Chemical Pathology Overview: Thyroid, Pituitary, Adrenals & Metabolic Disorders
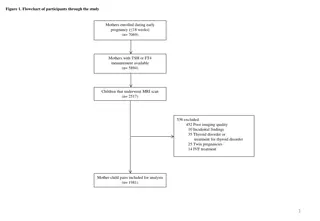
This talk by Dr. Vlad Makeev provides an overview of important topics in chemical pathology, including thyroid, pituitary, adrenals, enzymes, and metabolic disorders. It covers essential physiology concepts, structured examination approaches, and aims to enhance comfort with pathology. Learning objectives encompass various hormonal, metabolic, and physiological aspects related to endocrine and metabolic health.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Chem Path 2 Pituitary, thyroid, adrenals, enzymes and metabolic disorders Dr Vlad Makeev
The purpose of this talk 1. Give you an overview of the important topics regarding to some (not all) of chemical pathology 2. Revise some basic physiology relevant to the above 3. Emphasise the concept of a structured approach to examination answers 4. Hopefully make you feel more comfortable with pathology in general This talk will not: Provide intense details on all pathology pertaining to a particular topic Provide you with every bit of information you need to get a distinction Cover the minutiae
Outline 2 sections with questions at the end of each section Section 1 Thyroid Pituitary Section 2 Adrenals Diabetes Metabolic disorders
Learning objectives Anterior pituitary hormones: recall the six anterior pituitary hormones and explain the hypothalamic factors responsible for their control Plasma protein function: summarise the functions of commonly measured plasma proteins and explain factors that contribute to their concentration Cori cycle: explain the Cori cycle Insulin: explain the synthesis, storage, secretion and physiological actions of insulin incl. the role of c-peptide, and homeostatic mechanisms of control Glucose homeostasis: explain the factors regulating blood glucose incl. counter-regulatory mechanisms Porphyrine metabolism: summarise the principles of porphyrine metabolism Adrenal physiology: summarise adrenal function, histology, microanatomy and zonation Cholesterol and lipoprotein metabolism: summarise cholesterol and lipoprotein metabolism and explain the link between lipid disturbance and cardiovascular disease Renal physiology: define glomerular filtration rate (GFR) and compare different methods of GFR assessment Renal physiology: explain why serum creatinine alone is a poor marker of absolute kidney function, and why a normal serum creatinine does not mean that renal function is normal Thyroid physiology: summarise thyroid physiology Energy metabolism: summarise energy metabolism incl. protein, lipid and carbohydrate metabolism Purine metabolism: summarise the basics of purine metabolism Enzymes: summarise the roles of enzymes in body metabolism and recognise the effect of organ-specific/biochemical disease on plasma levels of enzymes and subsequent outcomes Therapeutic drug monitoring: interpret the factors affecting serum levels for a given dose (pharmacokinetics) and those factors affecting response to a drug at its active site (pharmacodynamics) Therapeutic drug monitoring: explain the concept of a therapeutic range and demonstrate awareness of its limitations Therapeutic drug monitoring: list examples of drugs which require measurement of levels, for therapeutic and toxic reasons e.g. anticonvulsants, lithium, digoxin and theophylline Metabolic disorders and screening: recognise how prevalence, predictive values, sensitivity and specificity relate to disease and diagnostic tests of disease Metabolic disorders and Screening: demonstrate awareness of current UK screening for inherited metabolic disorders and future prospects incl. Phenylketonuria (PKU)
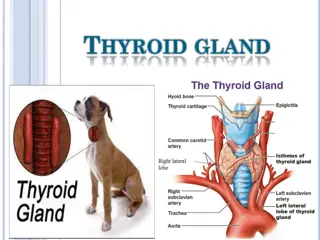
Thyroid Thyroxine is important for: Regulating basal metabolic rate Potentiating responses to catecholamines
Hypothyroidism Aetiology Autoimmune Primary atrophic (no goitre) Hashimoto s (goitre and anti-TPO/TG) Other Iodine deficiency Surgery/radioactive ablation Drugs: amiodarone, lithium, carbimazole Symptoms/Signs Weight gain Cold intolerance Depression Dry skin Hair loss Fatigue Constipation Bradycardia
Hypothyroidism Investigations: Bloods including TSH and T4 Addition of other hormone panels if indicated Imaging is in the form of central if ?secondary disease Management Oral levothyroxine Titrate to normal TSH with 6 weekly check ups until stable Ensure no signs of over- replacement - palpitations Higher doses may be needed in pregnancy, nephrotic syndrome I.V Liothyronine Only for Myxoedema coma
Additional thyroid states Sick euthyroid Subclinical hypothyroidism Pre-hypothyroid Pituitary gland can compensate High TSH, normal T3/4 If positive anti TPO Ig then higher risk of hypothyroidism later Severe illness Body tries to shut down metabolism To conserve energy Low T3 and T4 Initially high TSH, then low TSH Have similar TFTs Only way to differentiate is based on clinical picture
Hyperthyroidism Aetiology Autoimmune - Graves De Quervain s Neoplasm - Thyroid adenoma Drug induced - Amiodarone Toxic multinodular goitre Postpartum Symptoms / Signs: Weight loss Irritability Heat intolerance Palpitations Increased appetite Goitre Graves specific Pretibial myxoedema, graves orbitopathy Investigations: Bedside - ECG (?AF) Bloods - U+Es, TFTs, antibodies Anti-TSHR) Basic imaging USS Advanced imaging Thyroid uptake scan (radiolabelled iodine)
Hyperthyroidism Management Conservative Smoking cessation Medical Carbimazole or Propylthiouracil Titrate or block & replace Tx Usually for 18 months Beta-blockers Lugol s iodine Radio-iodine Surgical Hemi/Total thyroidectomy Must be euthyroid before surgery
Pituitary mass Pituitary adenoma Macroadenoma >1cm Usually non-functional Occasionally can be associated with hyperprolactinaemia Microadenoma More likely to be functional GH or Prolactin secreting Lead to Acromegaly Symptoms: Bitemporal hemianopia Prolactin related: Galactorrhoea, Gynaecomastia, Oligo/amenorrhoea, loss of libido, Impotence. Somatotrophin related Acromegaly - Soft tissue growth (Hands, feet, tongue), Organomegaly, Symptoms of heart failure, hypertension, Diabetes Carpal tunnel
Pituitary mass Investigation: Imaging Acromegaly Glucose tolerance test Measurement of GH Plasma IGF-1 Prolactinoma Serum prolactin levels (>6000) Management: Medical Octreotide (Somatostatin analogue) Cabergoline or bromocriptine (Dopamine agonist) Pegvisomant (GH Receptor antagonist) Radiotherapy Surgical Trans-sphenoidal debulking Monitoring Serum GH / Prolactin levels Bowels (acromegaly)
Thyroid tumours Commonest: papillary Then: follicular Good prognosis 5% medullary C-cells that produce calcitonin Linked to MEN2 (see histo) Lymphoma Risk in Hashimoto s Anaplastic Elderly, undifferentiated Poor prognosis Papillary & Follicular Surgery +/- radio-iodine Replace thyroxine to completely suppress TSH Monitor thyroglobulin levels Psammoma body 1 3 Klatt, E., Robbins, S. and Cotran, R. (2015). Robbins and Cotran atlas of pathology. Philadelphia: Elsevier/Saunders.
The (anterior) Pituitary Laycock and Meeran 2012
Hypopituitarism Aetiology: Malignancy Pituitary adenoma* Craniopharyngioma Weird & Wonderful Infection TB Syphilis Infiltration Sarcoid Lymphoma Iatrogenic Surgical / Traumatic / radiation Infarct Sheehan s or Apoplexy Tertiary (rare!) Symptoms/signs: Generic Sex hormones Impotence (men) Loss of libido Oligo/amenorrhoea ACTH Addisonian crisis TSH Myxoedema coma Lethargy Weight gain Hypotension Hair loss Myalgia
16 CPFT: combined pituitary function test Give a patient GnRH, TRH and insulin Measure levels of pituitary hormones every 30 mins for 2h GH Cortisol TSH LH FSH Prolactin Check to see if an adequate response FSH/LH only applicable after puberty Poor response can indicate hypopituitarism NB: Acromegaly needs an oral glucose tolerance test to diagnose Measurement of IGF-1 is sensitive but not specific Various normal ranges
Hypopituitarism Investigation Screening 9am cortisol / salivary cortisol TFTs Serum testosterone/oestrogen Combined pituitary function test Administer LHRH + TRH + Induce hypoglycaemia Measure LH, FSH, TSH, ACTH and growth hormone for 2 hours at half hourly increments Imaging CT/MRI Management Replacement of end hormones - much cheaper and easier to control Hydrocortisone No need for fludrocortisone Thyroxine Oestrogen / Testosterone Cause specific Adenoma Next section Infiltration Steroids Infection Antibiotics as needed
28/02/2025 18 Halfway questions and break Mentimeter Code 4272 1861 Feedback link: https://forms.office.com/r/VYYRE 1Wxmt
28/02/2025 19 Answers A woman has diarrhoea, sweating, fever and palpitations for the last week. Bloods show low TSH and high thyroxine. She does not have good uptake on technetium scan. De Quervain s Thyroglobulin Which blood marker is monitored to check for recurrence of papillary thyroid carcinoma post resection? Anti TG and TPO What antibodies are tested for in the laboratory diagnosis of Hashimoto's thyroiditis? Carbimazole Which medication is used for hyperthyroidism?
28/02/2025 20 Answers Commonest cause of hypothyroidism in the UK? Hashimoto s Commonest thyroid cancer? Papillary (memory aid: papillary = popular)
28/02/2025 21
Adrenals The adrenal gland is divided into zones which provide different steroid hormones: Glomerulosa - Mineralocorticoids (Aldosterone) Fasciculata - Glucocorticoids (Cortisol) Reticularis - Sex hormones Medulla Catecholamines the closer to the middle, the sweeter it gets
Addisons Aetiology: Primary Iatrogenic Autoimmune TB Infarct Malignancy Secondary Pituitary Signs/Symptoms: Postural symptoms Weight loss, anorexia Fatigue Vomiting, salt craving Skin/Mucosal pigmentation (*) *Schmidt s Syndrome
24 Management Hydrocortisone Sick day rules Fludrocortisone Investigations: 9am Cortisol (>350 excludes addisons) Electrolytes (Hyponatraemia, Hyperkalaemia). Serum ACTH Check glucose Synacthen test Synthetic ACTH administered IV/IM Cortisol readings at 0, 30, 60 Only rises in secondary disease
Cushings Aetiology Primary Adrenal malignancy Secondary Pituitary adenoma Ectopic/Paraneoplastic ACTH (SCC Lung Ca) Iatrogenic Investigations Dexamethasone suppression Low dose - confirms Cushing s syndrome High dose - Helps to determine Cushing s syndrome from disease Imaging CT CAP / Adrenals MRI pituitary Management Primary Adrenalectomy +/- steroid replacement *Nelson s syndrome Pituitary adenoma Mx Ectopic - Cancer Mx Ketoconazole / Metyrapone / Mifepristone
Conns Aetiology Adrenal hyperplasia Adrenal adenoma / carcinoma Symptoms/Signs Treatment resistant hypertension Hypokalaemia Hypernatraemia Investigations Bloods - electrolytes, plasma aldosterone:renin ratio (raised) Adrenal vein sampling Imaging Treatment: Aldosterone antagonists Surgery
27 Conn s and Phaeos Phaeochromocytoma Conn s syndrome Pulses of hypertension, arrhythmias, sweats Adrenal hyperplasia or tumour Hypertension High sodium, low potassium Measure 24h urine catecholamines Formerly vanillylmandelic acid (VMA) Measure aldosterone:renin ratio High in Conn s syndrome Adrenal medulla tumour : adrenaline Peripheral neural tumour : noradrenaline Treat with spironolactone and possibly adrenalectomy
Phaeochromocytoma Associated with: MEN-2(A/B) NF-1 VHL Symptoms/Signs: Episodes of impending doom /Panic Resistant hypertension Investigations Urinary/Plasma nor/metanephrines False positives - TCAs, CCBs, Beta-blockers Imaging Management Alpha blockade Phenoxybenzamine Beta blockade Surgery
2 x P 1 x M 3 x P 1 x P 3 x M Wikipedia
Diabetes Feature Type I Type II Habitus Plasma insulin B cell function B cell antibodies Lean Low Absent Present [ICA, IAA, GADA, IA-2A] Absent [usually] Yes Yes 0.25% DR-3 or 4 Europeans Young / Adolescent (can be old LADA) Acute Obese Variable Present Absent Family history Ketosis prone Weight loss Prevalence HLA associations Ethnicities Age Present [usually] No No 4-7% None Asian, African Middle age (Can be and is increasing in young) Gradual Onset
Diagnosis Pre-diabetes Diabetes Fasting blood glucose 6.1-6.9 >7 OGTT 7.8-11 >11.1 HbA1c 42-47 >48 (6.5%) Random BM 7.8 - 11 >11.1 Diagnosis = symptomatic + one of the above test being positive Be wary in using HbA1c
Management Type 1 Conservative Lifestyle advice (alcohol) Diabetes nurse review Dietary advice Medical Insulin Basal bolus Insulin pump Biphasic OD/BD Metformin if BMI >25 Surgical SPK (Single pancreas kidney transplant) Type 2 Conservative Diet + Lifestyle advice Exercise Medical 1. Metformin 2. Add one of: a. Sulphonylurea b. DPP-4 agonists c. SGLT-2 inhibitors 3. Add GLP-1 antagonist or two of above 4. Insulin Surgical Bariatric surgery
Hyperglycaemic hyperosmolar state (HHS) Predominantly type II diabetics Insulin resistance causing persistent hyperglycaemia Osmotic diuresis results Takes days to fully develop Presents as: Confusion Clinically very dehydrated (Patients lose up 10-20% of body weight in water) Investigations: Raised serum osmolality (>320) Glucose >30 NO ketones / acidosis Treatment: 1. IV Fluids a. Aim +3-6L/24h b. NaCl +/- KCl 2. Monitoring a. Electrolytes (Na, K) i. Beware of rapidly over- correcting hypernatraemia b. BMs + Ketones i. BMs should fall at around 5mM/h c. Neurological status 3. Insulin (0.05u/kg FRII) a. Only needed if Ketones rising or if BMs no longer falling with just fluids
DKA Predominantly type I diabetics A state of absolute insulin deficiency regardless of whatever insulin is present in the body Body thinks it s starving despite hyperglycaemia Unregulated ketosis results with subsequent acidosis Results in polyuria, dehdyration and circulatory shock Signs / Symptoms Confusion Abdominal pain Vomiting Confusion / drowsiness Kussmaul breathing Causes Infection Surgery Alcohol Missed insulin Trauma
DKA Investigations: Ketones >3 pH <7.3 BM >15 Find the cause: Monitoring Catheter Hourly Ketones + BM Ketones should drop by 0.5/h Hourly VBG K+ and bicarbonate Keep potassium >4 Resolution Ketones <3 pH > 7.3 Stop FRII when back E+D and has had normal insulin 1h ago Accurate urine output needed At least 0.5ml/kg/hr FBC, blood Cultures, CXR, Urine culture/dip, Find the damage U/Es, A/VBG, ECG Treatment: 1. Fluids a. Deficit + Maintenance/24hr b. Rapid initial administration then taper c. Potassium (If K+ <5.5) 2. Intravenous Insulin (0.1u/kg) a. Continue normal s/c insulin! 3. 10% Dextrose a. When BM <15
Mentimeter Code: 3768 4640
Practice Question A 55 year old patient presents with low blood pressure, increased pigmentation of skin creases, low glucose, low sodium and high potassium What is the best investigation to order to confirm the likely diagnosis?
Practice Question A patient presents with new-onset type 2 diabetes, an enlarged jaw and forehead and carpal-tunnel syndrome. Which investigation would be most useful to diagnose the likely cause? Short SynACTHen test Combined pituitary function test Measurement of plasma [growth hormone] Low-dose dexamethasone suppression test Oral glucose tolerance test a) b) c) d) e)
Both mother and grandmother had medullary thyroid carcinoma, and have tested positive for MEN2. What [biomarker/protein] would be raised in the blood to confirm medullary thyroid cancer?
Along with an appropriate fluid regime what other management should be started? A 24-year-old female is brought into the emergency department with a 3-day history of abdominal pain, vomiting, polyuria and reduced eating and drinking. She has T1DM and usually takes both long and short acting insulin. pH 7.32 Ketones 5 BM 20
Thank you very much! Feedback link: https://forms.office.com/r/VYYRE1Wxmt