Understanding Male Reproductive Anatomy and Function
Explore the intricate male reproductive system from meiosis to accessory glands, learning about the purpose and location of processes like meiosis, sperm production in the testes, and the functions of structures such as the epididymis, vas deferens, urethra, and accessory glands in semen production and ejaculation. Delve into details like the role of different glands in semen production, the pathway of sperm through the male reproductive tract, and the importance of meiosis in generating sperm with a human chromosome number of 46.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
I. Need for Meiosis A. Human chromosome number = 46 B. Mitosis C. Meiosis 1. purpose 2. location 3. difference in male and female meiosis
II. Male parts A. Testes 1. produces sperm in seminiferous tubule 2. approximately 700 feet long 3. site of male meiosis 4. interstitial cells also located in testes 5. producers of testosterone
B. Epididymis 1. location 2. 20 feet 3. twenty days to pass through 4. undergo maturation 5. storage organ 6. contracts upon ejaculation sending sperm on to next part of journey
C. Vas deferens or ductus deferens 1. Travels from epididymis to urethra 2. Travels through the inguinal canal with the spermatic cord-blood vessels and nerves 3. Expands into the ampulla 4. Then enters ejaculatory duct
5. Vasectomy a. Part of vas lies in scrotum b. Local c. Small incision d. Cuts and ligates e. Sterile but not impotent
D. Urethra 1. Prostatic urethra 2. Membranous urethra 3. Spongy or penile urethra 4. Carries both sperm and urine 5. Never at same time
E. Accessory glands producing semen 1. seminal vesicles a. Produce 60% of semen b. Thick yellowish secretion c. Rich in sugar, vitamin C, and prostaglandins d. Nourish and activate sperm e. Joins vas deferens on either side to form ejaculatory duct
2. Prostate gland a. Doughnut shaped b. Size of peach pit c. Milky alkaline fluid that activates sperm d. Approximately 40% of semen e. Anterior to rectum is able to be palpated by digital exam f. Hypertrophy
3. Bulbourethral glands a. Also called Cowper s glands b. Base of prostate-size of peas c. First to empty with ejaculation d. Cleanse and neutralizes penile urethra e. Also minor lubricant for coitus
4. Seminal fluid a. Mature sperm are streamlined missiles b. Need nutrient source-fructose from seminal vesicle c. Need buffer from prostate d. Prostaglandins cause smooth muscle to contract e. Fibrinogen and profibrinolysin f. Inhibitors of female immune system g. Dilutes sperm
F. Male parts 1. scrotum a. Air conditioner b. Rather exposed c. Cooler temperatures d. Best produced 93 degrees e. Bikers problems
2. Penis a. b. c. d. e. f. Corpora cavernosa Corpus spongiosum Urethra Glans penis Prepuce Mechanics of an erection
G. Spermatogenesis 1. occurs in seminiferous tubule 2. spermatozoa a. acrosome b. head c. midpiece d. flagella
3. Defective sperm and numbers a. Defective morphology b. Low sperm count c. 10 million/ml d. Varicocoel e. Cryptochordism f. Retrograde ejaculation
H. Testosterone production 1. Interstitial cells of Leydig 2. In response to LH production by the anterior pituitary 3. Occurs at about the age of 12 4. Maturation of male reproductive parts 5. Stimulates production of sperm along with FSH 6. Produces male secondary sexual traits such as hair growth patterns, deepening of the voice, skeletal muscle development
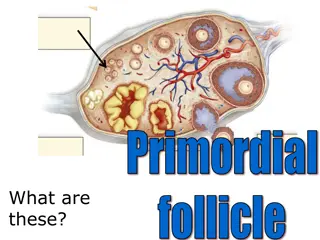
III. Female parts A. Ovary 1. ovarian follicles 2. oocyte and follicular cells 3. antrum with follicular fluid 4. Graafian follicle 5. ovulation 6. corupus luteum
B. Duct system 1. Fallopian tubes 2. Fimbriae 3. Uterus a. Body, fundus, cervix b. Endometrium, myometrium 4. Vagina-birth canal
C. Female external genitalia 1. 2. 3. 4. 5. 6. Mons pubis Labia majora Labia minora Vestibule Clitoris Perineum
IV. Female reproductive functions A. Oogenesis 1. Oogonium 2. Primary oocyte 3. Meiosis I 4. ovulation 5. Meiosis II
B. Hormonal interactions 1. Pituitary hormones 2. Ovarian events 3. Ovarian hormone fluctuations 4. Uterine lining evernts
And then there was baby http://www.evtv1.com/player.aspx?itemnum= 735
Fetal development http://www.youtube.com/watch?v=RS1ti23SU Sw