their satisfaction and engagement increases. If you improve quality, Deming showed that the costs go down so management are happy. Finally if you improve the service, patients benefit hugely. There are no losers with quality improvement. Dr. Margaret Hall, Consultant in Nuclear medicine, Royal Free London NHS Foundation Trust, United Kingdom 49
I believe that education, as in the act of teaching and learning, is at the core of any effective quality management system. Clinical audit is a mainstay of a quality management system. It can be driven by the quality assurance framework, quality control (a specific area has been identified to be audited) or new evidence/research where the audit will evaluate practice in order to effect positive change. Regardless of what the drive has been to guide clinical audit, education will inform it and education will always be the answer to interpret and implement findings. This is true whenever there is a need to educate staff to correct a system/behaviour, educate the team to implement a system change brought about by the results of the audit or educate oneself to understand and further develop future audits. My approach to quality and safety management systems is always propelled by either the education of myself, systems and/or others. Liliana Barreira Lynch, Radiation Safety Officer, Children s Health Ireland at Temple Street 50