Comprehensive Overview of Infectious Diseases: Classes and Historical Perspectives
Infectious diseases are a significant public health concern, with various classes and prevention strategies discussed in a structured educational setting. The course covers topics ranging from antibiotic stewardship to viral infections, providing insights into the historical perspective of infectious agents. Definitions and transmission methods of infectious diseases are also elucidated, offering a holistic understanding of the field.
- Infectious Diseases
- Antibiotic Stewardship
- Prevention Strategies
- Historical Perspective
- Transmission Methods
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
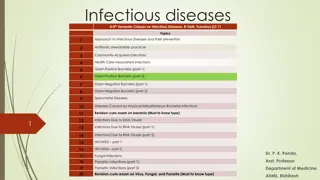
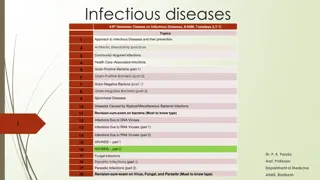
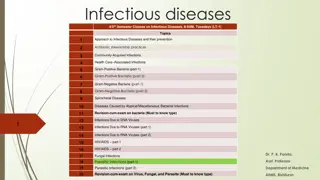
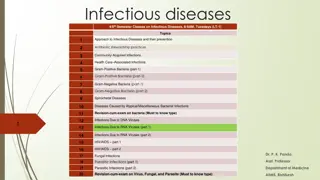
Infectious diseases 4/5thSemester Classes on Infectious Diseases, 8-9AM, Tuesdays (LT-1) Topics Approach to Infectious Diseases and their prevention 1 Antibiotic stewardship practices 2 Community-Acquired Infections 3 Health Care Associated Infections 4 Gram-Positive Bacteria (part-1) 5 Gram-Positive Bacteria (part-2) 6 Gram-Negative Bacteria (part-1) 7 Gram-Negative Bacteria (part-2) 8 Spirochetal Diseases 9 Diseases Caused by Atypical/Miscellaneous Bacterial Infections 10 Revision-cum-exam on bacteria (Must to know type) 11 1 Infections Due to DNA Viruses 12 Infections Due to RNA Viruses (part 1) 13 Infections Due to RNA Viruses (part 2) 14 HIV/AIDS part 1 15 HIV/AIDS part 2 16 Dr. P. K. Panda, 17 18 Fungal Infections Parasitic Infections (part 1) Asst. Professor Department of Medicine 19 Parasitic Infections (part 2) AIIMS, Rishikesh 20 Revision-cum-exam on Virus, Fungal, and Parasite (Must to know type)
Historical perspective 2 Infectious agents have probably always caused disease in humans and recently are second leading cause of death worldwide Miasma (bad air) can be traced back to at least mid-sixteenth century Smallpox in ancient Egyptian and Chinese writings; malaria and poliomyelitis have existed since ancient times In the 20th Century, influenza & AIDS may have killed up to 50 and 20 million people respectively worldwide Bacteria were discovered in 1675 by Antony van Leeuwenhoek, but it wasn t until 1876 that a German physician named Robert Koch first demonstrated that specific diseases are associated with particular microorganisms (Koch s Postulates)
Definitions and Terms 3 Disease a pathological condition of body parts or tissues characterized by an identifiable group of signs and symptoms Infectious disease disease caused by an infectious agent such as a bacterium, virus, protozoan, or fungus that can be passed on to others Infection occurs when an infectious agent enters the body and begins to reproduce; may or may not lead to disease Pathogen an infectious agent that causes disease Host an organism infected by another organism Virulence the relative ability of an agent to cause rapid and severe disease in a host
Transmission of Infectious Diseases 4 Agents that cause infectious diseases can be transmitted in many ways Through the air Through contaminated food or water Through body fluids By direct contact with contaminated objects By animal vectors such as insects, birds, bats, etc.
Infectious Agents & Host Interactions 5 Microbial encounter with and entry into the host Microbiome (the collection of microbial genomes residing in or on mammalian organisms) Microbial growth after entry Avoidance of innate host defences Resistance to killing within the macrophage by herpes-type viruses, measles virus, poxviruses, Salmonella, Yersinia, Legionella, Mycobacterium, Trypanosoma, Nocardia, Histoplasma, Toxoplasma, and Rickettsia Tissue invasion and tropism - Compared with viral tissue tropism, the tissue tropism of bacterial and parasitic infections has not been as clearly elucidated Tissue damage Host response (Inflammasomes) Transmission to new hosts
Phases of infectious diseases 7 Incubation period time between infection and the appearance of signs and symptoms Prodromal phase mild, nonspecific symptoms that signal onset of some diseases Clinical phase a person experiences typical signs and symptoms of disease Decline phase - subsidence of symptoms Recovery phase symptoms have disappeared, tissues heal, and the body regains strength
Classification of infectious diseases 8 By duration Acute develops and runs its course quickly Chronic develops more slowly and is usually less severe, but may persist for a long, indefinite period of time Latent characterized by periods of no symptoms between outbreaks of illness By location Local confined to a specific area of the body Systemic a generalized illness that infects most of the body with pathogens distributed widely in tissues By timing Primary initial infection in a previously healthy person Secondary infection that occurs in a person weakened by a primary infection
Taxonomy Prions Size 30 50 kD Site of PropagationExamples Intracellular Disease Creutzfeld-Jacob disease Poliomyelitis Prion protein 9 Viruses 20 300 nm Obligate intracellular Obligate intracellular Extracellular Poliovirus Bacteria 0.2 15 m Chlamydia trachomatis Streptococcus pneumoniae Mycobacterium tuberculosis Candida albicans Thrush Histoplasma capsulatum Trypanosoma gambiense Trypanosoma cruzi Chagas disease Trachoma, urethritis Pneumonia Facultative intracellular Extracellular Facultative intracellular Extracellular Tuberculosis Fungi 2 200 m Histoplasmosis Protozoa 1 50 m Sleeping sickness Facultative intracellular Obligate intracellular Extracellular Leishmania donovani Wuchereria bancrofti Trichinella spiralis Kala-azar Helminths 3 mm 10 m Filariasis Intracellular Trichinosis
Approach to the Acutely Ill Infected febrile Patient 10 Before the history is elicited and a physical examination is performed, an immediate assessment of the patient s general appearance HISTORY - Presenting symptoms are frequently nonspecific Exposure History, Social history, Dietary habits, Animal exposures, Travel history, Host-Specific Factors PHYSICAL EXAMINATION - A complete physical examination should be performed, with special attention to several areas that are sometimes given short shrift in routine examinations DIAGNOSTIC WORKUP (Laboratory and radiologic testing) - After a quick clinical assessment, diagnostic material should be obtained rapidly and antibiotic and supportive treatment begun Blood (for cultures; baseline complete blood count with differential; measurement of serum electrolytes, blood urea nitrogen, serum creatinine, and serum glucose; and liver function tests) can be obtained at the time an IV line is placed and before antibiotics are administered The blood lactate concentration also should be measured
Laboratory Diagnosis of Infectious Diseases 12 Direct detection refers to detection of pathogens without the use of culture MICROSCOPY AND STAINING - wet mount is the simplest method, others will be discussed next MACROSCOPIC ANTIGEN DETECTION - Latex agglutination assays and EIAs DETECTION OF PATHOGENIC AGENTS BY SEROLOGIC METHODS CULTURE NUCLEIC ACID TESTS
Techniques Gram stain Acid-fast stain Infectious Agents Most bacteria Mycobacteria, nocardiae (modified) Fungi, legionellae, pneumocystis Fungi, amebae Cryptococci Campylobacteria, leishmaniae, malaria parasites All classes All classes All classes 13 Silver stains Periodic acid Schiff Mucicarmine Giemsa Antibody probes Culture DNA probes
Empirical antibiotic therapy is critical and should be administered without undue delay 14
Prevention 16 Every disease has certain weak points susceptible to attack. The basic approach in controlling disease is to identify these weak points and break the weakest links in the chain of transmission.
I. Controlling the reservoir If the first link in the chain of causation is deemed to be the weakest link, logically, the most desirable control measure would be to eliminate the reservoir or source, if that could be possible Elimination of the reservoir may be pretty easy with the animal reservoir but is not possible in humans But we can reduce the quantity of the agent available for dissemination by: 18
(1) EARLY DIAGNOSIS 19 The first step in the control of a communicable disease is its rapid identification (2) NOTIFICATION Once an infectious disease has been detected (or even suspected), it should be notified to the local health authority whose responsibility is to put into operation control measures, including the provision of medical care to patients, perhaps in a hospital
Under the International Health Regulations (IHR) certain prescribed diseases are notified by the national health authority to WHO. These can be divided into : 20 Those diseases subject to International Health Regulations (1969). Third Annotated Edition. 1983: cholera, plague, and yellow fever Diseases under surveillance by WHO - louse- borne typhus fever, relapsing fever, paralytic polio, malaria, viral influenza, etc
(3) EPIDEMIOLOGICAL INVESTIGATIONS An epidemiological investigation is called for whenever there is a disease outbreak 21 (4) ISOLATION Isolation is the oldest communicable disease control measure. It is defined as "separation, for the period of communicability, of infected persons or animals from others in such places and under such conditions, as to prevent or limit the direct or indirect transmission of the infectious agent from those infected to those who are susceptible, or who may spread the agent to others"
Period of isolation recommended Disease Duration of isolation Chickenpox Until all lesion crusted about 6 days after onset of rash. From the onset of catarrhal stage thought 3rd day of rash. Measles Diphtheria Cholera 3 days after tetracycline started, until 48 hours of antibiotics/or negative culture after treatment. Shigellosis Until 3 consecutive negative stool cultures. Salmonellosis Until 3 consecutive negative stool cultures. Hepatitis A 3 weeks. Influenza 3 days after onset. Polio 2 weeks adult, 6 weeks pediatrics. Mumps Until swelling subsides. Pertussis 4 weeks or until paroxysm cease. Meningococcal inf. Until the first 6 hours of effective antibiotic therapy are completed. Streptococcal pharyng. Until the first 6 hours of effective antibiotic therapy are completed. 22
(5) TREATMENT The object of treatment is to kill the infectious agent when it is still in the reservoir, i.e. before it is disseminated Treatment reduces the communicability of disease, cuts short the duration of illness and prevents development of secondary cases. Treatment is also extended to carriers (6) QUARANTINE In contrast to isolation, quarantine applies to restrictions on the healthy contacts of an infection. With better techniques of early diagnosis and treatment, quarantine, as a method of disease control, has become outdated. It has been replaced by active surveillance 23
II. Interruption of transmission 24 A major aspect of communicable disease control relates to breaking the chain of transmission. This may mean changing some components of man s environment to prevent the infective agent from a patient or carrier from entering the body of susceptible host
III. The susceptible host 25 They my be protect by: Active immunization Active immunization is one of the most powerful and cost-effective weapons of the modern medicine, e.g. for cholera, plague, etc Passive immunization is a short-term expedient useful only when exposure to infection has just occurred or is imminent within the next few days. The duration of immunity induced is short and variable-1-6 weeks Combined active and passive immunization
Chemoprophylaxis 27 Chemoprophylaxis implies the protection from, or prevention of, disease Cholera Tetracycline or furazolidone(furoxone) for house-hold contacts/Selective chemoprophylaxis (one dose of doxycycline) Diphtheria Erythromycin and first dose of vaccine. Plague Tetracycline for contacts of pneumonic plague. Meningococcal meningitis Sulphadiazine for 4 days only if strain is shown to be no- resistant, for household contacts;immunization against serogroups A, C, Y, W135; rifampin, ciprofloxacin; and close community
A CDC Framework for Preventing Infectious Diseases 28 Element 1 Element 2 Element 3 Strengthen public health fundamentals, including infectious disease surveillance, laboratory detection, and epidemiologic investigation Identify and implement high impact public health interventions to reduce infectious diseases Develop and advance policies to prevent, detect, and control infectious diseases
Emerging & Re-emerging of infectious diseases 29 Human demographics and behaviour are among the many variables that contribute to the emergence of infectious diseases Microbial adaptation to widespread antibiotic use contributed to the emergence of drug resistance in many species, including Mycobacterium, gonorrhoeae, Staphylococcus, Salmonella, Enterococcus, and Malaria Some infectious agents are genuinely new to humans, e.g., HIV, which causes AIDS, and B. burgdorferi, which causes Lyme disease Surprising number of new infectious agents continue to be discovered
30 2015 Zika virus Microcephaly and Guillain-Barr syndrome
Category B Microbial Bioterrorism Category A Category C Agents Of Bioterrorism anthracis) Botulism (Clostridium botulinum toxin) Plague (Yersinia pestis) Smallpox (Variola major virus) Tularemia (Francisella tularensis) Viral hemorrhagic fevers (filoviruses [e.g., Ebola, Marburg] and arenaviruses [e.g., Lassa, Machupo]) Anthrax (Bacillus Brucellosis (Brucella sp.) Epsilon toxin of Clostridium perfringens Food safety threats (e.g., Salmonella sp., Escherichia coli O157:H7, Shigella) Glanders (Burkholderia mallei) Melioidosis (Burkholderia pseudomallei) Psittacosis (Chlamydia psittaci) Q fever (Coxiella burnetti) Ricin toxin from Ricinus communis (castor beans) Staphylococcal enterotoxin B Typhus fever (Rickettsia prowazekii) Viral encephalitis (alphaviruses [e.g., Venezuelan equine encephalitis, eastern equine encephalitis, western equine encephalitis]) Water safety threats (e.g., Vibrio cholerae, Cryptosporidium parvum Emerging infectious disease threats such as Nipah virus, Hantavirus, SARS or MERS coronavirus, and pandemic influenza 31
Thank you 32