primary thyroid lymphoma
Primary thyroid lymphoma is a rare form of cancer that primarily affects the thyroid gland. This type of lymphoma is typically of B-cell lineage and is often associated with preexisting chronic autoimmune thyroiditis, such as Hashimoto's thyroiditis. The etiology of primary thyroid lymphoma is not entirely understood, but risk factors include iodine supplementation and a history of autoimmune thyroiditis. Diagnosis involves a combination of history, physical examination, thyroid ultrasound, and biopsy, with treatment often including chemotherapy. This article provides an overview of the diagnostic approach, etiology, classification, and treatment of primary thyroid lymphoma.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
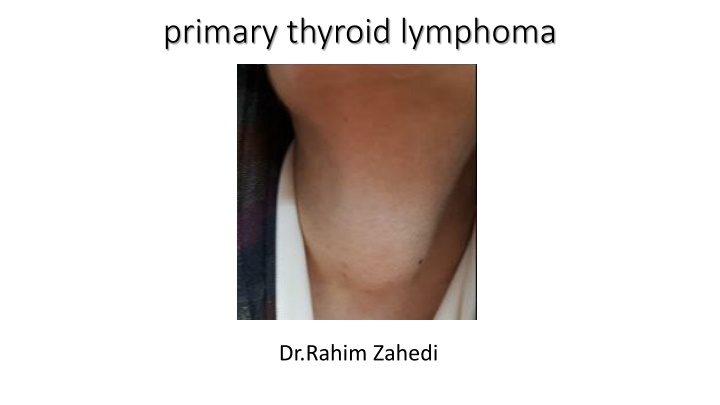
primary thyroid lymphoma Dr.Rahim Zahedi
Rapid enlargement of thyroid Rapid enlargement of thyroid Acute infectious thyroiditis ( onset of pain, firmness, tenderness, redness or swelling in the anterior aspect of the neck, sudden fever, dysphagia and dysphonia, very rare 0.1 0.7% of all thyroiditis ) subacute thyroiditis (pain, swollen and tender, fever, fatigue, weakness, difficulty swallowing) hemorrhage of thyroid adenoma or cyst Anaplastic thyroid cancer (neck pain and tenderness, and compression or invasion of the upper aerodigestive tract, resulting in dyspnea about 35 percent , dysphagia 30 percent, hoarseness 25 percent, cough and sometimes hemoptysis, 25 percent) Thyroid lymphoma
Diagnostic approach History and physical examination : rapid growth of a neck mass , no history of irradiation, no family history of thyroid cancer, no history of hypothyroidism, dyspnea and dysphagia, there is a palpable firm mass in approximate size of 5*4cm in right lobe of thyroid and could be palpated over isthmus of thyroid which causes left trachea deviation Serum TSH : 1.1 mlu/ml Thyroid ultrasonography : a hypoechoic 59*38 m.m mass in Rt lobe of thyroid with internal vascularity , without calcification , without hypoechoic rim FNA : Benign , Note : due to monomorphic pattern of lymphoid cells, lymphoma cannot be ruled out COR NEEDLE BIOPSY :primary thyroid lymphoma TREATMENT : chemotherapy (R-CHOP)
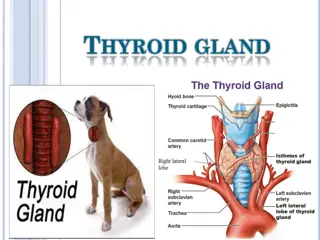
Primary thyroid lymphoma Thyroid lymphomas are nearly always of the non-Hodgkin type Only about 2 percent of extranodal lymphomas arise within the thyroid gland lymphomas represent no more than 2 percent of all malignant thyroid tumors the annual incidence rate was estimated to be 2.1 per million persons with a four to one female predominance The mean and median ages at diagnosis are between 65 and 75 years
ETIOLOGY Preexisting chronic autoimmune (Hashimoto's) thyroiditis is the only known risk factor for primary thyroid lymphoma and is present in about one-half of patients Among patients with Hashimoto's thyroiditis, the risk of thyroid lymphoma is at least 60 times higher than in patients without thyroiditis Lymphoma may also occur more commonly after iodine supplementation There appears to be no clear association between exposure to ionizing radiation and lymphoma Chromosomal abnormalities are rare in thyroid lymphomas
CLASSIFICATION Primary thyroid lymphoma is almost always of B-cell lineage often in areas endemic for HTLV-I-associated adult T-cell leukemia/lymphoma 60 to 80 percent of thyroid lymphomas are diffuse large B-cell lymphomas The next most common subtype (approximately 30 percent) is extranodal marginal zone lymphoma Other less common histologic subtypes include follicular lymphomas extranodal small lymphocytic lymphomas have also been described
CLINICAL PRESENTATION In more than 90 percent , the major symptom is a rapidly enlarging goiter Many patients have symptoms or signs of tracheal, esophageal or neck vein compression, including dysphagia, dyspnea, stridor, hoarseness, neck pain, and facial edema On examination, the thyroid is firm, even hard, may be slightly tender, and is often fixed to adjacent structures and immobile with swallowing Substernal extension is common About one-half of patients have enlarged cervical or supraclavicular lymph nodes up to 10 percent of patients have systemic ("B") symptoms of lymphoma
DIAGNOSTIC EVALUATION An ultrasound scan of the thyroid gland and needle biopsy or excisional biopsy are usually recommended as initial diagnostic procedures Although the diagnosis of lymphoma may be suggested by the fine needle aspiration initially performed for suspicion of thyroid malignancy, fine needle aspiration cytology is often nondiagnostic for thyroid lymphoma Thyroid lymphomas cannot be distinguished from carcinomas or Hashimoto's thyroiditis by radiographic or radionuclide imaging Radioiodine scanning has no diagnostic role in patients with thyroid lymphomas because the malignant cells lack iodine-concentrating ability CT and MRI are superior to ultrasonography for evaluating local extent because of their greater ability to detect tracheal invasion, substernal extension, and involvement of cervical, mediastinal, or abdominal nodes MRI may be more sensitive for defining the extent of extrathyroidal invasion
TREATMENT Severe airway compromise may occur in up to 25 percent of an aggressive lymphoma variant (eg, DLBCL) Such tumors shrink within hours after initiation of combination chemotherapy (eg, CHOP), due to the rapid effect of the steroid component, potentially obviating the need for tracheotomy There is little evidence that thyroidectomy is of value in patients with stage IIE or IIIE thyroid lymphoma In patients with clinical stage IE disease (particularly MALT lymphomas), surgery may permit the distinction between intrathyroid tumor, which may be treatable by local therapy alone (surgery followed by postoperative radiation), and extrathyroid extension, which appears to require systemic chemotherapy Patients with diffuse large B-cell lymphoma (DLBCL) of the thyroid should be treated in the same manner as employed in patients with DLBCL of any other site or extent. Thus, patients with localized, early stage disease can be treated with either three courses of combination therapy (eg, CHOP plus rituximab , followed by radiation therapy to the thyroid bed or six to eight cycles of CHOP plus rituximab without radiation
PROGNOSIS In one series of 51 patients with localized (stage I or II) thyroid lymphoma, five-year failure-free survival rates were 76, 50, and 91 percent for patients treated with radiation, chemotherapy, or combined modality therapy, respectively In another series of 171 patients with localized (stage IE or IIE) thyroid lymphoma, five-year event-free survival rates for aggressive (diffuse large B-cell lymphoma and diffuse large B-cell lymphoma with MALT) and indolent (MALT) lymphoma was 73 and 89 percent, respectively
Survivals The 5- and 10-yr probability of overall survival (OS) was, for all patients, 77% and 54%, respectively The median survival was 10.9 yr OS was significantly influenced by age and performance status , and a complete response was achieved with the treatment
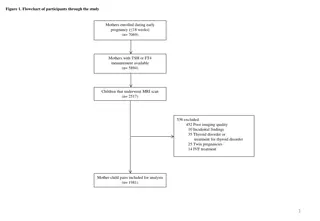
We included 13 consecutive patients with pathologically proven primary thyroid lymphoma at Xiangya Hospital from 2007 to 2013 Another 27 patients were randomly chosen as controls who had pathologically proven nodular goiter at our hospital from 2012 to 2013
Thank you Thank you for your attention for your attention