ENLS Version 5.0 Pharmacotherapy Pearls and Hyperosmolar Therapy Overview
This content delves into the pharmacotherapy pearls of ENLS Version 5.0, highlighting medication characteristics, adverse effects, and optimal pharmacotherapy strategies for acute neurological injuries. It specifically focuses on Hyperosmolar Therapy, comparing options like Mannitol and Sodium Chloride 23.4%. A case study of a 25-year-old male post-TBI with elevated ICP is presented to illustrate treatment decisions.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
ENLS Version 5.0 Pharmacotherapy Pearls Content: Eljim Tesoro, PharmD, BCCCP, FNCS, FCCM; Mehrnaz Pajoumand, PharmD Slides: Eljim Tesoro, PharmD, BCCCP, FNCS, FCCM
Editors Note: Global Considerations The intent of the editors, authors, and reviewers of this ENLS topic was not to address all the variations in international practice for the different diseases. We have discussed major practice variances (e.g., the availability of diagnostic testing, or the type of medications used) and encourage learners to use the ENLS algorithms as a framework on which any relevant local practice guidelines can be incorporated.
Pharmacotherapy Learning Objectives Describe the pharmacology, pharmacokinetics, and pharmacodynamic characteristics of medication used in ENLS. Identify potential adverse drug effects and drug interactions for medications used in ENLS. Determine the optimal pharmacotherapy strategy for a patient with acute neurological injury.
ENLS Medication Review Anticoagulant reversal and hemostatic agents Hyperosmolar therapy Antiseizure medications Antithrombotic agents Neuromuscular blocking agents Anti-shivering agents Sedation and Analgesia Antihypertensive agents Vasopressor and Inotropes Antimicrobials
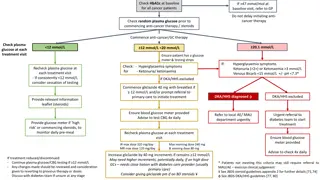
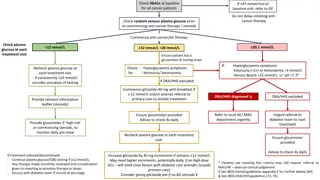
Hyperosmolar Therapy Comparison Mannitol 20% Sodium Chloride 23.4% Equi-osmolar dose 1 g/kg 30 mL Infusion IVPB over 15-30min IVP/IVPB over 10-20 min Line Monitoring Central preferred Monitor trough osmolar gap (Goal < 20 mOsm/Kg) Central Monitor serum sodium every 4-6 hours (trough), avoid prolonged hypernatremia > 160 mEq/L
Hyperosmolar Therapy Case 25-year-old male post TBI, sustained ICP 25-30 mmHg x 5 minutes Has received 3 doses of 23.4% NaCl and 2 doses of mannitol in last 24 hours Lab findings: Na: 154 mEq/L K: 4.5 mEq/L Cl: 119 mEq/L HCO3: 18 mEq/L BUN: 29 mg/dL (10.4 mmol/L) Cr: 1.1 mg/dL (97.3 umol/L) Gluc: 188 mg/dL (10.4 mmol/L) Osm: 341 mOsm/L What is the best osmotic therapy for this patient for ICP control? A. 30 ml of 23.4% NaCl B. Mannitol at 1 gm/kg
Hyperosmolar Therapy Case 25-year-old male post TBI, sustained ICP 25-30 mmHg x 5 minutes Has received 3 doses of 23.4% NaCl and 2 doses of mannitol in last 24 hours Lab findings: Na: 154 mEq/L K: 4.5 mEq/L Cl: 119 mEq/L HCO3: 18 mEq/L BUN: 29 mg/dL (10.4 mmol/L) Cr: 1.1 mg/dL (97.3 umol/L) Gluc: 188 mg/dL (10.4 mmol/L) Osm: 341 mOsm/L What is the best osmotic therapy for this patient for ICP control? A. 30 ml of 23.4% NaCl B. Mannitol at 1gm/kg
Mannitol Pearls Requires in-line filter (precipitates-crystal formation) May require warming to dissolve crystals before administration May be given via peripheral access Duration of effect 90 min 6 hr Monitor trough osmotic gap Goal < 15-20 mOsm/L Osmolar gap = Measured osmolality Calculated osmolality Osmolar gap = Measured osmolality [(2 x Na) + (BUN/2.8) + (glucose/18)]
Hypertonic Saline Pearls Central access is required for: 23.4% NaCl bolus >2% NaCl if using continuous infusion Duration of effect: 90 min 4 hour Monitor serum sodium every 4-6 hours (trough) Avoid prolonged hypernatremia > 160 mEq/L
Adverse Reactions Mannitol Rebound ICP elevation (with high, repeated dosing) Hypertonic Saline Pulmonary edema Heart failure Acute kidney injury Coagulopathy Hypernatremia Metabolic acidosis Thrombophlebitis Osmotic demyelination syndrome with rapid correction Acute kidney injury Dehydration Hypotension Electrolyte imbalances
Antiseizure Meds: Emergent (1st line) Drug Name Diazepam Dose Rate Adverse Effects Hypotension, respiratory depression Clinical Pearls Rapid redistribution rate; can be given rectally; contains propylene glycol 0.15 mg/kg IV (up to 10 mg per dose); may repeat in 5 minutes 5 mg/min (IVP) 0.1 mg/kg IV (up to 4 mg per dose); repeat in 5-10 minutes 2 mg/min (IVP) Hypotension, respiratory depression May be longer-acting for seizure cessation than diazepam, contains propylene glycol Lorazepam 0.2 mg/kg IM up to 10 mg per dose Sedation, hypotension, respiratory depression Can also be given buccally, intranasally Midazolam
Antiseizure Meds: Urgent (2nd line) Target Serum Concentrations 10 20 mcg /mL Free: 1-2 mcg/ml Adverse Effects Arrhythmias, hypotension, bradycardia Drug Name Dose Rate Clinical Pearls Load: 20 mg/kg ADULT/PEDS Maintenance dose: 4-6 mg/kg/day divided in 2-3 doses Load: 20 mg PE/kg ADULT/PEDS Maintenance dose: 4- 7 mg/kg/day divided into 2-3 doses Up to 50 mg/min Hypotension (contains propylene glycol), especially in older adults; STRONG CYP inducer with many potential drug interactions Phenytoin Up to 150 mg PE/min Same as phenytoin above Arrhythmias, hypotension, bradycardia Prodrug converts to phenytoin in 7-15 min after infusion; less thrombophlebitis than phenytoin; same drug interactions and monitoring parameters Long-acting; contains propylene glycol; STRONG CYP enzyme inducer with many potential drug interactions Fosphenytoin Phenobarbital 20 mg/kg 50 100 mg/min 15 40 mcg/mL Hypotension, sedation, respiratory depression Maintenance dose: 1-3 mg/kg/day divided into 1-3 doses *Pediatric dosing: 1-5mg/kg/day
Antiseizure Meds: Urgent (2nd line) Target Serum Concentrations 50 150 mcg/mL Drug Name Dose Rate Adverse Effects Clinical Pearls Load: 40 mg/kg IV Maintenance dose: 10-15 mg/kg/day divided into 2-4 doses *Pediatric dosing: 20-40 mg/kg/day divided q6h 3 6 mg/kg per minute Fewer CV side effects than phenytoin; CYP enzyme inhibitor with many potential drug interactions; Meropenem will significantly reduce VPA levels therefore caution should be used when combination prescribed Reduce dose in renal impairment; few drug interactions Valproate sodium Hepatotoxicity, thrombocytopenia, hyperammonemic encephalopathy Load: 60 mg/kg IV (max: 4500 mg) Maintenance dose: 1000-3000 mg/day in 2 divided doses *Pediatric dosing: 60 mg/kg/day divided q12h 200-400 mg IV Every 12 hrs *Pediatric dosing: 10 mg/kg IV load, then 5-10 mg/kg/day divided q12h Over 15 min 12-46 mcg/ml (not typically monitored) Levetiracetam Dizziness, behavior disturbances (irritability, agitation, aggression) Over 15 min 2.8-18 mcg/ml (not typically monitored) Consider monitor EKG in patients with underlying cardiac disease; Reduce dose in renal impairment; few drug interactions Lacosamide PR prolongation, hypotension (rare)
Antiseizure Medication Case A patient diagnosed with status epilepticus is receiving fosphenytoin, valproate, pentobarbital, and levetiracetam. What drug is least likely to cause drug interactions? A. Fosphenytoin B. Valproate C. Pentobarbital D. Levetiracetam
Antiseizure Medication Case A patient diagnosed with status epilepticus is receiving fosphenytoin, valproate, pentobarbital, and levetiracetam. What drug is least likely to cause any drug interactions? A. Fosphenytoin B. Valproate C. Pentobarbital D. Levetiracetam
Antiseizure Medication Pearls Antiseizure agents (urgent therapy), administered after benzodiazepines (emergent therapy) for treatment of status epilepticus, should be given intravenously over a short period of time. The appropriate agent should be chosen based on the medication s adverse drug reaction profile, etiology of seizure, patient organ function, pre-existing antiseizure drugs, and the patient hemodynamic stability.
Alteplase Pearls Swirl, DO NOT SHAKE, during reconstitution. Prepare the appropriate dose of alteplase. Remove excess drug from the bottle before infusion to prevent: Inadvertent administration of total doses of >90 mg Increased risk of intracerebral bleeding DOAC (Direct Oral AntiCoagulants) administration within the last 48 hours or any abnormal coagulation tests for these specific agents are a contraindication for receiving alteplase Determine time of last dose if possible and renal function Angioedema can occur during or after alteplase administration and has been associated with previous angiotensin- converting enzyme (ACE) inhibitor use.
Antithrombotic Considerations Clopidogrel Approximately 30-60% of the population have genetic polymorphisms and do not respond to clopidogrel, a prodrug. DOACs Significantly lower intracranial bleeding risk than warfarin, but are associated with a risk of gastrointestinal bleeding ASA If the patient requires ASA for AIS and is on a DOAC, there is an increased risk of bleeding, and the risk-to-benefit ratio must be considered until the DOAC has had time to be cleared from the body (i.e., approximately 3-5 half-lives)
General Management Strategies Treatment of major hemorrhages, and identification of the cause and source of bleeding Maintenance of hemodynamic and respiratory stability Maintenance of normal body temperature, blood pH, and electrolyte balance to facilitate coagulation Application of packing or dressing if applicable; local hemostatic measures or surgical intervention to control bleeding Identification of the anticoagulant and administering an appropriate reversal agent
Acute Reversal: Life-threatening Bleeding Hold anticoagulant (if receiving one) If oral anticoagulant given within 2 hours, consider activated charcoal 50 g Give vitamin K 10mg IV (for warfarin) Do not administer SQ Consider administration of PCC or FFP Recheck INR 30 minutes after PCC or FFP (if appropriate based on anticoagulant)
Acute Reversal: Life-threatening Bleeding Warfarin For rapid reversal, guidelines suggest use of PCC agents over FFP Dabigatran Idarucizumab binds dabigatran to neutralize its anticoagulant effects Apixaban/Rivaroxaban Andexanet alfa competitively binds apixaban and rivaroxaban and eliminates the ability of these agents to inhibit endogenous Factor-Xa
Comparison of PCC Products Anticoagulant Proteins Protein S Clotting Factors FVII Protein C FII FIX FX AT Heparin Product 3-Factor PCCs 24-38 IU/ml NA NA 24-38 IU/ml <5 IU/ml 24-38 IU/ml 100 U NA <0.15 IU /IU of FIX NA Bebulin NA NA NMT 150 U/100 FIX units NMT 35 U/100 FIX units 100 U/100 FIX units NA Profilnine 4-Factor PCCs 22-60 IU/ml 15-45 IU/ml 12-38 IU/ml 12-32 IU/ml 20-48 IU/ml 10-25 IU/ml 30-31 IU/ml 25 IU/ml 0.2-1.5 IU/ml NA 0.4-2 IU/ml Beriplex/ Kcentra Octaplex 13-31 IU/ml 14-38 IU/ml 9-24 IU/ml 18-30 IU/ml 5-12.5 IU/ml Activated PCC 1.1 U/U NA 1.3 U/U 0.9 U/U 1.4 U/U 1.1 U/U NA None FEIBA
Acute Antithrombotic Reversal Case An agent that will achieve the fastest reversal of laboratory parameters in a patient receiving rivaroxaban? A. Vitamin K B. Andexanet alfa C. FFP
Acute Antithrombotic Reversal Case An agent that will achieve the fastest reversal of laboratory parameters in a patient receiving rivaroxaban? A. Vitamin K B. Andexanet alfa C. FFP
Acute Antithrombotic Reversal Case What factor is used to determine the dose of PCC? A. II B. VII C. IX D. X
Acute Antithrombotic Reversal Case What factor is used to determine the dose of PCC? A. II B. VII C. IX D. X
Coagulation Reversal Pearls When reversing an anticoagulant, the risk of continued bleeding relative to the risk of thrombosis is of the utmost importance and should be determined in each case. Timing of the last dose of anticoagulant administered and elimination half-life is necessary to determine if reversal is warranted. In the case of life-threatening bleeding, reversal should be considered if the anticoagulant was taken within 3-5 half-lives and may be necessary out to 2-3 days from the last dose with anticoagulants with long half-lives and/or in patients with renal dysfunction. For rapid reversal of warfarin, guidelines suggest use of prothrombin complex concentrate (PCC) agents over fresh frozen plasma (FFP) in combination with Vitamin K.
Management of Shivering during Temperature Control The Bedside Shivering Assessment Scale Score Description No shivering 0 Shivering localized to the neck and/or thorax only 1 Shivering involves gross movement of the upper extremities (in addition to neck and thorax) 2 Shivering involves gross movements of the trunk, upper and lower extremities 3
TTM Case 45-year-old man with TBI and elevated ICP Temp 38.9 C Goal: Temp 36.5-37.5 C Topical cooling initiated BSAS 3 What medications may be useful in controlling this patient s shivering?
Shiver Management Pearls Shivering is crucial to identify and treat in patients treated with targeted temperature management because it: Increases the metabolic rate Counteracts cooling induction Consumes energy Contributes to increased intracranial pressure Increases brain oxygen consumption Can be deleterious in acute brain injury
Neuromuscular Blocking Agent Medication Administration pearls Cannot be reversed May cause slight increases in intracranial pressure (ICP; inconsistent data) Severe hyperkalemia may occur in patients with burns, severe muscle trauma, neuromuscular diseases, strokes, spinal cord injury, multiple sclerosis, and prolonged immobilization Contraindicated in patients with Malignant hyperthermia Hyperkalemia (serum potassium > 5.0 mEq/L) Succinylcholine Pancuronium Conditions that slow circulation may delay onset No significant cardiovascular effects No effect on ICP Vecuronium Longer half-life in elderly Elimination via enzymatic breakdown and does not rely on renal or liver function for clearance Cisatracurium Rocuronium Prolonged duration in renal failure
Neuromuscular Blocking Agent Pearls When administering neuromuscular blocking agents, it is vital that adequate sedation and analgesia be administered prior to neuromuscular blocking agent. Monitoring the train-of-four (TOF) with a peripheral nerve stimulator (PNS) in conjunction with the clinical assessment (vital signs, synchrony with the mechanical ventilator) should always be used to evaluate the extent of paralysis. Patients should not have noxious stimuli or oculovestibular response performed as they will be unable to elicit a motor response due to muscle paralysis.
Summary Pharmacologic management in patients is very challenging, especially while attempting to minimize secondary brain injury. Medication choices and doses must be individualized for each patient based upon the following: Medical history Comorbidities Pharmacokinetic and pharmacodynamic changes due to age, critical illness, and neurocritical care interventions; potential adverse drug effects, and drug interactions Appropriate pharmacotherapy is essential during application of ENLS to optimize care of patients with neurological emergencies.