Surgical History Taking and Patient Evaluation Guidelines
Proper history taking in surgery involves gathering detailed information through patient interview, examination, and investigation. Elements such as chief complaint, past medical history, family history, and social background are vital for accurate diagnosis and treatment planning. This process helps surgeons make informed decisions and provide effective care. Paying attention to small details, being empathetic, and involving patients' relatives can enhance the quality of information obtained. Age, sex, religion, marital status, occupation, and residence all play essential roles in shaping the clinical presentation of surgical conditions. Consideration of these factors can aid in identifying potential diagnoses and tailoring treatment approaches.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
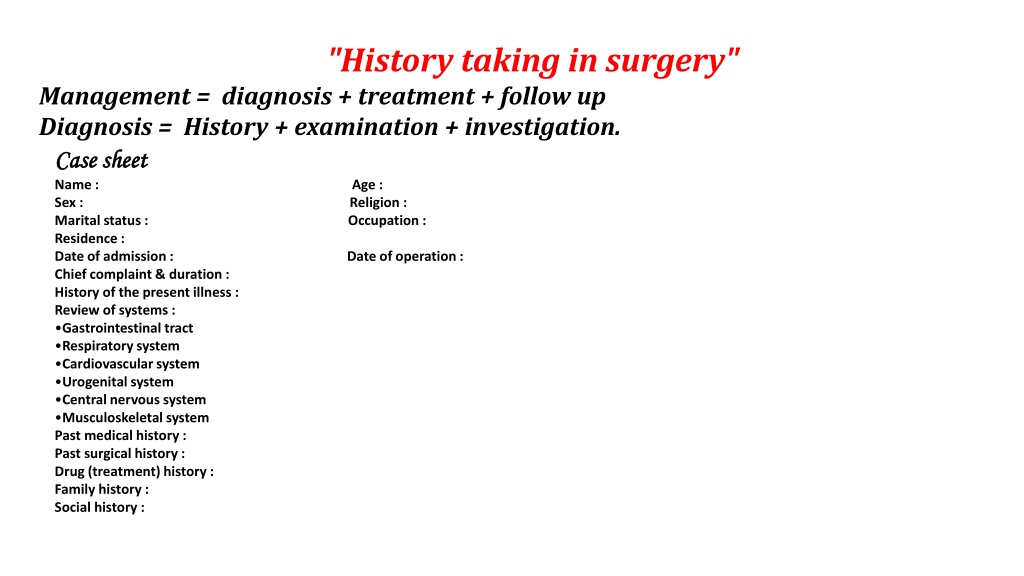
"History taking in surgery" Management = diagnosis + treatment + follow up Diagnosis = History + examination + investigation. Case Case sheet sheet Name : Age : Sex : Religion : Marital status : Occupation : Residence : Date of admission : Date of operation : Chief complaint & duration : History of the present illness : Review of systems : Gastrointestinal tract Respiratory system Cardiovascular system Urogenital system Central nervous system Musculoskeletal system Past medical history : Past surgical history : Drug (treatment) history : Family history : Social history :
History is the key step in the surgical diagnosis. Seeing the patient walking into the room gives some information. Always introduce yourself so that the patient knows to whom he is talking, shake his hand, ask him whether comfortable or not, be social with him. Sometimes the relatives or the accompanying persons (witness) give better history than the patient himself. Do not ask leading questions.
Name (should be triple) :- o For social reasons & to differentiate him. Age :- o e.g. vomiting have different diagnosis in different ages e.g. :- Neonate may be pyloric stenosis Infant may be Intussusceptions Preschoolers may be Mesenteric lymphadenitis Adult may be Peptic ulcer Old age may be CA colon o E.g. volvulus of midgut occurs mostly in early age while volvulus of sigmoid colon occurs mostly in elderly. o E.g. multiple myeloma occurs in elderly while diphtheria & poliomyelitis occur in children.
Sex : - o Disease occurs only in male e.g. benign prostatic hyperplasia,haemophilia. o Disease occurs only in female e.g. uterine fibroid, ovarian disease. o Disease occurs more common in male : inguinal hernia, CA lung, CA esophagus, Hirschsprung's disease. o Disease occurs more common in female : femoral hernia, thyroid disease, gall bladder disease, paraumbilical hernia, urinary tract infection. Religion :- o Muslim : circumcision o Christian : taenia solium o Jewish : in born error of metabolism, inflammatory bowel disease.
Occupation :- o Wool sorter(Anthrax) ,farmers (bird flu), butchers (brucellosis, ),(ofr or pustular dermatitis), job with prolong standing (deep venous thrombosis), hair dresser (pilonidal sinus). Residence :- o Rural : infectious disease, hook worm infestation o Urban : rickets, pneumoconiosis (functional lung disease) o Whether there is endemic area or if there is communicable disease. Marital status :- o Varicose vein in male o Hysterectomy in female o Gonorrhea & other sexually transmitted disease.
Date of admission:- o e.g. 1st of oct.2010 2ed of Dec. 2011 3rd of April 2012 & so on. o To see whether the problem acute or chronic Date of operation :- o The same day of surgery is called day 0 o The next day is called day 1 post operation & so on. o To see the course of hospitalization. Chief complaint & duration :- o It is better not to know the diagnosis. o It is the thing which brings the patient to the doctor. o If more than one; which is more concerned about? o By the patient words not medical term. o For how long this complain & if recurrent attacks; the last episode.
History of the present illness :- o Details of the story from the beginning of the problem until reaching the hospital & taking the proper management. o Do not ask leading question. o Do not interrupt the patient. o Mention the related symptoms of the same system which is abnormal. Review of systems :- o To reveal other disorder unaware by the patient. o Starting with the involved system unless you mentioned in the present illness. o Here you allowed asking direct question. o -ve answered are as important as +ve one. These symptoms you have to know by heart.
"History taking in surgery" Part 2 Gastrointestinal tract:- o Appetite : increased, decreased, changed o Diet : type of food; solid, liquid, salty, sweaty, spicy. o Weight : increase or decrease, clothes get looser or tighter. Relatives or friends notice the change in his weight better than himself. o Swallowing : dysphagia = difficulty in swallowing. Odynophagia = pain with the swallowing. o Nausea : o Regurgitation : effortless return of food into the mouth. o Vomiting : powerful with involuntary contraction of abdominal wall. Mention the frequency, associated with pain or not, type of the vomited materials, amount, color, coffee ground, and the taste.
o Heart burn : burning sensation behind the sternum due to reflux of gastric acid into the esophagus. o Flatulence : wind escape upward (frequent belching) or downward (flatus) & dose it relief the symptoms. o Haematemesis : vomited blood.(Haemoptysis) : coughed up blood. o Indigestion : discomfort after eating. o Abdominal pain : o Abdominal distention : o Jaundice : yellowish appearance of the skin, mucous membrane, sclera. Any change in the color of the stool & urine. Is there any jaundice in the family or friends. Any injection or blood transfusion.
o Defecation : constipation, diarrhea. Never use these words without recording the frequency of bowel motion & the consistency of the stool (watery, formed, and solid). Is the patient taking any purgative drugs or drug causing constipation. If he passed mucous , pus in the stool. If he passed blood in the stool :- Mixed with the stool (infection) On the surface of the stool (fissure) After passing stool (hemorrhoid) Malaena (black tarry stool)
Respiratory system :- o Cough : dry or productive, time of occurrence, aggravating &relieving factors, like cold, pollens , dust. Associated with pain or not. o Sputum : quantity time of expectoration, color, odor, consistency, blood(streaks, clot, or massive). o Wheezing : constant or intermittent, provoking factors. o Haemoptysis : coughed up blood. o Dyspnea : feeling of difficulty in breathing (breathlessness). o Tachpnea : increase respiratory rate (shortness of breath). o Orthopnea : dyspnea on lying flat o Chest pain :
Cardiovascular system :- o Chest pain : o Dyspnea, orthopnea, paroxysmal nocturnal dyspnea : o Palpitation : awareness of heart beats. o Cough : o Haemoptysis : o Sputum : o Dizziness, headache : o leg swelling : o Peripheral vascular system :- o Intermittent claudication : o Pain in limb on rest : o Cold extremities : o Change in color : o Parasthesia (tingling sensation or numbness).
Genitourinary system :- Urinary :- 1-Pain :loin, groin, suprapubic 2-Edema : swelling 3-Urine :- o Color : faint yellow(normal), bloody (hematuria), cloudy (urinary tract infection or could be normal), tea color (obstructive jaundice), dark yellow(concentrated of dehydration), transparent (diluted of polyuria). o Quantity : o Smell : o Hematuria : microscopic & macroscopic o Pneumaturia : air bubbles in urine.
4-Micturition problems :- o Frequency : frequent times o Polyuria : increase amount (volume more than 3000ml/24 hr.) o Oliguria : decrease amount(less than 300 ml / 24 hr.) o Anuria : less than 50 ml /24 hr. o Dysuria : difficult & painful urination o Nocturia : desire to urinate at night o Hesitancy : hesitate in initiation of urination o Latency : delay in starting urination o Intermittency : intermittent stream of urine o Stream of urine : narrow caliber or good o Drippling at the end of micturition.
Genital system :- o Pain in the scrotum o Swelling in the scrotum o Urethral discharge o Menstruation in female :- o Menarche : date of 1st menstrual cycle o Menopause : date of cessation of cycle o Dysmenorrhea : painful menstruation. o Quantity & duration o Amenorrhea : no menstrual cycle o Mid cycle pain : (mittelschmerz syn.): loin pain at the mid cycle due to ovulation.
Central nervous system :- o Mental state : nervous, calm o Consciousness: coma, blackout o Tremor: o Fit (convulsion): o Headache : o Any change in smell, vision. Hearing o Paralysis or weakness in the face o Paralysis or weakness in the limbs(hemipalgia, hemiparesis). o Loss of cutaneous sensation (parasthesia). Musculoskeletal :- o Pain o Swelling in joint o Limitation of joint movement o Congenital deformities
Past medical history :- Common infectious disease, serious illnesses, previous hospitalization, ischemic heart disease, hypertension, diabetes mellitus, T.B, asthma, jaundice, epilepsy, stroke, renal disease. Past surgical disease :- o Previous surgery : cause & if any complication o Anesthetic problems : malignant hyperthermia, scoline apnea. o Blood transfusion o Renal colic o Peptic ulcer o Urinary tract infection
Treatment history :- o Current treatment oral drug or injectable o Chronic usage o Self taken drug o Compliance o Allergies o Steroid & NSAID. o Radiotherapy o Chemotherapy
Family history :- o No. of family member o Patient position in the family o Age of children o Parent dead or alive o Cause of death in the 1st degree relatives o Hereditary disease in the family : atopy, hypertension, diabetes, epilepsy, T.B. Social history :- o Smoking :type (cigar, pipe, cigarette), amount & for how long o Alcohol : amount & for how long o Tattoo o Overseas travelled abroad o Animals at home o Sanitary condition : (water supply, overcrowding)
special History in surgery" History of pain :- o The pain is warning us that are something is going wrong in our body. o Pain : subjective feeling by itself. o Tenderness : feeling of pain in response to stimulus (by the examiner). 1. Site : described in the proper anatomical areas. 2. Time of onset: morning, night, suddenly, insidiously. 3. Severity : effect of pain on the patient activities.
Nature : burning like esophagitis, o throbbing like headache, o stabbing like dissecting aneurysm, o constricting like myocardial infarction, o distending like ascites, o colicky like intestinal colic = (comes & goes, occur in hollow tubular o structure, ask him with example) o just a pain with no character. Progression : steady, gradual worsening, gradual decline, fluctuating. End : suddenly or gradual. Duration.
Relieving factors. Aggravating factors. Radiation : extensions of pain to another site while the initial pain persist o E.G. (perforated DU or pancreatitis in the epigastrium radiate to the back). o Referred pain : pain felt at a distance from its source (cholecystitis pain o referred to right shoulder). o Shifted pain : pain disappears from one site & appear at another site. o (acute appendicitis appears in epigastric region then shifted to the right o iliac fossa region).
History of mass (lump) : - 1. When it was first be noticed.(the lump was firstly appeared = wrong) (the lump was firstly be noticed = right). 1. What made the patient notice the mass (accidentally, pain, by someone else). 2. Symptoms of the mass (pain, disfiguring, interfere with the movement, with respiration, with swallowing). 3. Change in the mass (in size, in shape, in surface, in the pain). 4. Disappearance. 5. Other masses.
History of ulcer :- Ulcer : break in the continuity of an epithelium. 1. When it was first be noticed. 2. What made the patient notice it (pain, discharge, bleeding). 3. Symptoms (pain, interfere with eating, with walking, with defecation) . 4. Change. Other ulcers.