Effective Communication in Discussing Life-Sustaining Treatments
Enhance your skills in discussing life-sustaining treatments with patients by following the REMAP framework. Learn how to reframe conversations, expect emotions, map out priorities, align with patient values, and plan treatments that match values. Discover strategies for addressing unclear plans, assessing readiness, providing relevant information, offering recommendations, resolving inconsistencies, and gaining consent for the treatment plan.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Goals of Care Conversations Part 4 Discussing Life-Sustaining Treatments
Serious Illness Communication Skills Training Delivering Serious News Conducting Goals of Care Conversations Part 1 - Reframing: We re in a Different Place Part 2 - Mapping the Future: Clarifying Priorities Part 3 - Aligning with Patient Values Part 4 - Discussing Life-Sustaining Treatments
Life Life- -Sustaining Treatments Sustaining Treatments Artificial nutrition Artificial hydration Mechanical ventilation invasive and non-invasive Others, e.g., dialysis, blood products Transfers to the hospital, ICU CPR
Review: REMAP Review: REMAP R Reframe E Expect emotion M Map out what s important A Align with patient values P Plan treatment to match patient values
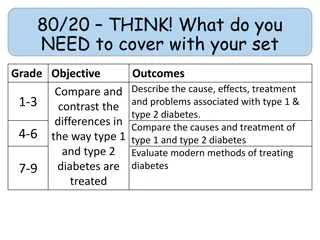
What We Will Learn What to do if mapping and aligning do not point to a clear plan about life-sustaining treatment
REMAP: Plan REMAP: Plan Treatments that Match Values Treatments that Match Values AFTER mapping what s important and aligning with the AFTER mapping what s important and aligning with the patient s values patient s values: : If goals point to a clear plan about life If goals point to a clear plan about life- -sustaining treatment , make a recommendation make a recommendation sustaining treatment ,
REMAP: Plan REMAP: Plan Treatments that Match Values Treatments that Match Values AFTER mapping what s important and aligning with the AFTER mapping what s important and aligning with the patient s values patient s values: : If goals do not point to a clear plan about life-sustaining treatment, or if more information is desired by the patient: 1. Assess understanding of and readiness to discuss LSTs 2. Assess and provide desired information 3. Ask whether the patient wants a recommendation about LSTs or they want to express their preferences 4. Explore inconsistences between goals and LST decisions 5. Summarize and gain consent for the plan
How We Will Learn Define skills Observe skills in action Practice
What are some unintended consequences of the following? Would you like us to try to restart restart your heart? Would you like us to do everything possible your father s heart stops beating and he stops breathing? everything possible if I think it s time to withdraw care withdraw care.
What are some unintended consequences of the following? Would you like us, in what would naturally be your final moments, to press on your chest and break your ribs, shove a tube down your throat and poke you with needles in lots of places in a chaotic attempt that has a very small chance of giving you more time to be technically alive but unlikely to ever return to meaningful communication with others? http://www.cunniffdixon.org/resource/do-not-punctuate-the-end-of-your-life-with-a-senseless-act-of-brutality-2/
Our role Ensure patients receive treatment consistent with their values and goals by helping them Define what is important to them Understand the possible outcomes of treatment Make informed decisions to support their goals
Assess Understanding and Readiness Assess Understanding and Readiness Would you want CPR if your heart stops beating? VERSUS VERSUS Tell me what you know about CPR.
Assess Understanding and Readiness Assess Understanding and Readiness Tell me what you know about [this LST]. Allows the clinician to: Determine the patient s readiness to discuss the treatment Assess patient s understanding of the treatment Provide helpful information before asking the patient to make a choice
Provide Information Provide Information If the patient does not have a basic understanding of the treatment, provide information Be clear and direct; avoid medical jargon Give 1-2 pieces of information at a time, then stop and wait for the patient to respond
One Year Survival Rates After In Hospital CPR One Year Survival Rates After In Hospital CPR Peberdy MA, Kaye W, Ornato JP et al. Cardiopulmonary Resuscitation of Adults in the Hospital: A Report of 14 720 Cardiac Arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation 2003; 58: 297-308. Chan PS, Nallamothu BK, Krumholz HM, et al. Long-Term Outcomes in Elderly Survivors of In-Hospital Cardiac Arrest. N Engl J Med 2013; 368:1019-1026.
Cognitive Status After CPR for Age 65+ Cognitive Status After CPR for Age 65+ Peberdy MA, Kaye W, Ornato JP et al. Cardiopulmonary Resuscitation of Adults in the Hospital: A Report of 14 720 Cardiac Arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation 2003; 58: 297-308
Make a Recommendation (with permission) Make a Recommendation (with permission) Some patients want a recommendation; others do not Asking permission shares control of the conversation with the patient and demonstrates respect If the patient wants a recommendation, state how it is related to the patient s goals
Explore Inconsistencies Between Goals and Explore Inconsistencies Between Goals and Tx Tx Decisions Decisions If decisions about life-sustaining treatments appear inconsistent with the patient s goals: I worry that CPR won t help you reach your goals Tell me more about what you are hoping for with [intervention X]. Is there a situation you could imagine when you [would/would not] want [intervention X]?
Respond to Emotion with Empathy Respond to Emotion with Empathy These decisions can be emotional Attend to emotion BEFORE moving on to anything else Do not respond to feelings with facts respond with empathy See Empathic Responses handout
Summarize and Confirm the Plan Summarize and Confirm the Plan To ensure shared understanding, summarize and confirm the plan Review next steps Write orders in the record Follow-up and/or consults for needed services (if applicable)
Reviewing Goals and Decisions Later Reviewing Goals and Decisions Later Once life-sustaining treatment decisions have been made and documented in the record, it may be appropriate to review them on occasion. The situation may call for: Revisiting (and reframing if necessary) when goals and decisions may be changing -> REMAP Reviewing goals and decisions without casting doubt
Review / Verify Decisions Without Casting Doubt Review / Verify Decisions Without Casting Doubt When your mother met with Dr. Jones about two months ago, she knew her illness was getting worse, and she said it was her goal to stay as comfortable as possible. She wanted medical orders written to avoid being placed on a breathing machine and to avoid CPR. Those orders were written then, and they are in place so everyone will know to honor her wishes. Is there anything more you can share to help us respect her decisions?
Drill Instructions Drill Instructions Review drill as a group Divide into pairs to practice the drill Practice the drill (person with bigger feet goes first) Switch roles Debrief with one another: How did it feel to say the words? One thing clinician noticed One thing patient noticed
Drill A: Introduction Drill A: Introduction Clinician Patient I want to be sure you get the care that helps achieve your goals. It s helpful to know in advance whether you would or wouldn t want certain treatments. One of those treatments is CPR. Is it OK if we talk about this now? Sure.
Drill A: Assess Understanding and Readiness Drill A: Assess Understanding and Readiness Clinician Patient Can you tell me what you know about CPR? No one has really told me about it. I ve seen it on TV, but I don t know that much about it.
Drill A: Provide Information Drill A: Provide Information Clinician CPR is used only when someone s heart and breathing have stopped. Sometimes the heart and breathing stop as a natural part of the dying process. Other times it happens unexpectedly. CPR involves forcefully pushing on the chest. It can also include shocking the heart and putting a tube down the throat to try to get the heart and breathing to start again.
Drill Instructions: Swap Roles Drill Instructions: Swap Roles Drill Instructions Patient Clinician
Drill: Debrief Drill: Debrief How did it feel to say the words? One thing clinician noticed One thing patient noticed
Drill B: Assess Information Desired Drill B: Assess Information Desired Clinician Patient I thought CPR usually works to save people s lives. It doesn t? Would it be helpful to know how many people survive after receiving CPR and what the risks might be? Or is there other information that might be helpful?
Drill B: Provide Desired Information Drill B: Provide Desired Information Clinician Patient Most adults who receive CPR don t survive. Young and otherwise healthy people have better chances of surviving, and people with serious health problems have lower chances. What do you think my chances are?
Drill B: Provide Desired Information Drill B: Provide Desired Information Clinician Patient About 17 of 100 people survive after receiving CPR in the hospital, which means that 83 out of 100 people die. These are averages. Unfortunately, for people with health problems like yours, the chances of survival are [much lower] lower]*. *customize per patient s risk using general terms Wow, that s a lot different than I expected. [much
Drill B: Provide Desired Information Drill B: Provide Desired Information Clinician It can be surprising. You mentioned that it s important for you to be able to [be family]* family]*. There s a [small chance [small chance]** recognize them if you survived after CPR. Also, there is a high risk of broken ribs, and a [large chance [large chance]** ]** that you would need more help. You might not be able to go back home to live by yourself. *customize to patient s goals **customize per patient s risk using general terms [be with your with your ]** that you wouldn t be able to
Drill Instructions: Swap Roles Drill Instructions: Swap Roles Patient Clinician
title Drill: Debrief Drill: Debrief How did it feel to say the words? One thing clinician noticed One thing patient noticed
Drill C: Ask Permission to Make Recommendation Drill C: Ask Permission to Make Recommendation Clinician Patient I guess I d like to hear what you think. Would you like me to make a recommendation about CPR, or would you prefer to let me know your thoughts?
Drill C: Explore Inconsistencies Drill C: Explore Inconsistencies Clinician Patient Based on your goals to [stay at home with your family, be able take care of yourself, and not be stuck in the hospital]*, I would not recommend CPR. Does that sound right to you? I think I would still want CPR. *customize to patient s goals using their words
Drill C: Explore Inconsistencies Drill C: Explore Inconsistencies Clinician Patient I guess at this point I still feel like I would want to give CPR a try, even though it probably won t work, or I might have problems afterward. I might be that rare person who makes it through! I worry CPR won t help you reach your goals.
Drill C: Explore Inconsistencies Drill C: Explore Inconsistencies Clinician Patient Can you think of a situation when you wouldn t want CPR? If I couldn t recognize my family or make decisions for myself, at that point I wouldn t want CPR. That s very helpful to know. Let s make sure [your surrogate] knows what you want.
Drill C: Summarize and Confirm Plan Drill C: Summarize and Confirm Plan Clinician Patient So it sounds like you would want CPR if your heart and breathing stop. Do I have that right? Yes, that s right. Ok, I ll put that in your health record. And we ll talk with [your surrogate] together to make sure they know that you wouldn t want CPR if you couldn t recognize your family or make decisions for yourself. Is that ok? That sounds good.
Drill Instructions: Swap Roles Drill Instructions: Swap Roles Patient Clinician
Drill: Debrief Drill: Debrief How did it feel to say the words? One thing clinician noticed One thing patient noticed
Putting It All Together Drill Instructions Putting It All Together Drill Instructions Review drill as a group Divide into pairs to practice the drill Practice the drill (person with bigger feet goes first) Switch roles Debrief with one another: How did it feel to say the words? One thing clinician noticed One thing patient noticed
Drill Instructions: Swap Roles Drill Instructions: Swap Roles Patient Clinician
Drill: Debrief Drill: Debrief How did it feel to say the words? One thing clinician noticed One thing patient noticed
What surprised you? What do you want to take forward? Anywhere you might get stuck?
Goals of Care Conversations Goals of Care Conversations training materials were developed and made available for public use through U.S. Department of Veterans Affairs contracts with VitalTalk [Orders VA777-14-P-0400 and VA777-16-C-0015]. Materials are available for download from VA National Center for Ethics in Health Care at www.ethics.va.gov/goalsofcaretraining.asp. Published Jan. 2017