BLOOD PHYSIOLOGY
A vital liquid connective tissue in the human body, responsible for various functions such as transportation, homeostasis, protection against infections, and blood clotting. It comprises plasma and formed elements, with plasma containing essential proteins like Albumin, globulin, and Fibrinogen. Learn about the volume of blood in adults, the role of plasma proteins in coagulation and immune defense, maintenance of osmotic pressure, and transportation of nutrients.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
BLOOD PHYSIOLOGY By roll no. 51,52,53,54,55
Introduction Blood is type of liquid connective tissue The total blood volume takes up about 6% to 8% of body weight. So an average adult human will have 5-6L of blood. The circulating blood volume will be less than the total blood volume as some blood is deposited in organs like liver and spleen.
Blood Volume Blood Volume 5 liter in adult: 45% is packed cells volume (PCV). 55% is plasma volume. 3
FUNCTIONS OF BLOOD FUNCTIONS OF BLOOD 1. Transport O2, CO2, nutrient, hormones, waste product 2. Homoeostasis Regulation of body temperature, ECF pH 3. Protecting against infections White Blood Cells, Antibodies 4. Blood clotting prevent blood loss 4
Composition Plasma Formed elements 55- 60% by volume 40-45% by volume
Plasma composition 98% water + ions + plasma proteins e.g. (Albumin, globulin, Fibrinogen) Same ionic composition as interstitial fluid. 8
Plasma proteins and their roles Blood Plasma has various vital functions Coagulation- Plasma contains fibrinogen and procoagulants such as thrombin and factor x Immune Defense- Plasma has Immunoglobulins (antibodies) that play a role in the body s immunological defence process
Maintenance of osmotic pressure- The presence of plasma proteins such as Albumin which is vital for maintaining a balance of fluid, called oncotic pressure, in the blood (maintained at around 25 mmHg). Acid-base balance- Plasma proteins helps in acid-base balance through buffering action. Transportation of Nutrients- Nutrients such as glucose, amino acids, liquids and vitamins are transported in the blood plasma from the digestive system to different body parts.
Transportation of Respiratory Gases. Oxygen is carried to the body from the lungs and carbon dioxide back to the lungs for excretion. Transportation of Hormones. Excretion- Waste products from cellular metabolism are carried within the plasma and excreted via the kidneys, lungs and skin Temperature Regulation The erythrocyte sedimentation rate (ESR) is used as a diagnostic tool. As fibrinogen increases in acute inflammatory conditions, the ESR will also increase.
Plasma pH The pH of blood plasma is approximately 7.4, which is slightly acidic. The condition of high plasma pH is called alkalosis; low plasma pH is acidosis. The body has three lines of defense against departures from normal plasma pH: the chemical buffers, the respiratory system, and the renal system.
Serum Serum is the fluid and solute component of blood which does not play a role in clotting. It may be defined as blood plasma without the clotting factors, or as blood with all cells and clotting factors removed.
Blood corpuscles/ Formed elements 1.Erythrocytes 2.Leucocytes 3.Thrombocytes
Blood Cells Formation Erythropoiesis: Formation of RBC (erythrocytes) Leucopoiesis: Formation of WBC (leucocytes) Thrombopoiesis: Formation of platelets (thrombocytes) 16
Red Blood Cells Red Blood Cells Shape & size Flat Biconcave Disc. Non-nucleated. Diameter 7-8 mx2.5 mx1 m. Flexible Average volume 90-95 m3 Number = 4.7 - 5 x106 Hb = 14-16 g/dl in the blood 17
Production of RBC In-utero: Early few weeks of embryo nucleated RBCs are formed in yolk sac. Middle trimester mainly in liver & spleen & lymph nodes. Last months RBCs are formed in bone marrow of all bones. 18
After Birth: Bone marrow of flat bone continue to produce RBC into adult life Shaft of long bone stop to produce RBC at puberty while epiphysis continued
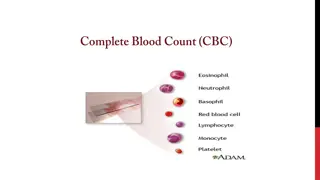
Leucocytes Leucocytes are the cellular component of the blood that are also known as white blood cells (WBCs). WBCs have a nucleus and lack hemoglobin. WBCs form 1% of the total blood volume in healthy adults.[5] They are considered to be an important part of the immune system. The leucocytes are produced in the bone marrow in a process called Hematopoiesis[11] and normal WBCs count ranged between 4,000 and 10,000 cells/MCL
Types and Function of Leucocyte There are several types of WBCs such as Neutrophils, Eosinophils, Basophils, Lymphocytes (B and T) and Monocytes
Neutrophils Neutrophils are WBCs that are released from the bone marrow. They represent 50% of total WBCs count. Around 100 billion of the Neutrophils cells are produced every day and they are considered to be the first immune system cells. They are the major pathogen- fighting immune cells that migrate to sites of infection and then identify and kill bacteria and viruses. Neutrophils also send signals to alert other immune system cells.
Monocytes Monocytes represent 5 to 12 % of the total WBCs count. They are considered to be the garbage trucks of the immune system and play an important function in cleaning dead cells and tissue regeneration.
Eosinophils Eosinophils represent less than 5% of the total WBCs. They are found in large amounts in the digestive system. Eosinophils play an important role in dealing with invading bacteria and parasites, such as worms.
Basophils Basophils represent 1% of the total WBCs count. These cells play a role in asthma. They stimulate histamine release, leading to the inflammation and bronchoconstriction that occurs in asthma.
Lymphocytes Lymphocytes produce antibodies that give immunity to the body if the body is exposed to the same infection again. It consists of two types of cells, T cells which have an invading function and B cells, which in contrast to other WBCs, are responsible for humoral immunity ie immunity associated with circulating antibodies, in contradistinction to cellular immunity. These cells play an important role in developing a lot of the current vaccines.
Platelets Platelets are small anucleate cell fragments that circulate in blood playing crucial role in managing vascular integrity and regulating hemostasis. Platelets are also involved in the fundamental biological process of chronic inflammation associated with disease pathology.
Abnormalities Abnormalities Blood Disorders There are many conditions of/or affecting the human hematologic system i.e the biological system that includes plasma, platelets, leukocytes, and erythrocytes, the major components of blood and the bone marrow. This list is an example of disorders:
Hemochromatosis Sickle Cell Anemia Anaemia of Chronic Disease Acute Lymphoblastic Leukemia Acute Myeloid Leukemia Multiple Myeloma Aplastic Anaemia Erythrocytosis Paraneoplastic Syndrome Hypercoagulable Disorder Iron Deficiency and vitamin B12 Anemia Leucocytosis Leucopenia
What causes increased blood in the body? Your body may increase red blood cell production to compensate for any condition that results in low oxygen levels, including: Heart disease (such as congenital heart disease in adults) Heart failure. A condition present at birth that reduces the oxygen-carrying capacity of red blood cells (hemoglobinopathy Polycythemia vera (pol-e-sy-THEE-me-uh VEER-uh) is a type of blood cancer. It causes your bone marrow to make too many red blood cells. These excess cells thicken your blood, slowing its flow, which may cause serious problems, such as blood clots. Polycythemia vera is rare.
What happens The increase in blood cells makes the blood thicker. Thick blood can lead to strokes or tissue and organ damage. Symptoms include lack of energy (fatigue) or weakness, headaches, dizziness, shortness of breath, visual disturbances, nose bleeds, bleeding gums, heavy menstrual periods, and bruising.
Bleeding disorders When some coagulates found in the plasma are malfunctioned it will lead to bleeding disorders such as haemophilia and von Willebrand disease
Anemia A condition in which there is a deficiency of red cells or of haemoglobin in the blood, resulting in pallor and weariness. Anemia has three main causes: blood loss, lack of red blood cell production, and high rates of red blood cell destruction.
Anemia Anemia can also be classified based on the size of the red blood cells and amount of hemoglobin in each cell. If the cells are small, it is called microcytic anemia; if they are large, it is called macrocytic anemia; and if they are normal sized, it is called normocytic anemia.
Clinical examination Complete blood count with indices: MCV indication of RBC size. RDW indication of RBC size variation. Examination of the peripheral blood smear. Reticulocyte count: Measurement of newly produced young RBC s. Considered a measure of bone marrow responsiveness.
Microcytic Anemia Microcytic anemia is defined as the presence of small, often hypochromic, red blood cells in a peripheral blood smear and is usually characterized by a low MCV (less than 83 micron ). Iron deficiency is the most common cause of microcytic anemia.
Iron deficiency A condition of too little iron in the body. Iron deficiency is a common cause of too few healthy red blood cells in the body (anaemia). In a pregnant woman, iron deficiency puts the baby at risk of developmental delays. Thalassemia Thalassemia is an inherited blood disorder characterised by less oxygen-carrying protein (haemoglobin) and fewer red blood cells in the body than normal.
Sideroblastic anemia Sideroblastic anemia is a group of blood disorders characterized by an impaired ability of the bone marrow to produce normal red blood cells . In this condition, the iron inside red blood cells is inadequately used to make hemoglobin, despite normal amounts of iron. Anemia of chronic disease Anemia of inflammation, also called anemia of chronic disease or ACD, is a type of anemia that affects people who have conditions that cause inflammation, such as infections, autoimmune diseases, cancer link, and chronic kidney disease (CKD).
Normocytic Anemia Normocytic anemia is a blood problem. It means you have normal-sized red blood cells, but you have a low number of them. The presence of normal-sized red blood cells tells your doctor that you have normocytic anemia rather than another kind of anemia.
Anemia of chronic diseases Iron deficiency (Early) Anemia of renal disease Anemia of renal disease is a hypoproliferative anemia , a decrease in the number of red blood cells (RBCs), hemoglobin (Hb) content, can result from decreased RBC production (erythropoiesis), increased RBC destruction. Combined nutritional deficiency Nutritional deficiency anemia traditionally includes iron deficiency anemia (IDA), vitamin B12 (cobalamin) deficiency anemia, folate deficiency anemia, protein deficiency anemia, and pyridoxine deficiency anemia
Marrow failure Bone marrow failure is the reduction or cessation of blood cell production affecting one or more cell lines. Pancytopenia, or decreased numbers of circulating red blood cells (RBCs), white blood cells (WBCs), and platelets, is seen in most cases of bone marrow failure, particularly in severe or advanced stages. Hypothyroidism Abnormally low activity of the thyroid gland, resulting in retardation of growth and mental development in children and adults.
Macrocytic Anemia Macrocytic anemia is defined as the insufficient concentration of hemoglobin in which the red blood cells (RBCs) (erythrocytes) are larger than their normal volume.
Megaloblastic anemia Megaloblastic anemia is a type of anemia characterized by very large red blood cells. In addition to the cells being large, the inner contents of each cell are not completely developed. This malformation causes the bone marrow to produce fewer cells, and sometimes the cells die earlier than the 120-day life expectancy. Hemolytic anemia Hemolytic anemia is a disorder in which red blood cells are destroyed faster than they can be made. Liver disease Macrocytic anemia in liver disease may be due to an increased deposition of cholesterol on the membranes of circulating RBCs
Hypothyroidism Myelodysplasia A myelodysplastic syndrome (MDS) is one of a group of cancers in which immature blood cells in the bone marrow do not mature, so do not become healthy blood cells