Understanding Dental Composites: History, Classification, and Properties
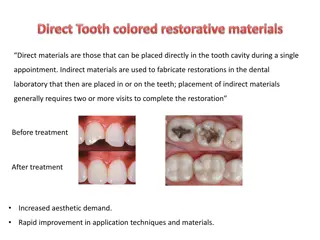
Dental composites are tooth-colored materials developed for natural appearance in dental procedures. They are defined as highly cross-linked polymeric materials reinforced with fillers. This article covers the history, classification, and properties of dental composites, including definitions by experts in the field like Anusavice. Various classifications and types of composites are discussed, providing insight into their composition and advantages in aesthetic and cosmetic dentistry.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
The constant desire of dental profession to achieve a natural appearance has led to development of various tooth coloured material, one among them being DENTAL COMPOSITE
CONTENTS History Definition Classification Indication and contraindication Advantages and disadvantages Composition Properties of composite
DEFINITION By Anusavice 1. Composite in material science, a solid formed from two or more distinct phases (e.g. particles in a metal phase) that have been combined to produce properties superior to or intermediate to those of the individual constituents Dental composite is defined as a highly cross-linked polymeric material reinforced by a dispersion of amorphous silica, glass, crystalline, or organic resin filler particles and/or short fibers bonded to the matrix by a coupling agent
DCNA 2007; Dental materials; vol. 51; July Composite is a multiphase material that exhibits the properties of both phases where the phases are complimentary, resulting in a material with enhanced properties. DCNA 2007; vol. 50, Aesthetic and cosmetic dentistry A composite is a multiphase substance formed from a combination of materials that differ in composition or form, remain bonded together, and retain their identities and properties. Sturdevant A composite is a physical mixture of the materials.The parts of the mixture generally is chosen with the purpose of averaging the properties of the parts to achieve intermediate properties.
CLASSIFICATION 1. ADA specification No. 27 (JADA Vol. 94, Jun 1977) Type 1:unfilled and filled resins Type 2: composite resin materials to which a filler has been added 2. Skinner s classification (10th edition) Traditional composites (Macrofilled) 8-12 m Small particle filled composite 1-5 m Microfilled composite 0.04 0.4 m Hybrid composite 0.6 1 m
Lutz and Philips (1983) The basis for the Lutz and Philips (1983) System rests with three types of fillers organized into four major classes. The three types of filler particles are Traditional macro-fillers Microfillers (Pyrogenic silica) Microfiller based complexes, with three subgroups. Splintered pre-polymerized microfilled complexes (SSP) Spherical polymer-based microfilled complexes (SphPB) The agglomerated microfiller complexes (AMC According to Craig TYPE I : polymer based materials suitable for restoration ivolving occlusal surfaces TYPE II :other polymer based materials Class 1:self cured materials class 2:light cured materials group 1 :energy applied intra orally group 2 :energy applied extra orally
According to sturdevant (4th edition) Based on range of filler particle size Megafill- quartz , large size Macrofill 10-100 m Midifill 1-10 m Minifill 0.1-1 m Microfill 0.01-0.1 m Nanofill 0.005-0.01 m
Composites with mixed range of particles sizes are called hybrid and the largest particle size range is used to define the hybrid type Midifill hybrid Minifill hybrid According to whether composite is a homogenous mixture of resin and filler or includes the pre-cured composite Homogeneous if composite consists of filler and uncured matrix material Heterogeneous if it includes pre-cured composites or other unusual filler
Based on area of application Anterior Posterior composites Based on method of curing Chemical curing Light curing UV light Visible light Plasma arc Laser curing Dual cure Based on consistency Light body Flowable composite Medium body Homogeneous microfills, macrofills and midifills minifills Heavy body Packable hybrid DCNA (Leinfelder K; Apr; 1985) Classified composites as conventional composites Intermediate composite Hybrid composite
According to Marzouk:- 1st -Macro ceramics 2nd -Colloidal silica 3rd -Hybrid :macro and micro colloidal ceramics 4th Hybrid : heat cured irregularly shaped 5th -Hybrid : heat cured spherical 6th -Hybrid : agglomerates of sintered micro ceramics
INDICATIONS CONTRAINDICATIONS When proper isolation is not possible Class I, II, III, IV, V, VI restorations Foundations or core buildups When occlusion is on composite restoration Sealants and preventive resin restorations When preparation extending on root surface or subgingival area Poor oral hygiene Esthetic enhancement procedures Cements (for indirect restorations) High caries index Temporary restorations Patient s with abnormal habits (bruxism) For splinting Subgingival area/root surface Non caries lesions like abrasion erosion Enamel hypoplasia Composite inlays and onlays Repair of old composite restoration
ADVANTAGES DISADVANTAGES Esthetics Technique sensitive Conservation of tooth structure Polymerization shrinkage Less complex when preparing the tooth Higher coefficient of thermal expansion Insulative having low thermal conductivity Difficult time consuming Used almost universally Increased occlusal wear Bonded to tooth structure (good retention) Low modulus of elasticity Repairable Bio-compatibility ? No corrosion Staining Strengthening of tooth structure Costly
Composition Resin matrix Optical modifiers Coupling agent Inhibitor Fillers Activator and initiator
RESIN MATRIX PRINCIPAL MONOMERS BIS-GMA-aromatic-1962-BOWEN S RESIN Bis-GMA structure The bis-phenol A nucleus: Terminal methacrylate groups Hydroxyl groups
ADVANTAGES DISADVANTAGES High molecular weight Difficult to crystallize and purify Extensive cross-linking- increases rigidity High molecular weight increase viscosity Decreased polymerization shrinkage Stability of color is questionable Non-volatile It produces less heat during polymerization.
DILUENT MONOMERS Urethane dimethacrylate-(UDMA) Triethylene glycol dimethacylate-(TEGDMA) Ratio of Bis-GMA to TEGDMA 3:1 75wt% bis-GMA,25%wt%TEGDMA-4300centipose Ratio of Bis-GMA to TEGDMA-1:1 50wt% TEGDMA,50wt% Bis-GMA-200centipose
Functions of the diluent Reduce the viscosity Results in higher filler loading. Results in higher degree of conversion. Increase the number of cross-linking reactions. Increases the gelation time Disadvantage of the diluent Greater polymerization shrinkage. Increased flexibility. Decreased abrasion resistance. Tends to encourage microbial activity potential for secondary caries
fillers fillers Functions of the fillers - Reinforcement of matrix resin resulting in increased hardness, strength and decreased wear. Reduction in polymerization shrinkage Reduction in thermal contraction and expansion Improved workability by increasing the viscosity Reduction in water sorption, softening and staining Increased radiopacity and diagnostic sensitivity through the incorporation of strontium (Sr) and barium (Ba) glass and other heavy metal compounds that absorb X-rays.
Materials used for fillers:- Types of fillers used -ground quartz colloidal silica glasses or ceramic containing heavy metal Other fillers used are Amorphous silica Organic filler Fiber filler Single crystal Crystalline polymers Fluoride containing fillers
Filler loading Between 30 and 70 volume% or 50 to 85 wt% of a composite. The maximum theoretical packing fraction for closed-packed structure is 74 vol%. Filler surface area 50-400 m2/gm Recent areas of study in fillers Calcium metaphosphate ceramics Hollow sphere plastic Glass fiber Beta-quartz glass inserts Fluoride-containing inorganic materials as fillers
COUPLING AGENTS Essential for bonding of fillers to the resin matrix. Functions of the coupling agents Bind filler particles to resin. Allow more flexible polymer matrix to transfer stresses to the higher modulus (more stiffer & stronger) filler particles Impart improved physical & mechanical properties Inhibit leaching by preventing water from penetrating along the resin-filler interface. Types of coupling agents Organosilanes -methacryloxypropyl trimethoxysilane (MPS). Titanates. Zirconates A174 (3-methacryloxy-propyl-trimethoxysilane)
ACTIVATOR-INITIATOR SYSTEM Chemically activated Benzoyl peroxide initiator (universal paste) Aromatic tertiary amine activator (N,N, dimethyl-p- toluidine)(catalyst paste) Light activated Camphorquinone -0.2%-1% Organic aliphatic amine dimetylaminoethyl methacrylate (DMAEMA)-0.15%, ethyl-4-dimethylaminobenzoate (EDMAB), or N,N-cyanoethyl- methylaniline (CEMA) Absorbs blue light with wavelength between 400 and 500 nm Dual activated composites
Inhibitor Butylated hydroxytoluine (BHT), which is used in concentration of 0.01 wt%. inhibitors have two functions They extend the storage life time for all resins They ensure sufficient working time. Optical modifiers To match the appearance of teeth commonly titanium dioxide and aluminum oxides are added as opacifiers in minute amounts 0.001 to 0.007 wt%. Uv stabilizers prevents discolouration 2-hydroxy-4 methoxy benzophenone
TYPES OF COMPOSITE Conventional /traditional composite Small particle filled composite Microfilled composite Hybrid composite
Traditional composite Developed during the 1970s filler used - finely ground amorphous silica and quartz. The average particle size is 8 - 12 m, Filler loading generally is 70 80 wt% or 60 70 vol% Indication used in class II and class IV
Clinical considerations Produce rough surface Difficult to polish High initial wear Can be used for stress bearing areas Clinical considerations Produce rough surface Difficult to polish High initial wear Can be used for stress bearing areas strength Advantages Disadvantages Compressive, tensile Polishability Surface roughness Stiffness Staining, plaque Hardness Occlusal wear Polymerization shrinkage Poor esthetics Water sorption, thermal expansion
Properties of traditional composites Compressive strength-300% to 500% Elastic modulus -4 to 6 times higher Water sorption,polmerization shrinkage,thermal expansion Resistant to abrasion High hardness
Small particle filled composite Introduced to overcome the disadvantages of traditional composite Inorganic fillers are ground to a size range of approximately 0.5 to 3 m, but with a fairly broad size range distribution Contain more inorganic filler (80 wt% to 90 wt% and 65 to 77 vol%) than traditional composites Use amorphous silica as filler, but most incorporate glasses that contain heavy metals for radiopacity Colloidal silica added in amounts of approximately 5 wt% to adjust the viscosity of paste.
Clinical application Indicated for application in which large stresses and abrasion might be encountered Attain a reasonably smooth surface for anterior application but not as good as hybrid or microfilled composites. Advantages Disadvantages Good mechanical properties Prone to wear and deterioration. Good smoothness Less polymerization Shrinkage Radiopacity Wear resistance
Properties of SPF Superior physical,mechanical properties Compressive strength,elastic modulus,wear resistance,surface smoothness Tensile strength Polymerization shrinkage,co-efficient of thermal expansion
Microfilled composite Introduced in 1970s Individual particles are approximately 0.04 m (40nm) in size - Colloidal silica particles Ground polymer with colloidal silica (50 u) Filler size - 0.004 to 0.4 m size range. Polymer matrix with colloidal silica Inorganic filler content - 35 to 60% by wt. The greater surface area per unit volume of these microfine particles, the microfill composites cannot be heavily filled Approaches to increase the filler loading Sintering Grinding of prepolymerized composites Final inorganic filler - 50 wt%; if composite particles counted as filler particles, the filler content is closer to 80 wt% (approx 60 vol %)
Clinical consideration In stress-bearing situation, the potential for fracture is greater Diamond burs rather than fluted tungsten-carbide burs are recommended for trimming Low modulus of elasticity suitable for restoring class V cervical lesions or defects where cervical flexure can be significant Indications Esthetic anterior restoration Restoring sub-gingival areas Carious lesion on smooth surface (Class V)
properties Inferior physical and mechanical properties Higher co-efficient of thermal expansion decreased elastic modulus Remain remarkably wear resistant
Advantages Disadvantages Best surface finish Tensile strength Excellent wear resistance Water sorption and CTE fracture resistance Radiolucent Polymerization shrinkage
Hybrid composites Developed to combine properties of conventional and microfilled composites Contain two kinds of filler particles - colloidal silica and ground particles of glasses containing heavy metals Content of approximately 75 to 80 wt%. Average particle size of about 0.4 to 1.0 m Colloidal silica represents 10 20 wt% of total filler content. Silane-coated silica or glass Polymer matrix with colloidal silica
Clinical considerations Surface smoothness and reasonably good strength used in anteriors including Class IV Few practical differences between hybrid and SPF composites - two terms used interchangeably Provides a smooth Platina-like surface texture in finished restoration. Currently are the predominant direct esthetic restorative material used. Have almost universal clinical applicability Advantages Disadvantages Good physical properties Improve wear resistance Increased surface roughness with time Superior surface morphology Good esthetics
Chemically cured composite Syringes Tubes Light-cured composite Syringes Compules Enlarge picture
CHEMICALLY ACTIVATED RESINS Supplied as two pastes When the two pastes are spatulated, the amine reacts with the Benzoylperoxide to form free radicals and polymerization is initiated. Advantages Even polymerization throughout the restoration to maximum 75% Disadvantages Impossible to avoid incorporation of air into the mix forms pores and weakens the structure. Oxygen inhibition of polymerization during curing No control over the working time Both insertion and contouring must be completed quickly once the resin components are mixed and placed into the cavity Often discolors after 3-5 yrs of intraoral service
Light-cured composites Developed To overcome the problems of chemical activation The first light activated systems were formulated for UV light to initiate free radicals. Today, the UV light is replaced by visible blue light-activated systems Light curable composites are supplied as a single paste contained in a light-proof syringe The free radical initiating system, consists of a photosensitizer and an amine initiator, is contained in this paste Camphorquinone (CQ) is photosensitizer - absorbs blue light with wavelengths between 400 and 500nm Amine initiator is Dimethylaminoethylmathacrylate (DMAEMA) in case of visible light and Benzoylmethylether in case of UV light polymerization
Advantages Easy to use, single paste system Less porosity Color stability Command polymerization Allow operator to complete insertion and contouring before curing is initiated They are not as sensitive to oxygen inhibition as the chemical cured systems Better mechanical properties Setting time faster cure; an exposure of 40 seconds or less is required to light cure a 2mm thick layer.
Disadvantages They must be applied incrementally when the bulk exceeds approx. 2 3mm Limited depth of light penetration Time consuming Relatively poor accessibility in certain posterior and interproximal locations Variable exposure times because of shade differences, resulting in longer exposure times for darker shades and/or increased opacity Sensitivity to ambient light leads to formation of a skin or crust when an opened tube is exposed Cost of the light curing unit is expensive Shrinkage towards light source Ocular damage can cause retinal damage if one looks directly at the beam.
Chemical Light cure Polymerization is central Peripheral Curing is one phase Is in increments Sets within 45 seconds Sets only after light activation No control over working time Working time under control Shrinkage towards centre of bulk Shrinkage towards light source Air may get incorporated Less chance of air entrapment More wastage of material Less wastage Not properly finished Better finish
Properties Physical Mechanical Clinical
WORKING & SETTING TIME Light cure: surface hardens in 60-90 sec Chemical cure: 3-5 min Thermal properties the thermal coefficient of expansion for complete resins is greater than for crown of tooth Natural tooth-11.4 10-6 Amalgam -25 10-6 Hybrid & macrofilled composites-30-40 10-6
Polymerization shrinkage Multipurpose composite 0.7 to 1.4% Microfill composite 2 to 3% Packable composite 0.6 to 0.9% Macrofilled composite 1.2 to 1.3% Small particle filled composite 2 to 3% Nanocomposite and other types yet to be determined Incremental tecnique GIC as base