Assisted Reproductive Technologies: Gamete Intra-fallopian Transfer (GIFT)
Assisted Reproductive Technologies (ART), such as Gamete Intra-fallopian Transfer (GIFT), offer a method for couples struggling with infertility. GIFT involves placing fertilized eggs in the fallopian tubes, unlike In Vitro Fertilization (IVF). The procedure requires healthy fallopian tubes and offers an alternative for couples with ethical concerns about IVF. Learn about the process, eligibility criteria, and differences between GIFT and IVF.
- Assisted Reproductive Technologies
- Gamete Intra-fallopian Transfer
- GIFT procedure
- Infertility treatment
- ART
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
ASSISSTED REPRODUCTIVE TECHNOLOGIES Kamal Kumar Gupta
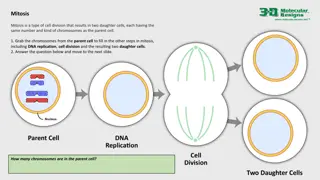
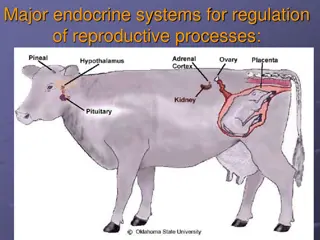
Gamete Intra-fallopian transfer GIFT is an assisted reproductive procedure which involves removing a woman s eggs, mixing them with sperm, and immediately placing them into a fallopian tube In GIFT fertilization takes place inside the fallopian tube rather than in a laboratory unlike in vitro fertilization (IVF) and zygote intrafallopian transfer (ZIFT)
How is GIFT performed? Healthy tubes are necessary for GIFT to work Patients must first have an x-ray to determine the presence of at least one healthy fallopian tube. The doctor use a laparoscope to ensure that there is not any scar tissue on the outside of the fallopian tube Using a laparoscope, eggs are then retrieved from the ovaries The male provides a sperm sample on the same day that the eggs are retrieved
How is GIFT performed? The eggs are then mixed with the sperm in a catheter The egg and sperm mixture is inserted into the fallopian tubes with a catheter The woman is then provided with medication to build up the uterine lining to support implantation of a fertilized egg
Who can be treated with GIFT? Couples with unexplainable infertility Women who have at least one healthy fallopian tube Couples in which the husband has a low sperm count or other problems with his sperm Couples who have not had success with IVF Couples who have a religious or moral reluctance to use IVF
Differences between GIFT and in vitro fertilization (IVF)? With IVF, the eggs are fertilized in a laboratory rather than in the fallopian tubes as with GIFT IVF can be used with couples in which the female does not have fallopian tubes or has blocked fallopian tubes IVF allows for fertilization confirmation and assessment of embryo quality GIFT does not involve fertilization outside of the body, so couples do not have to deal with the ethical concerns with choosing which embryos to transfer
Advantages and Disadvantages The GIFT does not require the patient to be hospitalized. After the procedure, patients typically stay in recovery for about eight hours Doctors cannot visibly confirm fertilization or determine embryo quality with GIFT GIFT cannot be used in patients who have damaged or blocked fallopian tubes
Vaginal GIFT A major disadvantage with conventional GIFT is that a surgical procedure - laparoscopy - is needed to transfer the eggs and sperm into the fallopian tube Dr. Jansen and Anderson from Sydney, described vaginal GIFT, in which the gametes can be transferred into the fallopian tubes through the vagina and cervix under ultrasound guidance
Vaginal GIFT This requires a special set of catheters which allow the doctor to enter the uterine ends of the fallopian tubes through the cervix Once the catheters have been accurately positioned - and ultrasound can help in this - the gametes are injected into the tubes. Since this does not involve surgery, it is less expense, no hospitalization, no scar and no anesthesia is required However, the technique does require much more technical expertise and is still being investigated more thoroughly. Also, the pregnancy rates with the method are less than with conventional laparoscopic GIFT.
Zygote Intrafallopian transfer Transfer of zygote in the fallopian tube Difference between IVF-ET and ZIFT Difference between GIFT and ZIFT
Similarities and Differences between ZIFT and In Vitro Fertilization (IVF) ZIFT and IVF both tend to be favorable treatments for women who have more severe infertility issues such as damaged fallopian tubes ZIFT and IVF both involve embryo culture ZIFT transfers the fertilized embryo into the fallopian tube whereas the IVF and embryo transfer procedures result in the fertilized embryo being placed into the uterus. The ZIFT procedure differs from IVF in that the transfer of embryos into the tube requires an extra surgical procedure called laparoscopy
PROST: Pronuclear stage Tubal Transfer Transfer of fertilized egg at pronuclear stage in the fallopian tube Few hour before ZIFT After 14 hr of penetration of the sperm
TEST: Tubal Embryo Stage Transfer TET: Tubal Embryo Transfer A multi cell (2, 4 or 8) stage embryo is transferred in fallopian tube after IVF
ICSI: Intracytoplasmic Sperm Injection If infertility is due to impaired sperm motility or failure of spermatids to differentiate into sperms The oocyte can be fertilized by injecting the sperm or spermatid directly in the its cytoplasm The Zygote is developed to 8 or 16 cell stage and introduced in to uterus
ICSI Patients with very low sperm numbers Patients with very low sperm motility Patients with very high numbers of abnormal sperm When the sperm have been surgically collected i.e. taken directly from the epididymis (MESA) or testicles (TESA) When there is a high level of antibodies in the semen When very few eggs conventional IVF or very few eggs have been collected at egg pick-up have fertilised following
PESA PESA or Percutaneous Epididymal Sperm Aspiration (PESA), does not require a surgical incision. A small needle is passed directly into the head of the epididymis through the scrotal skin and fluid is aspirated. The embryologist retrieves the sperm cells from the fluid and prepares them for ICSI.
MESA Microsurgical (MESA) is used in conditions like obstructive azoospermia, involves epididymis under the operating microscope and incision of a single tubule. Fluid spills from the Epididymal tubule and pools. This pooled fluid is then aspirated. Because the epididymis is richly vascularized, this technique invariably leads to contamination by blood cells that may affect sperm fertilizing capacity in vitro Epididymal Sperm Aspiration dissection of the
TESE and TESA TESE or testicular sperm extraction is a surgical biopsy of the testis whereas TESA or testicular sperm aspiration is performed by inserting a needle in the testis and aspirating fluid and tissue with negative pressure. The aspirated tissue is then processed in the embryology laboratory and the sperm cells extracted are used for ICSI.
How is it done? All patients receive hormonal stimulation as for conventional IVF treatment, the differences between IVF and ICSI occur in the laboratory alone. After its collection the egg is examined to ensure it is suitable for ICSI, and a single sperm is injected into the egg. The eggs are then placed in culture and examined the following day to see whether they have fertilised normally A semen sample will need to be provided on the morning of the egg collection by the partner. However, if the sperm is to be collected surgically, this will have been performed earlier and frozen, or collected on the days prior to, or on the day, of oocyte collection.
Potential risks One genetic abnormality that is known to be associated with male infertility is where there are Y- chromosome defects. If these genes are defective or parts of them are missing production will be reduced or non-existent. If ICSI is used to overcome the very low sperm counts and a male child is born he will inherit this problem. (deletions), sperm Increased pregnancies collected sperm when it is used to overcome low sperm numbers. miscarriage resulting rates from are ISCI also using seen surgically in
APPLICATIONS Intracytoplasmic sperm injection (ICSI) has enabled many men with AIDS, paralysis, very low sperm counts, or abnormal sperm to become fathers, without increasing the birth defect rate But potential problems are emerging, based on the fact that ICSI bypasses natural sperm selection barriers. ICSI is now commonly used on men who make very few or no sperm by using a needle to extract precursor cells, called spermatids, from the testes. That is, the infertility does not arise until the sperm mature. About 10 percent of infertile men have microdeletions in the Y chromosome and when they use ICSI, they pass on the infertility to their sons.
MIF: Microinjection Fallopian Transfer The embryo so obtained by microinjection method is transferred into fallopian tube