Plasma Exchange in Treatment of PANS - Overview and Considerations
Plasmapheresis, a type of apheresis, plays a crucial role in managing Pediatric Acute-onset Neuropsychiatric Syndrome (PANS) and Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS). This treatment involves separating the extracellular component of blood from the cellular component, aiding in the removal of harmful antibodies or toxins. The history, classification, typical setup, and mechanisms of plasma removal are discussed, highlighting the advancements in this therapeutic approach. The team at Virginia Commonwealth University has been actively involved in evaluating the effectiveness of plasmapheresis in treating patients with PANS.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
PLASMAPHERESIS IN TREATMENT OF PANS Wei Zhao, MD, PhD Professor and Chief Division of Allergy and Immunology Department of Pediatrics Virginia Commonwealth University
Conflict of Interest None
OBJECTIVES Discuss the role of plasma pheresis in management of PANS and PANDAS. Summarize the result and outcome of patients receiving plasma pheresis in our institution.
VCU Health Team Members Wei Zhao, MD, PhD: Pediatric Allergy and Immunology David Jaffe, MD: Pediatric Neurology Bela Sood, MD: Pediatric Psychiatry Parna Prajapati, MD: Pediatric Psychiatry William Koch, MD: Pediatric Infectious Disease Arin Barker, RN: Nurse Coordinator.
TERMINOLOGY Apheresis: The blood of a person is passed through an apparatus that separates out one particular constituent and returns the reminder to the circulation. Plasmapheresis Extracellular component of blood is separated from the cellular component. Therapeutic Plasma Exchange Plasma is separated from cellular component. The latter is returned to patient with a colloid or crystalloid substitute.
HISTORY 1000 years BC Blood-letting concept. 1914: Abell, Rowntree, and Turner reported 1stcase of animal model of manual plasma removal with return of corpuscles. Coin the term plasmapheresis . 1952: First used in a patient with hyperviscosity syndrome. 1960: Engineer Georg T. Judson and Emil Freireich developed 1stautomated cell separator in National Cancer Institute. Separation of leukocytes in a centrifuge. Returning all other cellular components and plasma to the donating subject.
CLASSIFICATION Leukocytapheresis (Leukocyte depletion) Thrombocytapheresis (Platelet depletion) Erythrocytapheresis (Red blood cell collection) Pleasmapheresis (Plasma collection/separation) Hematopoietic stem cell (HSC) collection Exchange a blood component Erythrocytes (red cell exchanges [RCE]) Plasma exchange (TPE)
TYPICAL SETUP Ogawa. Contrib Nephrol. 2018;196:194
MECHANISMS OF PLASMA REMOVAL Centrifugation-based Filtration-based Efficiency of removal Y/Y0 = e-x Y0. serum concentration before plasma exchange. Y. serum concentration after plasma exchange. x. number of plasma volumes exchanged. 1-1.5 plasma volume exchange will remove 70% of any substance located in the intravascular compartment (1TPV = 63.2%, 1.5TPV = 77.7%, 2TPV = 86.5%)
TPE in Neurological Disorders Inflammation leads to breach of blood-brain barrier. Immune cross-talk between periphery and CNS. Proinflammatory cytokines cross BBB by active transcellular receptor- dependent mechanism. Autoimmune induction occurs outside of CNS in Ab-mediated CNS diseases. Idealized Kinetics of TPE
Complications of TPE Potentially life-threatening complications Multi-organ failure secondary to thrombotic thrombocytopenic purpura, hemorrhage related to anticoagulation therapy for pulmonary embolism, sickle-cell disease with DIC. Most of them were non-neurological indications. Complications of central venous access Infection. Line obstruction. Depletion of non-pathogenic blood components Immunoglobulin. Coagulation factors. Anemia . Electrolyte derangements
Therapeutic Effect of Plasma Removal Remove pathological Abs proliferation of B cells, plasma cells, sensitizing them to immunosuppressants Remove immune complex Replace missing components Remove cytokines Change lymphocyte numbers T regulatory and T suppressor cells Restore Th1/Th2 ratio ( Th1) Reevers. Br J Haemtol. 2014;164:342
Therapeutic Plasma Exchange (TPE) Most commonly used to treat expending number of clinical disorders. American Society for Apheresis (ASFA) guidelines update every 2 yrs to include latest clinical and scientific evidence for the proper use of TPE. Removing the patient s plasma and replacing it with either plasma, plasma and albumin, or albumin alone. Most TPE indications are for those mediated by antibodies in which removal of these offending antibodies is critical to improve symptoms and reduce clinical complications associated with these antibodies.
ASFA 2019 Guidelines 2019 guideline writing committee comprised 13 members from diverse fields including Transfusion Medicine/Apheresis, Hematology/Oncology, Pediatrics, Nephrology, and Critical Care Medicine from US and Europe. Each Therapeutic Apheresis is indicated in 84 diseases where the term disease refers to a specific disease or medical condition. PANDAS is listed as Category 2, Grade 1B recommendation Cat. 2: Apheresis is accepted as 2nd-line therapy, either as a stand alone treatment or in conjunction with other modes of treatment. Grade 1B: Strong recommendation, moderate quality evidence, can apply to most patients in most circumstances without reservation. Padmanabhan. J Clin Apher. 2019;34:171
ASFA 2019 Guidelines Padmanabhan. J Clin Apher. 2019;34:171
Dr. Swedo 1999 Perlmutter. Lancet. 1999;354:1153
Latimer 2015 Latimer. J Child Ado Psycho. 2015;25:70
Cunningham Panel vs Improvement Shimasaki. J Neuroimmunol. 2020;339:577138
OUR EXPERIENCE From 2013 2021, 46 patients underwent 50 plasma exchange Patients include PANDAS and PANS
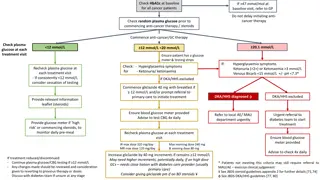
Patient Selection Met published diagnostic criteria Sigra. Neuroscinece and Biobehavioral Rev. 2018;86:51
Patient Selection Symptoms resistant to treatment with antibiotics and/or steroid Evidence of Strep infection/persistent elevated titers of strep and/or Mycoplasma titers, or Abnormal Cunningham panel ( 1) or Referred by outside neurologist/immunologist with existing diagnosis and have undergone extensive treatment
Procedure Out-patient setting in apheresis unit Prior to first session IR double-lumen tunneled Permacath placement (right internal jugular vein) under sedation. Total of 6 sessions in every other day schedule (typically, M.W.F x 2 weeks) After last session, catheter removed by IR service First follow-up 3 months after pheresis, data included 6 months after. Majority cases were approved by insurance Had one line infection
Case Example 10 yr old boy presented to our Immunology Clinic with history of strep infection, abrupt onset of symptoms Extreme Anxiety, OCD, Acute weight loss, Severe sleep disturbance, Mild tics Urgent Peds Neurology Consult Prompt Psychiatric Visit Initial response to antibiotics Fail to taper oral steroid Urgent case conference (Immunology, neurology, psychiatry) TPE performed urgently 100% resolution of symptoms. Followup up to 1 yr doing well.
SUMMARY A total of 46 patients with PANS and PANDAS underwent 50 TPE in our institution. Overall response rate over 70%. However, 11% showed no response. Both PANS and PANDAS equally responded to TPE treatment. There is a trend of higher response in Cunningham Panel positive patients to TPE. However, due the small sample size of Cunningham Panel negative group. No statistical significance was observed. 4 patients received 2nd round of TPE treatment (1-2 yrs interval). Multidisciplinary approach is desired. Larger sample size and long term followup needed to better understand the efficacy of TPE.