Operational Planning Guidance for Health Inequalities Priorities 2021/2022
The guidance outlines key priorities to address health inequalities, focusing on equitable access, excellent outcomes, and personalized care. It emphasizes tackling disparities in healthcare outcomes, workforce diversity, and economic recovery, with a strong emphasis on data collection, preventative programs, and leadership accountability.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
2021/2022 operational planning guidance: health inequalities priorities March 2021 NHS England and NHS Improvement
Contents Overview of health inequalities (HI) priorities 5 specific HI deliverables Elective recovery expectations Programme-specific deliverables Submission timeline National HI improvement programme approach NEY available support 2 |
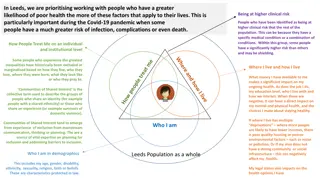
Planning guidance priorities Aim to deliver equitable access, excellent experience and optimal outcomes. Delivery through population health management approaches at place level 5 key priorities for first six months (see next slide) Elective recovery funding aligned to a focus on health inequalities within long waiters (ethnicity and deprivation) monthly progress criteria to be met Continued targeted COVID vaccination approaches among under-represented groups Funding to tackle inequalities of outcome on cancer, cardiovascular disease, mental health and maternity services System prevention plans for LTP deliverables, incl. smoking cessation and weight management expansion anddiabetes and CVD prevention Reduced variation in cardiac, MSK and eye care pathways Primary care expansion linked to tackling health inequalities Workforce inequalities, including WRES recommendations, increasing diversity and model employer goal delivery Health and care role in economic recovery Plus flexibility to develop bespoke system plans around health and care priorities that reflect the health inequalities needs of ICS population 3 |
Health inequalities 5 priorities Priority 1: Restore NHS services inclusively with a focus on ethnicity and deprivation Priority 2: Mitigate against digital exclusion through - providers offering face-to-face care to patients who cannot use remote service - more complete data collection to identify who is accessing face-to-face, telephone, or video consultations, broken down by relevant protected characteristic and health inclusion groups - taking account of their assessment of the impact of digital consultation channels on patient access. Priority 3: Ensure datasets are complete and timely - continuing to improve the collection and recording of ethnicity data across primary care, outpatients, A&E, mental health, community services, and specialised commissioning. Mandatory data reporting in primary care and linked data sets. Priority 4:Accelerate preventative programmes that proactively engage those at greatest risk of poor health outcomes incl. a culturally competent approach to COVID & flu vaccination delivery, CoC in maternity for targeted groups, a focus on LTCs and health checks for people with a LD and/or SMI Priority 5: Strength leadership and accountability systems and providers to have a named executive Board-level HI leads and access to training through the Health Equality Partnerships Programme In addition, systems are asked to develop their own set of local health and care priorities that reflect the needs of their population, aligned to the four primary purposes of an ICS: improving outcomes in population health and healthcare tackling inequalities in outcomes, experience and access enhancing productivity and value for money helping the NHS support broader social and economic development. 4 |
Elective recovery through a health inequalities lens Health inequalities within elective recovery will form one strand of the gateway criteria that systems will be required to demonstrate progress against on a monthly basis. Systems are required to demonstrate that plans for elective recovery will: Use waiting list data (pre and during pandemic), including for clinically prioritised cohorts, to identify disparities in relation to the bottom 20% by Index of Multiple Deprivation (IMD) and black and minority ethnic populations Prioritise service delivery by taking account of the bottom 20% by IMD and black and minority ethnic populations for patients on the waiting list and not on the waiting list, including through proactive case finding Use system performance frameworks to measure access, experience and outcomes for black and minority ethnic populations and those in the bottom 20% of IMD scores Evaluate the impact of elective recovery plans on addressing pre-pandemic and pandemic-related disparities in waiting lists, including for clinically prioritised cohorts Demonstrate how the ICS s SRO for health inequalities will work with the Board and partner organisations to use local population data to identify the needs of communities experiencing inequalities in access, experience and outcomes and ensure that performance reporting allows monitoring of progress in addressing these inequalities. Regional teams will review progress against the agreed deliverables on a monthly basis to determine if the gateway criteria are being met. 5 |
Programme-specific expectations Mental health, Learning Disabilities and Autism Improved LD health check delivery GP LD register improvements and intersectionality links made (C&YP, ethnicity etc) Delivery of actions emerging from LeDeR reviews SMI health checks Delivery of actions within Advancing MH Equalities Strategy Primary, community and personalised care Implementing population health management and personalised care approaches to improve health outcomes and address health inequalities in primary and community care Use of additional roles in primary care - Social Prescribing Link Workers, Health and Wellbeing Coaches and Care Coordinators. System and PCN work to address backlog of clinically prioritised long-term condition management reviews, including medication reviews and routine vaccinations (supported by re-introduction of QOF indicators from April) Targeting dental capacity to minimise deterioration in oral health and reduce health inequalities Using risk stratification to provide cross sector support for patients with the greatest health inequalities, complex needs or awaiting multiple appointments, in line with NHS Comprehensive Model for Personalised Care 6 |
Programme-specific expectations Maternity Continuity of carer for 35% of women with the proportion of Black and Asian women and those from deprived communities exceeding the proportion for population as a whole Develop an enhanced model of continuity of carer which provides for extra midwifery time for women from the most deprived areas for implementation from April 2022. LMSs to submit a Perinatal Equity Strategy (covering health outcomes, community assets and staff experience) and a co-production plan by Sept 2021, and Equity Action Plans by December, 2021, to deliver the national Perinatal Equity Strategy Prevention and LTC management Ongoing management of LTCs with a targeted focus on those at greatest risk of the poorest health outcomes Smoking cessation and weight management expansion Diabetes and CVD prevention acceleration ..maintain a focus on improving equalities across all programmes 7 |
Development & submission Health inequalities elements expected to be largely narrative and some quantitative 6 May draft plan submission 3 June final plan submission 8 |
National NHSEI Health Equity Improvement Approach Approach: Social movement approach by which the health inequality gap is closed through QI capability and capacity building from Boards to Frontline underpinned by a leadership culture which promotes and enables quality improvement and continuous learning. Model for Improvement: Quality Improvement work supported by a Health Inequalities Improvement dashboard. Appreciative Inquiry: Asking people and communities what works a) Identify exemplars b) Build from strength Co-production: a) b) Engaging communities in design, implementation & evaluation Genuinely listen with curiosity 9 |
Using a number of domains and lenses Domains and lenses Inclusion Health Disabilities (LD, SMI) Life Course Conditions Wider Ethnicity Deprivation Determinants Role of the NHS at 3 levels Anchor Institution Contributor to the wider determinants of health Commissioner & Provider of Healthcare Integrated Care System Partner 10 |
National support 1. Support System Leadership development 2. Build Capabilities 3. Health Inequalities Improvement Dashboard Across all of these: Hardwire Health Inequalities Improvement into policies & programmes 4. Mobilise Professional Networks 5. Comms Plan / Operating Model 6. Health Inequalities Improvement Framework 11 |
Regional Networks & Connections to support systems with effective delivery & co-ordination of reducing health inequalities KEY Health Inequalities System Regional National NHS England and NHS Improvement
Organisational HI leads PCNs Provider collaboratives/networks LAs VCSE Communities System-level operational groups and HI networks NENC ICS WYH ICS SYB ICS HCV ICS Prevention Workstream Improving Population Health Programme Board System Prevention Workstream Population Health & Prevention Board PHE NEY NHSEI NEY Health & Well-being Teams LKIS Team / C-WorKS platform RDM/Management Exec/Cells ICS Leaders Workforce Improvement Programmes LTP Programmes: Learning Disabilities & Autism Cross-cutting digital, personalised care, workforce, commitment to carers Life Course Maternity, Children & Young People, Ageing Well Settings Primary Care, In Hospital & Out of Hospital Care, Spec Comm (Homelessness) etc. LTCs Cancer, Diabetes, Mental Health, Respiratory NEY Peer Health Inequalities Group (AHSN-led): Edward Kunonga & Lisa Dodds: NENC Sarah Smith: WYH Lisa Kell: SYB Andrew Burnell, Karina Ellis, Stephen Pintus: HCV DPH/PH Networks Cumbria, North East, Yorkshire & Humber Partner Organisations Academic Health Science Networks (AHSNs) NENC, Y&H NEY Regional Health Inequalities Co-ordination Group: Jonathan Slade Rachel Johns Jill Simpson Liz Lingard Matthew Groom Moira Betteridge Helen Dowdy Will Manners Permjeet Dhoot (link to National Team) David Black Mathew James Applied Research Collaboratives (ARCs) NENC, Y&H National Health Inequalities Improvement - Bola Owolabi North East Leadership Academy Health Education England National NHSEI Programmes Race & Health Observatory, Population Health Management (PHM), Prevention Board, Long Term Plan (LTP), Health Equity Partnership Programme (HEPP), Health Anchors Learning Network (HALN), Beneficial Changes Network (BCN)
NEY HI support offer Supporting systems to embed a health equity focus into everything we do, specifically to: Build capabilities and a health equity culture within clinical programmes, places and ICSs through the provision of learning sessions and training Achieve strategic connectivity across all partners to best co-ordinate coherent delivery and channel resources accordingly Ensure 21/22 planning and clinical programme delivery is driven by a health equity focus and aligned to nationally mandated health inequalities priorities, including providing critical friend challenge and support Provide bespoke advice, support and facilitation to recovery priorities Collate and share good practice resources and support tools Drive data quality improvements and analytical use and capacity to inform health equity priorities Ensure future statutory and non-statutory health and care arrangements have a health equity focus and population health management approach (at region, system and place level) Deliver the successful development of the C&YP programme and embedding a life course approach For any training, support or advice requests or to share examples of good practice within your system, place or programme, contact: Jill Simpson: Senior Advisor, NHSEI North East & Yorkshire jill.simpson2@nhs.net Liz Lingard: Transformation Lead, NHSEI North East & Yorkshire liz.lingard@nhs.net 14 |