Guide to Becoming a Credentialed Provider in Tennessee
The State of Tennessee's Department of Intellectual and Developmental Disabilities (DIDD) oversees services for individuals enrolled in various programs and waivers. Learn about the mission, vision, integration goals, funding, and how to apply to become a credentialed provider in Tennessee.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
How to Become a Credentialed Provider Applicant Forum for Potential Providers
Who is DIDD? The State of Tennessee Department of Intellectual and Developmental Disabilities (DIDD) is the state agency responsible for monitoring the services and supports provided to persons enrolled in the Katie Beckett-Part A & B programs and 1915c Waivers. DIDD also serves as the managing authority and credentialing entity as of 7/1/2022 for the following: Katie Beckett Part A & B Employment and Community First Choices (ECF) CHOICES 1915c Waivers
Todays DIDD Vision To support all Tennesseans with intellectual and developmental disabilities to live fulfilling and rewarding lives. Mission To become the nation's most person centered and cost- effective state support system for people with intellectual and developmental disabilities.
1915c Waivers Status As of 2016 the DIDD 1915c waivers were closed for the enrollment of adults with an ID/D diagnoses. To offer a wide selection of long-term support of providers DIDD continues to accept credentialing applications for the 1915c waiver. A referral for ECF CHOICES is now being offered to adults with an ID/DD diagnosis.
Integration Goals Our integration intentions are to achieve a single, seamless, person-centered system of service delivery for people living with an I/DD diagnosis to increase their independence, full participate in their communities, and to achieve their competitive, integrated employment goals. This change will allow DIDD to leverage its expertise and passion in supporting people with I/DD to positively impact all Medicaid-funded programs.
Who Provides Funding and Oversight? Medicaid funding is through the Federal Department of Health and Human Services (DHHS). Federal oversight is provided by the Centers for Medicare and Medicaid Services (CMS) which is a component of DHHS. In Tennessee, state oversight is provided by the Division of TennCare. The Division of TennCare has contracted with DIDD to administer Medicaid Waiver services for persons who have Intellectual / Developmental Disabilities.
Becoming a Credentialed Provider Applicants may submit a Provider Credentialing Application(s) anytime of the year regardless of the programs and services being selected. Before submitting the New Provider Credentialing Application, you are required to register and obtain a Medicaid Identification number via the TennCare Provider Portal. Interested applicants are required to obtain the necessary service license(s) for each service selected prior to submitting a New Provider Credentialing Application. Additional prerequisites are demonstrated on the New Provider Credentialing Application. 7
Title VI Compliance and Tennessee Federal Requirements and Tennessee Law On May 31, 1993, the State of Tennessee became the first state to pass legislation enforcing Title VI compliance in all its departments, programs, and agencies. Accordingly, Tennessee Code Annotated 4-21-904 provides that: It is a discriminatory practice for any state agency receiving federal funds making it subject to Title VI of the Civil Rights Act of 1964 (42 U.S.C. 2000d et seq.), or for any person receiving such federal funds from a state agency, to exclude a person from participation in, deny benefits to a person, or to subject a person to discrimination under any program or activity receiving such funds, on the basis of race, color, or national origin.
Key to Title VI Compliance The Key to Title VI Compliance is to ensure that people receiving services receive: Equal treatment Equal access Equal rights Equal opportunities without regard to the race, color, and national origin, as well as Limited English Proficiency, of the individual.
The Deficit Reduction Act (DRA)
The Deficit Reduction Act (DRA) The Deficit Reduction Act (often referred to as Fraud and Abuse) is a piece of legislation passed by Congress that included provision impacting Federal Health Care Programs. This includes any plan which provides health benefits that are funded by the U.S. Government, or any state health care program defined under section 1320a-7(h). According to Section 6032 of the DRA of 2005, DRA compliance includes educating employees, contractors and agents on the following topics: Requires all entities that receive $5 million or more in annual Medicaid payments to establish written policies that provide detailed information about the Federal False Claims Act. Administrative remedies for false claims and statements. Any civil or criminal penalties under state false claims laws. Whistleblower protections under federal and state law. The role of such laws in preventing and detecting fraud, waste and abuse in federal health care programs.
The Deficit Reduction Act (DRA) The DRA also sets forth the following compliance standards: Background/exclusion checks review: Reviews should be conducted to verify that background checks are completed prior to an employee providing services to members, and exclusion checks are completed on a monthly basis. HCBS provider review: An audit should be conducted to assess compliance of the provider s policies and procedures related to the ECF CHOICES program, employee records and training. To report Fraud and Abuse to TennCare, please contact the Hotline: 1-800-433-3982 or website https://www.tn.gov/tenncare/fraud-and-abuse.html
Home & Community Based Services (HCBS) Final Settings Rule
Centers of Medicaid Services Announcement In January 2014, the CMS announced a requirement for states to review and evaluate current HCBS Settings, including residential and non-residential settings, and to demonstrate compliance with the new federal HCBS Settings rules that went into effect March 17, 2014.
HCBS settings MCO Requirements: o Effective July 1, 2015, Managed Care Organizations (MCOs) are required to verify that HCBS providers are in compliance with the HCBS Settings Rule detailed in 42 C.F.R. 441.301(c) (4)-(5). Provider compliance will be verified during the credentialing process, prior to executing an agreement with a provider and during recredentialing. If a provider is not compliant with the HCBS Settings Rule, The MCO cannot contract with the provider. o The MCO will use the HCBS audit process to monitor compliance with the Settings Rule and will complete HCBS annual audits that include evaluating physical location, policies, procedures, and other written documentation, employee training, and employee files.
Final Rule The final rule addresses several sections of federal law under which states may use federal Medicaid funds to pay for HCBS services. The rule supports enhanced quality in HCBS programs and adds protections for individuals receiving services.
Key Provisions of the Rule Ensures Individual Rights in the least restrictive Environment Integration and access to the community Offers choice of Settings Offers choice of Services and Service Providers Encourages Independence Privacy Dignity Respect Live Work Play
Centers of Medicaid Services (CMS) Intent To ensure that individuals receiving long-term services and supports through HCBS programs under the 1915(c), 1915(i), and 1915(k) Medicaid authorities have full access to the benefits of community living and an opportunity to receive services in the most integrated setting appropriate.
Assessing Initial Compliance DIDD must ensure, prior to contracting with a new credentialed provider and as part of ongoing monitoring of existing providers, that all HCBS settings where Medicaid- reimbursed services are provided are compliant with the CMS HCBS Rule 42 C.F.R. 441.301 (c)(4)-(5) and in accordance with the state s approved transition plan.
Ongoing Compliance Monitoring Mechanisms are in place to monitor ongoing compliance with the rule: Key provisions are embedded in the person-centered planning process and person-centered support plan Key provisions are embedded in Quality Assurance review processes Key provisions are embedded into polices, protocols, and rules Measured through Individual Experience Assessments; required for people supported during the annual planning process and each time there is a residential move
Modifications to the Rule Any departure from the requirements is considered a modification and must be: Supported by specific assessed need, Justified and documented in the person-centered service plan.
HCBS Compliance and Self-Assessment These self-assessments are designed to measure HCBS provider s planned and/or current level of compliance with the HCBS Settings Rule and to provide a framework for assisting interested provider applicants and credentialed providers with the necessary steps to reach and maintain compliance and enhance the quality of HCBS and provide protections to participants: TN Non-Residential Self-Assessment TN Residential Provider Self-Assessment A more complete overview of HCBS Self-Assessment resources are How to Become a Credentialed Provider (tn.gov) How to Become a Credentialed Provider (tn.gov) available for viewing at How to Become a Credentialed Provider (tn.gov)
Application Service Types
New Provider Credentialing Application This application is to be completed by an entity (e.g., individual, group, agency, or other type of organization) seeking to provide services through the KATIE BECKETT (Part A & B) program, 1915c Waiver, the Employment and Community First CHOICES (ECF), and CHOICES program administered by the Department of Intellectual and Developmental Disabilities (DIDD) and the Managed Care Organizations (MCOs). If you are currently contracted as a CHOICES only provider, you must submit a New Provider Credentialing Application to DIDD to expand services to any other waiver services or programs. If you are applying for CHOICES only you will submit an initial credentialing application to the MCO(s) for credentialing.
Service Areas and Credentialing When selecting the region(s) and or county(ies) the applicant shall note the following: Once credentialed the provider will be qualified based on the counties selected in each region as noted on the application for 1915c and Katie Beckett Part B. The MCOs will contract based on network capacity, county and services needed for the ECF, CHOICES and Katie Beckett Part A. An MCO contact is not guaranteed.
Expansion Credentialing Application This application must be completed by an entity (e.g., individual, group, agency, or other type of organization) who is currently contracted through either of the following programs: Katie Beckett- Part A, Katie Beckett- Part B, the 1915c Home and Community Based Services (HCBS) waivers, Employment Community First (ECF) Choices. (Reminder:If the applicant is contracted to provide CHOICES only services a New Credentialing Application is required.) The purpose of the expansion application is to add program(s), service(s), and all regions/counties must be identified. When a provider is solely requesting to add counties to a contracted region(s), please complete the MCO Contract and County Expansion Request Form located on the DIDD website.
IDD Program Integration Contract Structure
Contracted Providers As of July 1, 2022, all credentialed providers are eligible to obtain a contract with a participating Managed Care Organization (MCO); however, as a credentialed provider you will not be guaranteed a contract with any or all the contracted MCOs.
MCO Network An MCO network can be comprised of providers that are contracted for 1915c, *Katie Beckett Part-A & B, ECF Choices and/or CHOICES services. MCOs are required to maintain a network of contracted providers for the ECF Choices, CHOICES and 1915c programs to ensure they can adequately meet the needs of each Member enrolled in an LTSS Program. Katie Beckett Part-A services is contracted exclusively through BlueCare and DIDD credentials the application.
Electronic Visit Verification - EVV
EVV and Services Rendered All services listed below are required to participate via the Electronic Visit Verification EVV process: Personal Assistance, Respite, Supportive Home Care, Clinical Services (Nursing, Behavior services, Physical Therapy, Occupational Therapy, Speech Language and Pathology, and Nutrition) Behavior Supports
EVV and The Provider of Services The provider staff must use an electronic-based system (EVV) that verifies when provider visits occur and documents the precise times services begin and end. The provider is to monitor schedules/visits to ensure the person supported is receiving the approved services and units. Attempts should be made to ensure the person supported receives services if they want them for that day. The provider needs to have a back-up staffing plan in place to address alerts advising a staff person has not shown up for work or cannot work that day.
EVV Confirms Services Rendered The providers EVV system must verify the following: Date of service; Location of service; Individual providing service; Type of service; Individual receiving service; and Time the service begins and ends.
EVV Status Reports DIDD will provide a written status report to providers to allow them to understand their performance relative to the compliance standards using a compliance report that will reflect check-ins and check-outs monthly. Ongoing technical assistance and trainings will be available from DIDD to providers. DIDDwill incorporate a review of a provider s EVV usage for a sample of people supported. This review will occur during the Annual QA survey or FAR review for the provider and coordinated with DIDD program operations.
Process Overview for Providers 1915c & KB-B 1915C and KB-Part - B providers will complete additional requirements in thru their TennCare portal accounts. This step will finalize a 3-way contract with TennCare, DIDD and Provider Agency. After DIDD Provider Contract Agreement has all 3 signatures the provider will receive service codes for billing services and a final Notification Letter. Submits Application to the appropriate region through the DIDD OwnCloud link imbedded in the application(s) DIDD OBS may assist the applicant to get processed thru TennCare Provider Data Management System Provider Registration Portal/PDMS Application is processed: Additional information may be requested from the applicant as needed via an email Request for Clarification (RFC). Contracted providers may begin advertising their 1915c and Katie Beckett-B services. Completed applications are presented to the Regional Quality Management Committee (RQMC) for review and input A Fact Sheet with a list of the credentialed services is sent to the DIDD Office of Business Services (OBS), Regional Director, et. al. Final Disposition(s): Credentialed Closed Denied Applications reviewed by the Provider Development Committee (PDC) for final disposition. 38
Process Overview for Providers ECF Choices & CHOICES The applicant is now able to reach out to the specific MCO to discuss a contract agreement. An MCO Contract Agreement is not guaranteed. A Notification letter is sent to the Applicant and MCOs. This Notification letter illustrates the waivers and services approved for implementation. Submits Application to the appropriate region through the DIDD OwnCloud link imbedded in the application(s) Final Disposition(s): Credentialed Closed Denied Application is processed: Additional information may be requested from the applicant as needed via an email Request for Clarification (RFC). Completed applications are presented to the Regional Quality Management Committee (RQMC) for review and input Applications reviewed by the Provider Development Committee (PDC) for final disposition. 39
Application Disposition Application Disposition Outcomes: Credentialed The applicant is eligible for contract. Closed The applicant failed to respond to a Request for Clarification (RFC) Letter Denied The applicant failed to meet credentialing requirements. Incomplete The applicant is missing significant information., e.g. service licenses, Medicaid ID, the majority of supporting documents, and many prerequisites Withdrawn - The applicant requested to closed the application.
Additional Resources Tennessee Division of TennCare General Rules Social Security Act: Section 1915 (c) Home-and Community- Based Waivers Tennessee State Code Annotated: Title 33 The Code of Federal Regulations Title 42 Public Health Chapter IV Section 441.300 Health Insurance Portability and Accountability Act (HIPAA) Tennessee Department of Health Rules Resources Title VI 42
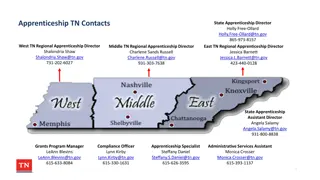
Office Contacts Middle Regional Office Stamps Building, 2nd Floor 291 Stewarts Ferry Pike Nashville, TN 37214 DIDD Central Office UBS Tower, 8th Floor 315 Deaderick St. Nashville, TN 37243 East Regional Office 520 West Summit Hill Drive, Suite 201 Knoxville, TN 37902 West Regional Office 11437 Milton Wilson Rd Arlington, TN 38002 Karen Johnson, Provider Development Coordinator Phone: 615-231-5021 Lori Kieffer, Provider Enrichment Coordinator Phone: 865-594-9296 Email: Lorene.M.Kieffer@tn.gov Linda Hall, Provider Development Coordinator Phone: 901-745-7553 Email: Linda.Hall@tn.gov Sandra Wise, Director of Provider Credentialing and Network Management Phone: 615-741-6159 Lorene.M.Kieffer@tn.gov Linda.Hall@tn.gov Email: Karen.Johnson@tn.gov Email: Karen.Johnson@tn.gov Janelle Weaver, Provider Credentialing Support Phone: 615-231-5094 Email: Janelle.Weaver@tn.gov Martha Adcock, Provider Development/Credentialing Support Phone: 615-231-5361 Email: Martha.Adcock@tn.gov KaRae Frierson, Director of Operations Phone: 615-231-5516 Email: KaRae.Frierson@tn.gov Latisha Dorton, Provider Credentialing Specialist Phone: 865-594-7146 Email: Latisha.Dorton@tn.gov Email: Email: Sandra.Wise@tn.gov Sandra.Wise@tn.gov Tamika Anderson, Provider Credentialing Support Phone: 901-371-3019 Email: Tamika.Anderson@tn.gov Denise Kirk, Director of Operations Phone: 901-745-7701 Email: Denise.Kirk@tn.gov Latisha.Dorton@tn.gov Linda Maurice, Statewide Provider Enrollment Coordinator Phone: 615-532-6568 Email: Janelle.Weaver@tn.gov Tamika.Anderson@tn.gov Carmel Beatty, Deputy Director Phone: 865-594-9339 Email: Carmel.Beatty@tn.gov DIDDProvider.Application@tn.gov DIDDProvider.Application@tn.gov Carmel.Beatty@tn.gov Martha.Adcock@tn.gov Denise.Kirk@tn.gov KaRae.Frierson@tn.gov
Thank you for attending the Applicant Forum Refer to the How to Become a Credentialed Provider website at: How to Become a Credentialed Provider (tn.gov) to obtain all necessary resources to complete the application process including but not limited the following: 1. Applications 2. Available service rates 3. HCBS Settings Rule 4. Minimum Required Policies & Review Guidelines 5. Service definitions 6. Service License requirement FINAL 7/28/2022 Revised 1/20/2023 Revised 2/21/2023 44