Awake Intubation Overview and Techniques
Awake intubation, as demonstrated by Dr. Jed Wolpaw MD, M.Ed, is a crucial technique for managing patients with difficult airways or who are at risk of aspiration. This method allows for intubation while the patient is conscious, offering a safe approach in challenging scenarios. The content covers indications, history, techniques (focusing on nasal approach), and considerations for patient preparation, nerve blocks, sedation, and more, providing valuable insights into the practice of awake intubation.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Awake Intubation Jed Wolpaw MD, M.Ed
References Based primarily on Collins SR and Blank RS. Fiberoptic Intubation: An Overview and Update. Respiratory Care. June 2014: 59;6(865-880).
Outline Indications Approaches Patient preparation Nasal Oral Nerve blocks Sedation Other approaches
History Peter Murphy, in England, in 1965 used a fiberoptic choledocosope to intubate nasally a pt with Still s disease.
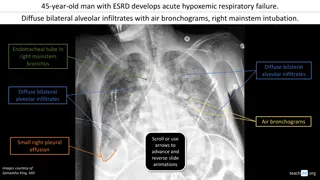
Indications for Awake Intubation Need for intubation where ability to ventilate via mask or supraglottic airway is unlikely or poses an aspiration risk History of need for awake intubation Anatomic features that are worrisome Limited mouth opening, reduced neck mobility, cervical spine instability, anatomic malformations of mandible or larynx, congenital deformities (Pierre Robin), head and neck cancers, trauma to the face, airway.
How common are difficult airways Review of 50,000 records excluded planned fiberoptics Found impossible to mask was only 0.15%, and 25% of those were difficult to intubate
Neck movement When compared with DL or glidescope FOI causes less movement of cervical spine
Techniques: Nasal Preferred when: large tongue, limited mouth opening receding lower jaw, or tracheal deviation or in cases in which an unobstructed surgical field is beneficial (eg, dental surgery). This approach is also anatomically favorable in that the laryngeal opening is more easily seen with the fiberscope as it courses past the nasopharynx with less obstruction by the tongue
Nasal Anti-sialogogue: Glycopyrollate 0.1-0.2mg Afrin or phenylephrine and lidocaine to nare, ask which is more open Inhaled nebulized lidocaine at 5l/min flow for correct droplet size, not trying to get into lungs, have pt stick out tongue Spray additional high concentration lidocaine through atomizer into back of throat and directed down on cords 5% lidocaine ointment onto tongue depressors with 4x4 attached, paint back of throat and let drip down while pt bites on tongue blade Plus/minus trans-tracheal injection of lidocaine, more concentrated is better Can also spray as you go
Nasal continued Dilate nare with increasing size of lubed NP airways Insert tube with gentle pressure until passes into oropharynx, then inflate balloon and draw back until resistance is felt Insert fiber and pass into cords, deflate cuff and advance tube Ideally use smaller tube, 6-5 or 7-0 better than 7-5 or 8-0 due to ease of passage into trachea If you cannot visualize cords, try having someone do a jaw thrust and/or pull the tongue out of the mouth with a 4x4 If scope is in trachea but tube won t pass, withdraw slightly and rotate 90 degrees and try again, then another 90 degrees. If necessary try corkscrew Parker Flex tip tube has curved tapered distal tip to slide past cords more easily
Oral Harder due to tongue, more anterior path needed to get to cords No nasal prep needed, otherwise the same Can use special oral airway such as Ovassapian with central channel to pass scope Jaw thrusts and tongue out can really help here Key is staying midline, walk along the tongue, manipulate ETT
Nerve Blocks Glossopharyngeal nerve supplies sensory to posterior third of tongue, vallecular, anterior epiglottis, walls of pharynx, tonsils Block by holding pledgets with lidocaine at tonsillar pillars or injecting at mandible and mastoid processes. Superior laryngeal nerve provides sensory to base of tongue and posterior surface of epiglottis to arytenoids. Block by injecting local at cornua of hyoid bone Vagus nerve branches (recurrent laryngeal) supply sensory innervation to the underside of epiglottis and trachea Transtracheal block 1% lido can last 75 minutes, up to 400 minutes with 1:200,000 epi
Sedation Depends on how scary the airway is, okay to use no sedation Versed +/- fentanyl Remi bolus vs drip (0.5-1mcg/kg and 0.05-0.1 mcg/kg/min) Ketamine bolus vs drip (0.3-0.5mg/kg and 10mcg/kg/min) Precedex, load and drip (0.4-1mcg/kg bolus over 10 min + 0.5-1mcg/kg/HR) General anesthesia with spontaneous ventilation, inhaled or propofol More hypoxia with propofol Remi vs. Prop: Remi better conditions, better tolerated, patients breathed when told to Precedex vs prop: Precedex superior in terms of hemodynamic stability and not having airway obstruction Precedex vs remi: Precedex better in terms of desaturations Johnston KD and Rai MR Consious Sedation for awake fiberoptic intubation: a review of the literature. Can J Anesth (2013) 60:584-599.
Other techniques Fiber through LMA Awake glidescope Awake DL DL and fiber or glidescope and fiber