Management of Chronic Kidney Disease: Work-Up and Treatment Strategies
This presentation discusses the work-up and management of chronic kidney disease (CKD) before nephrology referral. It covers the definition of CKD, work-up steps including history and investigations, and management strategies such as treating underlying causes, controlling risk factors, and lifestyle interventions. The case of a 72-year-old male with CKD is also presented, highlighting key considerations in patient assessment and care.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Management of Chronic Kidney Disease; Before the Nephrologist Stuart McAdam, MD, FRCPC General Internal Medicine The Moncton Hospital April 2022
Conflicts of Interest Nothing to disclose 2
Objectives Describe an approach to the work-up of chronic kidney disease (CKD) Outline an approach to the management of CKD Describe the indications for dialysis Understand when you should refer to a Nephrologist 3
Case 72 yo M referred for management of CKD PMH: HTN, Diabetes, CKD, Smoker Meds: Perindopril 4mg daily, Metformin 500mg BID, Semaglutide 0.5mg subcut weekly Feels like he s getting old, some mild edema O/E : BP 148/70, HR 82, sats 96% RR 16, weight 70kg Regular pulse, JVP 5cm, Normal S1/S2 no EHS or murmurs, lungs clear, abdo soft, non-tender, mild edema bilaterally Labs: Na 133, K 4.8, HCO3-18, Cl 100, Cr 150 (was 148 six months ago), Urea 6.8, GFR ~40ml/min/1.73cm2 WBC 9, HgB 98, Plts 230, Albumin 38, Calcium 2.20, Phos 1.10, PTH 7, Alk P 70, U ACR 300mg/g, A1c 7.0,ECHO Jan 2022 Diastolic dysfunction. 4
Chronic Kidney Disease CKD: Defined as abnormalities of kidney structure or function for >3 months1 Estimated 700 million people have CKD2 1. KDIGO Kidney Int 2013 2. Webster et al. Lancet 2017 5
CKD Work-Up History Exclude nephrotoxins Risk factors (Diabetes, HTN, Smoking, Obesity, Family History, Age) General review of systems Physical BP, Volume Status Investigations CBC, Lytes, Ext Lytes, HCO3, Cr, Urea, PTH, Alk P, Urinalysis, U ACR, Kidney U/S , Iron Studies, Lipid Profile, A1c Further Investigations guided by situation may include: SPEP, Free light chains, ANCAs, Anti-GBM, ANA, Anti-dsDNA, C3, C4, HIV, Hep B, Hep C, Cryoglobulins, Kidney biopsy 6
Management of CKD Treat underlying cause Treat risk factors: Ensure HTN, DM well controlled Restrict sodium intake to <2g sodium/day1 *Key point* Sodium increases BP and proteinuria, and blunts response to RAAS blockade Lifestyle 150 minutes of moderate intensity exercise per week. Healthy weight, No smoking Renally adjust medications, and avoid nephrotoxins Multidisciplinary care team Manage complications 1. KDIGO Kidney Int 2013 7
Blood Pressure in CKD ACE-I or ARB first line if proteinuric CKD3 Re-check lytes and Cr in about 2 weeks Continue unless Cr increases >30% within 4 weeks Sprint CKD Criteria GFR 20- 59, <1g proteinuria/day or ACR<600mg/g4 If diabetic <130/80 3. Rabi J .et al. Canadian Journal of Cardiology 2020 8 4. The SPRINT Research Group. N Engl J Med 2015
Dyslipidemia in CKD5 5. Pearson et al. Canadian Journal of Cardiology 2021 9
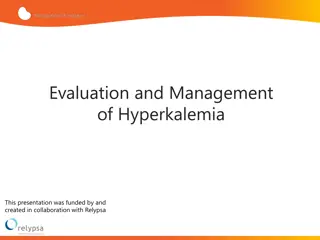
Hyperkalemia in CKD Potassium restricted diet Optimize acid-base status Review medications that could contribute Continue ACE-I/ARB if you can, but may need to reduce dose or stop Add diuretic if indication Potassium binders Sodium Polystyrene Sulfonate (Kayexalate) Patiromer Sorbitex Calcium (Veltassa) and Sodium Zirconium Cyclosilicate (Lokelma) Dialysis Management acutely is separate 12
Volume Overload Target euvolemia Sodium restriction Diurese as needed to target euvolemia *Key Point* Regardless of creatinine 13
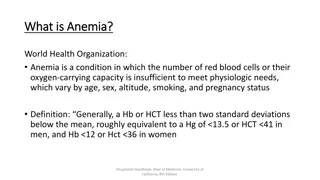
Anemia in CKD Do usual work-up for anemia Supplement iron if ferritin 500 and TSAT 30%7 *Key Point* Suggest not using erythropoietin stimulating agent (ESA) if HgB 100 If HgB 100 despite optimizing iron stores, consider ESA after weighing risks and benefits Suggest not targeting a HgB above 115 with ESA 7. KDIGO Anemia CKD. Kidney Int 2012 14
Acid Base in CKD Target bicarbonate 22 with oral bicarbonate supplementation1 15.4 to 23.1 mEq/day sodium bicarb in divided doses Typically start around 500-650mg BID then titrate 1. KDIGO Kidney Int 2013 15
CKD Mineral and Bone Disorder Target phosphate in normal range1,8 Phosphate binders If hypercalcemic avoid ones containing calcium Secondary hyperparathyroidism Optimal PTH level not known If persistently high look to optimize risk factors; hypocalcemia, hyperphosphatemia, vitamin D deficiency Consider calcitriol in CKD stage 4-5 with severe and progressive hyperparathyroidism Increased risk of osteoporosis 1. KDIGO Kidney Int 2013 8. KDIGO CKD-BMD Kidney Int 2017 16
Proteinuria 9. McFarlane et al. Can J Diabetes 2018 17
Proteinuria Non-diabetic CKD: ACE-I or ARB if albumin excretion >300mg/day1 Diabetic CKD: ACE-I or ARB if >30mg/day or ACR 2mg/mmol ACE-I and ARB are nephroprotective, reduce progression of CKD and proteinuria10 Monitor electrolytes and renal function, careful the lower the GFR Sodium restricted diet <2g sodium/day SGLT-2 inhibitors11 10. Hou et al. NEJM 2006 11. Heerspink et al. NEJM 2020 1. KDIGO Kidney Int 2013 18
4303 participants with GFR 25 to 75 and urine ACR 200 to 5000 mg/g Randomized to Dapagliflozin 10mg daily or placebo All patients were on stable dose of ACE-I or ARB, unless unable Primary Outcome sustained decline in GFR of at least 50%, ESRD, or death from renal or cardiovascular causes Primary outcome in 9.2% Dapagliflozin vs 14.5% placebo, HR 0.61 p<0.001 Dapagliflozin discontinued in 12.7% vs 14.4% placebo, amputation rate 1.6% vs 1.8% placebo, major hypoglycemia 0.7% vs 1.3% placebo, no DKA with Dapa, volume depletion 5.9% vs 4.2% placebo (p=0.01) 11. Heerspink et al. NEJM 2020 19
4401 patients with GFR 30 to 89 and urine ACR 300 to 5000mg/g Canagliflozin 100mg daily or placebo Were also treated with renin-angiotensin system blockade Primary outcome ESRD, doubling of creatinine, or death from renal or cardiovascular causes Primary outcome improved in canagliflozin, HR 0.70 p=0.00001 No difference in amputations, there were higher rates of DKA with canagliflozin 0.5% vs 0.05% 12. Perkovic V et al. NEJM 2019 21
Indications for Dialysis AEIOU Refractory to medical management Acidosis Electrolyte abnormalities hyperkalemia Intoxication certain toxicities Overload volume overload Uremia cognitive impairment, pruritis, loss of appetite, pericarditis 1. KDIGO Kidney Int 2013 24
When to refer to Nephrology in CKD AKI or abrupt sustained fall in GFR GFR < 30 cc/min/1.73 m2 Consistent significant albuminuria (ACR 300mg/g or AER 300mg/day, approx. equal to PCR 500mg/g or PER 500mg/day Progression of CKD Urinary red cell casts, >20 RBCs per hpf sustained and not explained CKD and HTN refractory to treatment with 4 or more antihypertensive agents Persistent abnormalities of serum potassium Recurrent or extensive nephrolithiasis Hereditary Kidney Disease Indication for dialysis 1. KDIGO Kidney Int 2013 25
Back to the Case 72 yo M referred for management of CKD PMH: HTN, Diabetes, CKD, Smoker Meds: Perindopril 4mg daily, Metformin 500mg BID, Semaglutide 0.5mg subcut weekly Feels like he s getting old, some mild edema O/E : BP 148/70, HR 82, sats 96% RR 16, weight 70kg Regular pulse, JVP 5cm, Normal S1/S2 no EHS or murmurs, lungs clear, abdo soft, non-tender, mild edema bilaterally Labs: Na 133, K 4.8, HCO3-18, Cl 100, Cr 150 (was 148 six months ago), Urea 6.8, GFR ~40ml/min/1.73cm2 WBC 9, HgB 98, Plts 230, Albumin 38, Calcium 2.20, Phos 1.10, PTH 7, Alk P 70, U ACR 300mg/g, A1c 7.0,. ECHO Jan 2022 Diastolic dysfunction. 26
Case Stage 3 CKD, likely from diabetes, hypertension Order urinalysis, kidney U/S, SPEP Treat risk factors: Target BP <130/80, DM control, quit smoking Diet: Salt restrict <2g sodium /day. Education on low potassium diet Edema: Diurese, start furosemide 27
Case Hypertension: Target <130/80, optimize fluid status, and perindopril, monitor lytes, renal function Proteinuria: Optimize perindopril, SGLT2- Inhibitor in time Acidosis: Start sodium bicarbonate Anemia: Order usual work-up, optimize iron stores Dyslipidemia: Order lipid profile, start statin 28
Take Home Points Sodium restrict patients with CKD Optimize volume status, diurese as needed ACE-I/ARB and SGLT2-I to reduce proteinuria, progression of CKD Optimize iron stores in anemic patients 29
References 1. Kidney Disease: Improving Global Outcomes (KDIGO) KDIGO 2012 Clinical Practice Guidelines for the Evaluation and Management of Kidney Disease. Kidney Int. 2013; 3: 1-163 2. Webster AC, Nagler EV, Morton RL, Masson P. Chronic kidney disease. Lancet 2017; 389: 1238-52. 3. Rabi D, McBrien K, Sapir-Pichhadze R, Nakhla M, Ahmed S. Hypertension Canada s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology 2020; 36: 596-624 4. The SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015; 373:2103-16 5. Pearson G, Thanassoulis G, Anderson T, Barry A, Couture P. 2021 CCS guidelines for the management of dyslipidemia for the prevention of cardiovascular disease in adults. Canadian Journal of Cardiology 2021; 37: 1129-1150 6. Quaife, P. (n.d.). Retrieved March 16, 2022, from https://www.pinterest.co.uk/pin/564849978237603369/?mt=login 7. Kidney Disease: Improving Global Outcomes (KDIGO) Clinical Practice Guideline for Anemia in Chronic Kidney Disease. Kidney Int. 2012; 2: 279-335 8. Kidney Disease: Improving Global Outcomes (KDIGO) Clinical Practice Guidelines Update for the Diagnosis, Evaluation, Prevention, and Treatment of CKD-MBD. Kidney Int. 2017; 7:1-59 9. McFarlane P, Cherney D, Gilbert R, Senior P. Chronic Kidney Disease in Diabetes. 2018 Clinical Practice Guidelines. Can J Diabetes. 2018;42:S201- S209 10. Hou F, Zhang X, Zhang G, Xie D, Chen P. Efficacy and Safety of Benazepril for Advanced Chronic Renal Insufficiency. N Engl J Med 2006; 354:131-140 11. Heerspink H, Stefansson B, Rotter R, Chertow G, Greene T et al. Dapagliflozin in Patients with Chronic Kidney Disease. N Engl J Med 2020; 383:1436-1446 12. Perkovic V, Neal K, Bompoint S, Heerspink H, Charytan D et al. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. N Engl J Med 2019; 380:2295-2306 30
Questions? 31