Airway Management in Neurological Patients: ENLS Version 5.0
Explore the essentials of airway, ventilation, and sedation in neurological patients through the ENLS Version 5.0 content. Understand the challenges and goals of managing airways in critical situations such as trauma or respiratory distress. Learn about common indications for intubation and the importance of optimizing cerebral physiology during patient care.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
ENLS Version 5.0 Airway, Ventilation, And Sedation Content: Christopher P. Robinson, DO, MS; Thomas L. Delmas, MD; Iqbal O Meara, MD Slides: Christopher P. Robinson D.O.,M.S. Presented by: Diane McLaughlin, APP
Editors Note: Global Considerations The intent of the editors, authors, and reviewers of this ENLS topic was not to address all the variations in international practice for the different diseases. We have discussed major practice variances (e.g., the availability of diagnostic testing, or the type of medications used) and encourage learners to use the ENLS algorithms as a framework on which any relevant local practice guidelines can be incorporated.
Case A 70-year-old man was seen by EMS at the scene after a motor vehicle collision and head trauma. He is obese, edentulous, and has a large facial laceration. EMS decides to perform bag-mask ventilation and intubate the patient.
What will be the reason for difficult bag- mask ventilation in this patient? A. The age of 70 years old B. The obesity of this patient C. The lack of teeth in this patient D. The large laceration on the patient s face E. All of the above
What will be the reason for difficult bag- mask ventilation in this patient? A. The age of 70 years old B. The obesity of this patient C. The lack of teeth in this patient D. The large laceration on the patient s face E. All of the above
Goals of Airway Management in Neurological Patients Maintain adequate oxygenation and ventilation Optimize cerebral physiology Preserve cerebral perfusion Prevent aspiration
Four Commonly Accepted Indications to Intubate: Failure to oxygenate Evidence of respiratory distress or cyanosis Low oxygen saturation, ABG Failure to ventilate Observation of respiratory effort exerted Capnometry, ABG Failure to protect the airway Bulbar dysfunction, airway anatomy Airway secretions, strength of cough reflex Ability to swallow after suctioning The presence of a gag reflex is an inadequate method of assessing airway protection. Anticipated neurological or cardiopulmonary decline
The MOANS Mnemonic Predicts difficulty of bag mask ventilation M = Mask seal, may be compromised by abnormal facies, facial hair and body fluids O = Obesity/obstruction A = Age > 55 N = No teeth S = Stiff lungs
Airway Assessment LEMON mnemonic predicts difficult intubation: L = Look externally E = Evaluate with 3-2-2 rule M = Mallampati score ? O = Obstruction/obesity N = Neck mobility
The MACOCHA Score Predicts difficulty of tracheal intubation in ICU patients M = Mallampati Score III or IV points) A = Apnea Syndrome (obstructive) C = Cervical spine limitation point) O = Opening of mouth < 3cm point) C = Coma (1 point) H = Hypoxia (<80%) (1 point) A = Anesthesiologist non-trained point) (5 (2 points) (1 (1 Know when to call for HELP!!! (1
Question What are the medications that you can use as pre-medication to avoid increases in intra cranial pressure (ICP) during intubation? A. Lidocaine and midazolam B. Fentanyl and midazolam C. Lidocaine and fentanyl D. Etomidate and fentanyl E. Etomidate and propofol
Question What are the medications that you can use as pre-medication to avoid increase in intra cranial pressure (ICP) during intubation? A. Lidocaine and midazolam B. Fentanyl and midazolam C. Lidocaine and fentanyl D. Etomidate and fentanyl E. Etomidate and propofol Lidocaine: Administer IV lidocaine 1.5 mg/kg 60-90 sec prior to intubation Fentanyl: Administer 2-3 mcg/kg slowly over 30-90 sec
Algorithm for Intubation with Elevated ICP
Intubating the Patient with Intracranial Pathology Goals of parameters: ICP below 22 mmHg Systolic blood pressure (SBP) >100-110 mmHg or mean arterial pressure (MAP) > 65 mmHg Cerebral perfusion pressure (CPP=MAP-ICP) at a minimum of 60 mmHg during intubation.
Intubating the Patient with Brain Ischemia Avoid hypotension to preserve ischemic penumbra Avoid hyperventilation due to cerebral vasoconstriction Use IV fluid bolus or (if needed) use vasopressor Induction agent: ketamine or etomidate Consider conscious sedation for endovascular therapy rather than intubation
Intubating the Patient with an Unsecured Vascular Malformation or Expanding Hematoma Avoid severe hypertension to prevent rebleeding Consider fentanyl prior to intubation Try to avoid ketamine due to sympathetic effects
Intubating the Patient with Neuromuscular Weakness Arterial blood gas measurement Serial respiratory function assessments Negative inspiratory force (NIF) - < - 30 Forced vital capacity (FVC) - > 18 cc/kg Maximum expiratory force (MEF) - > + 40 Assessment of bulbar function, neck strength, and cough
Intubating the Patient with Cervical Spine Injury Avoid: Bag mask ventilation Cricoid pressure Direct laryngoscopy Consider fiberoptic intubation if stable oxygenation and ICP Perform jaw-thrust rather than head-tilt/chin-lift Video laryngoscopy is preferred Manual in-line stabilization MILS and open the anterior part of collar Head-tilt/chin-lift
Medications Commonly Used in Rapid Sequence Intubation (RSI): Pre-induction Agents Onset of action Duration of effect Drug Dose Indications Precautions 2-3 /kg IV over 1-2 min Within 2-3 min 30-60 min Pre-induction, blunts ICP rise Respiratory depression Fentanyl Hypotension, rare chest wall rigidity 1.5 mg/kg IV 2-3 min before intubation 45-90 sec 10-20 min Pre-induction, blunts ICP rise Avoid if allergic or high-grade heart block if no pacemaker Lidocaine 1-2 mg/kg IV 2-10 min 10-30 min Pre-induction, blunts ICP rise Bradycardia, hypotension, increased airway reactivity Esmolol
Medications Commonly Used in RSI: Induction Agents Onset of action 30-60 sec Duration of effect 3-5 min Drug Dose Indications Precautions 0.3 mg/kg IV Induction, sedation; good in hypotension. Decreases CBF, ICP, preserves CPP. Induction, sedation, reduces ICP and airway resistance, anticonvulsive effects Decreases seizure threshold, decreases cortisol synthesis; avoid in sepsis Hypotension, myocardial depression Etomidate 1.5 mg/kg IV 9-50 sec 3-10 min Propofol 1.5-2 mg/kg IV 1-2 min 5-15 min Induction, analgesia, sedation, amnesia, bronchodilatory effects; good in hypotension. Catecholamine surge, possible increase in ICP, Ketamine re-emergence phenomenon if not pretreated with benzos
Medications Commonly Used in RSI Onset of action Duration of effect Drug Dose Indications Precautions 0.5-1.1 mg/kg IV 30-60 sec 5-15 min Preferred paralytic unless contraindicated Avoid in hyperkalemia, myopathy, neuropathy/denervation, history of malignant hyperthermia. Succinylcholine 0.6-1.2 mg/kg 45-60 sec 45-70 min Paralysis when succinylcholine contraindicated Caution in difficult mask ventilation and difficult intubation. Rocuronium 0.2 mg/kg Within 3 min 35 min Least preferred paralytic for RSI This dose speeds onset during RSI Vecuronium Caution in difficult mask ventilation and difficult intubation.
Laryngoscopy and Intubation Up to three attempts at laryngoscopy and intubation are permissible, as long the SpO2 remains >94%. With each attempt, change the operator or the technique. Video-laryngoscopy consistently results in higher rates of glottis visualization.
The Cormack-Lehane System Grading of the Direct Laryngoscopic View of the Glottis
The Failed Airway Cannot intubate, cannot ventilate : BMV is ineffective Single, best attempt intubation is unsuccessful Cannot intubate, CAN ventilate : Three attempts at intubation unsuccessful BMV remains effective
Post-intubation Management Post-intubation Checklist Secure endotracheal tube Confirm tube position, order chest x-ray Set cuff pressure to 20-30 cmH2O Pulse oximetry and quantitative waveform capnography Arterial blood gas measurement Deep sedation while neuromuscular blockade in effect Aim for: SpO2 >94% pH 7.35 7.45 PaCO2to 35 45 mmHg Counsel next of kin on change in patient status
Sedation in Neuro ICU Pros: Reduces ICP and cerebral oxygen consumption, facilitates tolerance of the mechanical ventilation, reduces sympathetic hyperactivity Cons: Makes accurate neurological examination difficult or impossible
Choice of Analgesia for Sedation Analgesia: Short-acting opioid infusion Fentanyl or hydromorphone Sedatives: Dexmedetomidine or propofol (benzodiazepines are less favorable) Use analgosedation as a first-line measure in the intubated patient.
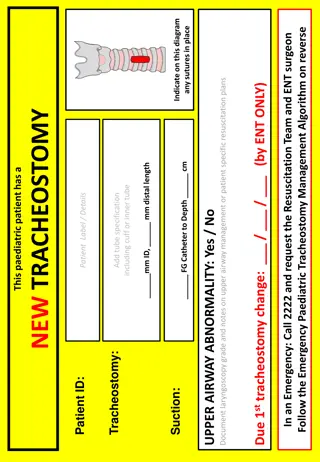
Pediatric Considerations Criteria for endotracheal intubation of children with TBI and other forms of acute brain injury: Hypoxemia unresponsive to supplemental oxygen Apnea, hypercapnia (PaCO2>45mmHg or 6 kPa) GCS score 8 or rapid decrease in GCS Anisocoria >1 mm Cervical spinal injury compromising ventilation Abnormal airway reflexes Clinical signs of herniation or impending herniation
Anatomical Differences Between the Pediatric and Adult Airway Children have a proportionally larger tongue Upper airway tissues are more compliant Epiglottis is longer, narrower, and floppier Tracheal distance is shorter Children have a prominent occiput The narrowest portion of the child s upper airway is subglottic, at the level of the cricoid ring.
Hand Off Communication Mental status and neurological examination immediately pre-intubation Intracerebral hemorrhage (ICH) score, if appropriate Vitals, hemodynamics, and gas exchange pre- and post-intubation Relevant drugs used around intubation Technique of intubation, confirmation of tube position Ease of bag-mask ventilation, intubation, and tube passage Cormack-Lehane grade, if appropriate Ventilator settings, ventilation and ETCO2 targets Analgesia and sedation strategy