Hyperemesis Gravidarum: Causes, Symptoms, and Treatment
Hyperemesis gravidarum is a severe form of nausea and vomiting during pregnancy, affecting around 27% to 52% of women. The condition typically starts between the 6th to 8th week of pregnancy and is linked to hormonal changes. Risk factors include family history, obesity, and young age at pregnancy. Clinical features include excessive nausea, dehydration, and weight loss. Diagnosis involves blood tests and ultrasound. Treatment includes IV fluids, antiemetics, and monitoring for complications like dehydration and malnutrition. Prevention strategies include early screening and avoiding fatty foods.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Introduction. Introduction. Excessive vomiting during pregnancy. It starts from 6thto 8thweek.
Epidemiology Epidemiology Studies showed that approximately 27 to 30 percent of women experience only nausea, while vomiting may be seen in 28% to 52% percent of all pregnancies.
Pathophysiology Pathophysiology Theories suggest a great role played by levels of hCG and Estrogen .
Risk factors Risk factors Family history Multiple pregnancy Polyhydramnios Prime gravidity Previous history of hyperemesis gravidarum Molar pregnancy Diets rich in fat contents Obesity Young age at pregnancy
Clinical features Clinical features Excessive Nausea and vomiting Features of Dehydration Weight loss
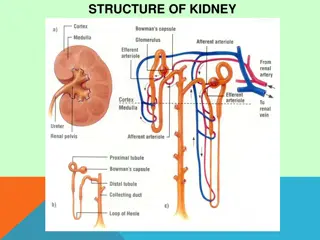
Investigations Investigations Full blood count Renal function test Urinalysis Liver function tests Obstetric ultrasound
Treatment Treatment Put the patient Nil per oral for 24 to 48 hours Urethral catheterization for urine output monitoring Vitamin B1 (IV)100mg 24hourly mix in intravenous rehydration solution AND Metoclopramide (IM) 5 10 mg 8hourly till vomiting stops OR Promethazine (IM) 12.5 mg 12hourly a day
Complications Complications Vitamin B1 deficiency Dehydration Malnutrition Wernicke encephalopathy Esophageal rupture Pneumothorax. Electrolyte imbalances Fetal Complications
Prevention Prevention Proper screening during ANC Avoiding fatty food staffs Early diagnosis and treatment