Developing a Surgical Site Infection Bundle for Improved Patient Outcomes
Developing a comprehensive Surgical Site Infection (SSI) bundle to reduce infection rates, including interventions like preoperative chlorhexidine baths, standardized antibiotic protocols, and targeted prophylactic measures. By implementing these strategies, the aim is to lower infection rates below 3% within a year and enhance patient safety during surgical procedures.
- Surgical Site Infection
- Patient Outcomes
- Infection Prevention
- Clinical Protocols
- Healthcare Improvement
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
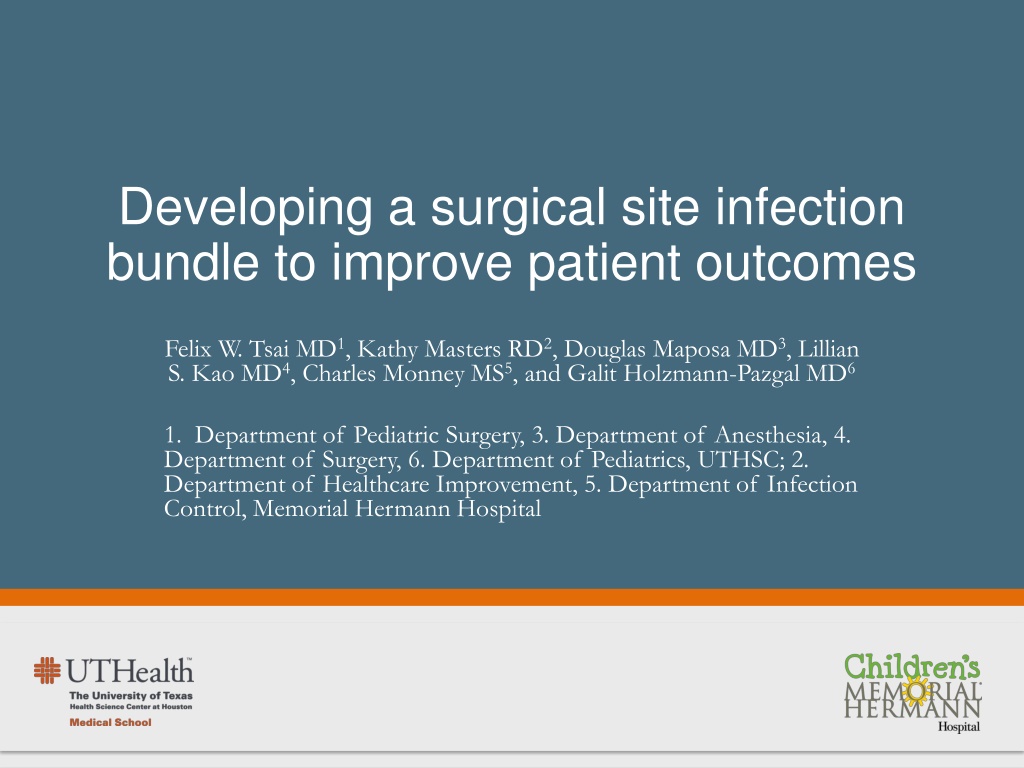
Developing a surgical site infection bundle to improve patient outcomes Felix W. Tsai MD1, Kathy Masters RD2, Douglas Maposa MD3, Lillian S. Kao MD4, Charles Monney MS5, and Galit Holzmann-Pazgal MD6 1. Department of Pediatric Surgery, 3. Department of Anesthesia, 4. Department of Surgery, 6. Department of Pediatrics, UTHSC; 2. Department of Healthcare Improvement, 5. Department of Infection Control, Memorial Hermann Hospital
Background - 44,000-98,000 preventable deaths a year - World Health Organization (WHO) Surgical Safety Checklist demonstrated to decrease mortality and morbidity world-wide - National Health Service has since advocated universal usage of the checklist N Engl J Med 2009;360:491
Background - Surgical Site Infections - Range between 2-5% for all surgical patients - Can add up to $30,000 additional hospital costs - Patient specific risk factors - Modifiable risk factors - Our infection rate - Between July 2007-December 2008, 7% - Between January 2009-September 2009, 4.8%
Goals - Decrease overall infection rates to less than 3% within 12 months - To develop a Surgical Site Infection (SSI) bundle, facilitated by an operative checklist, to decrease morbidity
Methods - SSI bundle creation - Preoperative chlorhexidine baths September 2008 - Routine antibiotic discontinuation within 48 hours April 2009 - Standardized prophylactic Vancomycin (targeted antibiotics) January 2010 - Antibiotics given 30-120 minutes before skin incision March 2010
Methods - SSI bundle creation - Preoperative chlorhexidine baths - Standardized prophylactic Vancomycin (targeted antibiotics) - Antibiotics given 30-120 minutes before skin incision - Routine antibiotic discontinuation within 48 hours
Methods - SSI bundle creation - Preoperative chlorhexidine baths - Routine antibiotic discontinuation within 48 hours - Standardized prophylactic Vancomycin (targeted antibiotics) - Antibiotics given 30-120 minutes before skin incision1 1 J Antimicrob Chemother 2006;58(3):645
Methods - SSI bundle creation - Preoperative chlorhexidine baths - Routine antibiotic discontinuation within 48 hours - Standardized prophylactic Vancomycin (targeted antibiotics) - Antibiotics given 30-120 minutes before skin incision1 1 J Antimicrob Chemother 2006;58(3):645
Methods - SSI bundle creation - Preoperative chlorhexidine baths - Routine antibiotic discontinuation within 48 hours - Standardized prophylactic Vancomycin (targeted antibiotics) - Antibiotics given 30-120 minutes before skin incision1 1 J Antimicrob Chemother 2006;58(3):645
Methods - SSI bundle creation - Preoperative chlorhexidine baths - Routine antibiotic discontinuation within 48 hours - Standardized prophylactic Vancomycin (targeted antibiotics) - Antibiotics given 30-120 minutes before skin incision1 1 J Antimicrob Chemother 2006;58(3):645
Methods - Risk stratification by Risk Adjusted Congenital Heart Surgery (RACHS) score - Low risk (RACHS 1, 2) - Medium risk (RACHS 3, 4) - High risk (RACHS 5, 6)
Methods - Retrospective and prospective data collection between August 2007 to August 2010 - Continuous ongoing data collection - Preoperative baths September 2008 - Routine antibiotic discontinuation within 48 hours April 2009 - Standardized antibiotic usage in January 2010 - Implementation of operative checklist began on March 24, 2010 - First cohort (August 2007-March 2010): 349 patients - Second cohort (March 2010-September 2010): 73 patients
Methods - Outcomes measured - Time between antibiotic administration and skin incision - SSI rates
Results - Random audits of preoperative baths: 100% compliance - Routine discontinuation of antibiotics on order form: 100% - Standardized usage of Vancomycin: >95% - Before the checklist, appropriate timing and dosing was only found in 21.4 - 40% of patients - After the checklist, actual compliance was 97.2% in all cases requiring cardiopulmonary bypass
Results Pre-intervention Antibiotic to Skin Incision Time Post-intervention Antibiotic to Skin Incision Time p value 26 34 Median = 24 minutes 60 29 Median = 59 minutes Low Risk (RACHS 1,2) 0.003 32 27 Median = 22.5 minutes 55 28 Median = 62.5 minutes Medium Risk (RACHS 3,4) 0.000 26 13 Median = 21 minutes 59 23 Median = 57 minutes High Risk (RACHS 5,6) 0.036 Surgical operations stratified as low risk, medium risk and high risk Pre- and post-bundle antibiotic dosage timing was analyzed by Student s t-test
Antibiotic Dosing Interval 90 80 70 60 50 Pre-intervention Post-intervention 40 30 20 10 0 -10 Low Risk Medium Risk High Risk
Conclusions - A SSI bundle appears to improve antibiotic delivery to biologically plausible times - This may help decrease the overall risk of developing a SSI - Quality process improvement requires a baseline commitment and environment
Conclusions - Checklists are flexible tools that may be effective in a variety of situations - Checklist utilization serve as reminders and may improve teamwork and intraoperative safety culture
Future Directions - Continue SSI surveillance - General pediatric surgery: process compliance - Pediatric neurosurgery & plastic surgery: near- misses (implants) - Laparoscopic surgery: OR efficiency - Further studies are needed to determine factors that help and hinder checklist utilization
Acknowledgements Jannette Gutierrez Jose Delgado Raul Guardiola Betsabe Quezada Sarah Eshelman Heather Dunne Bill Douglas Mohammed Rafique Kevin Lally Kathy Masters Eric Thomas This work was supported in part by a training fellowship from the AHRQ Training Program of the W.M. Keck Center for Interdisciplinary Bioscience Training of the Gulf Coast Consortia (AHRQ Grant No. T32 HS017586)

![Guardians of Collection Enhancing Your Trading Card Experience with the Explorer Sleeve Bundle [4-pack]](/thumb/3698/guardians-of-collection-enhancing-your-trading-card-experience-with-the-explorer-sleeve-bundle-4-pack.jpg)