Gonorrhea Diagnostic Methods and Tests Overview
Dr. Mohammad Ahmad El Khayyat, an Assistant Professor in Dermatology, STDs, and Andrology, details the diagnostic methods and tests for gonorrhea. Various tests including Gram stain, culture, antigen detection tests, and nucleic acid amplification tests are discussed, highlighting sensitivity and specificity rates for each method. The importance of Gram stain in diagnosing gonorrhea in symptomatic male urethritis is emphasized, while limitations in other infections are noted. The culture test is described, outlining its requirements and applications, especially in cases of suspected sexual abuse. The specificity, cost, personnel requirements, and presumptive identification associated with culture testing are also touched upon.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Gonorrhea (Part II) Dr. Mohammad Ahmad El Khayyat Assistant Professor in Dermatology, STDs & Andrology Faculty of Medicine - Minia University
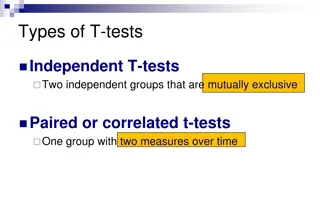
GC DIAGNOSTIC METHODS Gram stain smear Culture Antigen Detection Tests: EIA (enzyme immunoassay) & DFA (Direct fluorescent antibody) Nucleic Acid Detection Tests Probe Hybridization Nucleic Acid Amplification Tests (NAATs) Hybrid Capture
GONORRHEA DIAGNOSTIC TESTS Sensitivity Specificity 95% Gram stain 90-95% (male urethra exudate) DNA probe 95% 99% 98% 85-90% Culture 80-95% 90-95% NAATs
GC GRAM STAIN In symptomatic male urethritis: >95% sensitivity and specificity: reliable to diagnose and exclude GC In cervicitis: 50-70%sensitivity, 95% specificity Not useful in pharyngeal infections Accessory gland infection: similar to male urethritis Proctitis: similar to cervicitis
GRAM STAIN FOR GC: URETHRAL SMEAR Numerous PMNs Gram negative intracellular diplococci
- Sensitivity reduced in asymptomatic infections - Less that 50% sensitive as cell culture - Not useful in rectal infections
GRAM STAIN FOR GC: CERVICAL SMEAR PMN with Gram negative intracellular diplococci
GC CULTURE Requires selective media with antibiotics to inhibit competing bacteria (Modified Thayer Martin Media, NYC Medium) Sensitive to oxygen and cold temperature Requires prompt placement in high-CO2 environment (candle jar, bag and pill, CO2 incubator) In cases of suspected sexual abuse, culture is the only test accepted for legal purposes
- High degree of specificity - Expensive - Trained personnel - Media requirements - Presumptive identification
GC CULTURE SPECIMEN STREAKING CERVICAL AND URETHRAL
Antigen Detection and Enzyme Immunoassays - This type of screening is of little use in diagnosing gonorrhea - This is due to the antigenic variation seen in Neisseria gonorrhoeae and therefore a great enough immune response is not activated to test for antigens specific to N. gonorrhea. - less reliable at detecting asymptomatic infections.
DNA Probe Hybridization - Specific chemiluminescent label on probe - Available commercially - 85% sensitivity - 99% specificity - But over night
Nucleic Acid-Based Amplification Assays (NAAT) - 95% accurate - False positives due to specimen cross-contamination, environmental contamination
TREATMENT FOR UNCOMPLICATED INFECTIONS OF THE CERVIX, URETHRA, AND RECTUM Cefixime 400 mg Orally Once or Ceftriaxone 125 mg IM Once or 1Ciprofloxacin 500 mg Orally Once or 1Ofloxacin 400 mg Orally Once or 1Levofloxacin 250 mg Orally Once 1 Contraindicated in pregnancy and children.
Management CO-TREATMENT FOR CHLAMYDIA TRACHOMATIS If chlamydial infection is not ruled out: Azithromycin 1 g Orally Once or Twice a day for 7 days Doxycycline 100 mg Orally
SPECIAL CONSIDERATIONS: PREGNANCY - Pregnant women should NOT be treated with quinolones or tetracyclines - Treat with alternate cephalosporin - If cephalosporin is not tolerated, treat with spectinomycin 2 g IM once
GONORRHEA TREATMENT NEONATES Prophylaxis for maternal GC infection: Ceftriaxone 25-50 mg/kg IV or IM x 1 NTE 125 mg Disseminated Gonococcal Infection: Ceftriaxone 25-50 mg/kg/d IV or IM x 7 d (use 50 mg/kg/d for older children, treat for 10-14 d if child weighs 45 kg) Cefotaxime 25 mg/kg IV or IM q12h x 7 d
GONORRHEA TREATMENT NEONATES Ophthalmia neonatorum prophylaxis: Silver nitrate 1% aqueous solution topical x 1 Erythromycin 0.5% ointment topical x 1 Tetracycline 1% ointment topical x 1 Ophthalmia neonatorum treatment: Ceftriaxone 25-50 mg/kg IV or IM x 1 NTE 125 mg
GONORRHEA TREATMENT CHILDREN Uncomplicated genital infection: 45 kg: same as adults 45 kg: ceftriaxone 125 mg IM x 1 (alternative spectinomycin 40 mg/kg IM x 1) Disseminated Gonococcal Infection: Ceftriaxone 25-50 mg/kg/d x 7 d Use 50 mg/kg/d for older children Treat for 10-14d if child weighs 45 kg
DGI TREATMENT INITIAL IV THERAPY Begin IV therapy for 24-48 hrs, switch to oral therapy for a total of 1 week Recommended regimen: Ceftriaxone 1g IV or IM q 24 h Alternative Regimens: Cefotaxime 1 g IV q 8 h Ceftizoxime 1 g IV q 8 h Ciprofloxacin 400 mg IV q 12 h Ofloxacin 400 mg IV q 12 h Levofloxacin 250 mg IV q 24 h Spectinomycin 2 g IM q 12 h
DGI TREATMENT SUBSEQUENT ORAL THERAPY Oral therapy for total treatment of 1 week: Recommended Regimes: Cefixime 400 mg PO BID Ciprofloxacin 500 mg PO BID Ofloxacin 400 mg PO BID Levofloxacin 500 mg PO QD
IN CASE OF ALLERGY, INTOLERANCE AND ADVERSE REACTIONS: Allergic reactions to first generation cephalosporins -> <2.5 % of persons with a history of penicillin allergy and are uncommon to 3rd generation cephalosporins Dual treatment with single doses of oral gemfloxacin 320mg plus oral azithromycin 2gm or Dual treatment with single dose of intramuscular gentamicin 240 mg plus oral azithromycin 2gm
GC ANTIMICROBIAL RESISTANCE Resistance in 20%-30% of gonococcal isolates tested in U.S. Plasmid mediated B - Lactamase production Chromosomal mediated Confers resistance to PCN, tetracycline, spectinomycin, erythromycin, fluoroquinolones, and/or cephalosphorins
FOLLOW-UP - A test of cure is not recommended if a recommended regimen is administered. - If symptoms persist, perform culture for N. gonorrhoeae and any gonococci isolated should be tested for antimicrobial susceptibility.
SCREENING Pregnancy A test for N. gonorrhoeae should be performed at the first prenatal visit for women at risk or those living in an area in which the prevalence of N. gonorrhoeae is high. Repeat test during the 3rd trimester for those at continued risk. Other populations can be screened based on local disease prevalence and patient s risk behaviors.
PARTNER MANAGEMENT Evaluate and treat all sex partners for N. gonorrhoeae and C. trachomatis infections if contact was within 60 days of symptoms or diagnosis. Avoid sexual intercourse until therapy is completed and both partners no longer have symptoms.
GC PREVENTION STRATEGIES Health promotion, education & counseling Increased access to condoms Early detection through screening in selected high risk populations Effective diagnosis & treatment Partner management Risk reduction counseling
THANK YOU THANK YOU