EASL Clinical Practice Guidelines for Drug-Induced Liver Injury Management
These slides provide an in-depth overview of the EASL clinical practice guidelines on managing drug-induced liver injury. The guidelines cover epidemiology, key recommendations, future prospects, new biomarkers, unresolved issues, and unmet needs. Recommendations are based on evidence levels from the Oxford Centre for Evidence-based Medicine, with a focus on therapy, prevention, and harm assessment. Users are encouraged to reference the full publication for detailed information and consult with healthcare professionals when making patient management decisions.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Clinical Practice Guidelines Drug-induced liver injury
About these slides These slides give a comprehensive overview of the EASL clinical practice guidelines on the management of drug-induced liver injury The guidelines were first presented at the International Liver Congress 2018 and are published in the Journal of Hepatology The full publication can be downloaded from the Clinical Practice Guidelines section of the EASL website Please feel free to use, adapt, and share these slides for your own personal use; however, please acknowledge EASL as the source
About these slides Definitions of all abbreviations shown in these slides are provided within the slide notes When you see a home symbol like this one: topics pages, depending on which section you are in , you can click on this to return to the outline or These slides are intended for use as an educational resource and should not be used in isolation to make patient management decisions. All information included should be verified before treating patients or using any therapies described in these materials Please send any feedback to: slidedeck_feedback@easloffice.eu
Guideline panel Chair Raul J Andrade Panel members Guruprasad P Aithal, Einar S Bj rnsson, Neil Kaplowitz, Gerd A Kullak-Ublick, Dominique Larrey; Tom Hemming Karlsen (EASL Governing Board Representative) Reviewers EASL Governing Board, Didier Samuel, Tom L dde, Naga Chalasani EASL CPG DILI. J Hepatol 2019;70:1222 61.
Outline Methods Grading evidence and recommendations Methods Grading evidence and recommendations Background General concepts Epidemiology General concepts Epidemiology Background Guidelines Key recommendations Guidelines Key recommendations Future prospects New biomarkers Unresolved issues Unmet needs New biomarkers Unresolved issues Unmet needs Future prospects EASL CPG DILI. J Hepatol 2019;70:1222 61.
Methods Grading evidence and recommendations
Evidence Level of evidence based on the Oxford Centre for Evidence-based Medicine1,2 Level 1a 1b 1c 2a 2b 2c 3a 3b 4 5 Therapy / Prevention, Aetiology / Harm SR (with homogeneity) of RCTs Individual RCT with narrow confidence interval All or none* SR (with homogeneity) of cohort studies Individual cohort study (including low quality RCT [e.g. <80% follow-up]) Outcomes research; ecological studies SR (with homogeneity) of case-control studies Individual case-control study Case-series (and poor quality cohort and case-control studies) Expert opinion without explicit critical appraisal, or based on physiology, bench research or first principles *Met when all patients died before the treatment became available, but some now survive on it; or when some patients died before the treatment became available, but none now die on it 1. Oxford Centre for Evidence Based Medicine. Levels of evidence (March 2009). Available at: https://www.cebm.net/2009/06/oxford-centre-evidence-based-medicine-levels- evidence-march-2009/. Accessed March 2019; 2. Aithal GP, et al. Clin Pharmacol Ther 2011;89:806 15. EASL CPG DILI. J Hepatol 2019;70:1222 61.
Evidence Level of evidence based on the Oxford Centre for Evidence-based Medicine1,2 Level 1a 1b 1c 2a 2b Prognosis SR (with homogeneity) of inception cohort studies; CDR validated in different populations Individual inception cohort study with >80% follow-up; CDR validated in a single population All or none case-series SR (with homogeneity) of either retrospective cohort studies or untreated control groups in RCTs Retrospective cohort study or follow-up of untreated control patients in an RCT; Derivation of CDR or validated on split-sample only Outcomes research Case-series (and poor quality prognostic cohort studies) Expert opinion without explicit critical appraisal, or based on physiology, bench research or first principles 2c 4 5 1. Oxford Centre for Evidence Based Medicine. Levels of evidence (March 2009). Available at: https://www.cebm.net/2009/06/oxford-centre-evidence-based-medicine-levels- evidence-march-2009/. Accessed March 2019; 2. Aithal GP, et al. Clin Pharmacol Ther 2011;89:806 15. EASL CPG DILI. J Hepatol 2019;70:1222 61.
Evidence Level of evidence based on the Oxford Centre for Evidence-based Medicine1,2 Level 1a 1b 1c 2a 2b Diagnosis SR (with homogeneity) of Level 1 diagnostic studies; CDR with 1b studies from different clinical centres Validating cohort study with good reference standards; or CDR tested within one clinical centre Absolute SpPins and SnNouts* SR (with homogeneity) of Level >2 diagnostic studies Exploratory cohort study with good reference standards; CDR after derivation, or validated only on split-sample or databases SR (with homogeneity) of 3b and better studies Non-consecutive study; or without consistently applied reference standards Case-control study, poor or non-independent reference standard Expert opinion without explicit critical appraisal, or based on physiology, bench research or first principles 3a 3b 4 5 *Absolute SpPin = a diagnostic finding whose Specificity is so high that a Positive result rules-in the diagnosis; Absolute SnNout = a diagnostic finding whose Sensitivity is so high that a Negative result rules-out the diagnosis 1. Oxford Centre for Evidence Based Medicine. Levels of evidence (March 2009). Available at: https://www.cebm.net/2009/06/oxford-centre-evidence-based-medicine-levels- evidence-march-2009/. Accessed March 2019; 2. Aithal GP, et al. Clin Pharmacol Ther 2011;89:806 15. EASL CPG DILI. J Hepatol 2019;70:1222 61.
Evidence Level of evidence based on the Oxford Centre for Evidence-based Medicine1,2 Level 1a 1b 1c 2a 2b 2c 3a 3b 4 5 Differential diagnosis / symptom prevalence study SR (with homogeneity) of of prospective cohort studies Prospective cohort study with good follow-up All or none case-series SR (with homogeneity) of 2b and better studies Retrospective cohort study, or poor follow-up Ecological studies SR (with homogeneity) of 3b and better studies Non-consecutive cohort study, or very limited population Case-series or superseded reference standards Expert opinion without explicit critical appraisal, or based on physiology, bench research or first principles 1. Oxford Centre for Evidence Based Medicine. Levels of evidence (March 2009). Available at: https://www.cebm.net/2009/06/oxford-centre-evidence-based-medicine-levels- evidence-march-2009/. Accessed March 2019; 2. Aithal GP, et al. Clin Pharmacol Ther 2011;89:806 15. EASL CPG DILI. J Hepatol 2019;70:1222 61.
Grades of recommendation Grading is adapted from the Oxford Centre for Evidence-based Medicine1,2 Grade of recommendation A Consistent level 1 studies B Consistent level 2 or 3 studies OR extrapolations* from level 1 studies C Level 4 studies OR extrapolations* from level 2 or 3 studies D Level 5 evidence OR troublingly inconsistent or inconclusive studies of any level Grade of recommendation is not applicable where an evidence-based statement, rather than recommendation, is provided *Data used in a situation that has potentially clinically important differences from the original study situation 1. Oxford Centre for Evidence Based Medicine. Levels of evidence (March 2009). Available at: https://www.cebm.net/2009/06/oxford-centre-evidence-based-medicine-levels- evidence-march-2009/. Accessed March 2019; 2. Aithal GP, et al. Clin Pharmacol Ther 2011;89:806 15. EASL CPG DILI. J Hepatol 2019;70:1222 61.
Background General concepts Epidemiology
Idiosyncratic DILI: a complex drughost interaction1 Drug Drug Drug Cellular injury initiation Pharmacological responses Reactive metabolites, drug elimination Reactive metabolites, drug elimination Cellular injury initiation Pharmacological responses Reactive metabolites, drug elimination Toxicological responses Covalent binding, haptenization, oxidative stress, mitochondrial injury, ER stress Toxicological responses Covalent binding, haptenization, oxidative stress, mitochondrial injury, ER stress Cellular injury initiation Pharmacological responses Toxicological responses Covalent binding, haptenization, oxidative stress, mitochondrial injury, ER stress Cell death Apoptosis, necrosis, DAMP release Cell death Apoptosis, necrosis, DAMP release Drug properties Drug properties Physicochemical Pharmacological Toxicological Host factors Drug properties Host factors Possible host factors Genetic variants Race/ethnicity Age Gender Reproductive state Nutrition/alcohol/smoking Lifestyles Disease conditions Medications Gut flora Disease conditions Medications Gut flora Cell death Genetic variants Race/ethnicity Age Gender Reproductive state nutrition, alcohol, smoking Lifestyles Disease conditions Medications Gut flora Physiochemical Pharmacological Toxicological Bio-physiological effects Genetic variants Race/ethnicity Age Gender Reproductive state nutrition, alcohol, smoking Lifestyles Physiochemical Pharmacological Toxicological Bio-physiological effects Apoptosis, necrosis, DAMP release Host response to injury insult Biophysical effects Immune/inflammation Host response to injury insult Host response to injury insult Immune/ inflammation Repair Tissue injury Immune/ Clinical manifestation and outcome inflammation 1. Chen, et al. J Hepatol 2015;63:503 14. EASL CPG DILI. J Hepatol 2019;70:1222 61. Tissue injury Repair Tissue injury Repair Clinical manifestation and outcome Clinical manifestation and outcome
Epidemiology The incidence of DILI in the general population is not well known Population-based studies: France: 14 cases per 100,000 inhabitants per year1 Iceland: 19 cases per 100,000 inhabitants per year2 Korea: 12 cases of hospitalization per 100,000 inhabitants per year3 USA: 2.7 cases per 100,000 adults attending gastroenterology practices*4 Prospective registries: recruit bona fide cases, a bias for more severe hospitalized DILI Spanish DILI Registry5 DILIN6 LATINDILIN7 *Lower incidence may be due to: use of higher liver enzyme cut-offs vs. previous prospective studies; limitation of surveillance to subspecialists. 1. Sgro C, et al. Hepatology 2002;36:451 5; 2. Bj rnsson ES, et al. Gastroenterology 2013;144:1419 25.e3; 3. Suk KT, et al. Am J Gastroenterol 2012;107:1380 7; 4. Vega M, et al. Drug Saf 2017;40:783 87; 5. Andrade RJ, et al. Gastroenterology 2005;129:512 21; 6. Chalasani N, et al. Gastroenterology 2015;148:1340 52.e7; 7. Bessone F, et al. Int J Mol Sci 2016;17:313. EASL CPG DILI. J Hepatol 2019;70:1222 61.
Most common causative drug classes in large DILI populations Spain1 USA2 50 50 45 Total population (%) Total population (%) 40 40 32 30 30 17 17 16 20 20 10 10 10 5 0 0 Anti- infectives HDS CV drugs Anti- neoplastics Anti-infectives Nervous system drugs Latin America3 Musculoskeletal drugs Iceland4 50 50 Total population (%) Total population (%) 37 40 40 32 30 30 19 16 16 20 20 10 10 10 0 0 NSAIDs Anti-infectives Anti-androgens Anti-infectives HDS ISD 1. Andrade RJ, et al. Gastroenterology 2005;129:512 21; 2. Chalasani N, et al. Gastroenterology 2015;148:1340 52.e7; 3. Bessone F, et al. Int J Mol Sci 2016;17:313; 4. Bj rnsson ES, et al. Gastroenterology 2013;144:1419 25.e3. EASL CPG DILI. J Hepatol 2019;70:1222 61.
DILI qualification DILI can present with a very heterogeneous phenotype Liver biopsy is not available in most instances Qualification of liver injury for practical and scientific purposes is made by liver biochemistry1 ALT 5x ULN ALP 2x ULN ALT 3x ULN + TBL >2x ULN Pattern of liver injury is classified according to R (ALT x ULN/ALP x ULN)1 Hepatocellular = R 5 Cholestatic = R 2 Mixed = 2>R<5 1. Aithal GP, et al. Clin Pharmacol Ther 2011;89:806 15. EASL CPG DILI. J Hepatol 2019;70:1222 61.
Hys law: a sensitive and specific predictor of a drugs potential to cause severe liver injury In the late 1960s, Hyman Zimmerman discovered a combination of jaundice and drug-induced hepatocellular injury was associated with a 10 50% fatality rate from liver failure Temple s definition of Hy s Law cases used by the FDA in drug development: ALT >3x ULN and TBL >2x ULN without significant ALP increase New Hy s Law proposed by the Spanish DILI Registry: nR [(ALT or AST*/ULN)/(ALP/ULN)] >5 and TBL >2 ULN1 ALT >3x ULN; TBL >2x ULN 90 44 0.67 nR 5; R 5; TBL >2x ULN 83 67 0.74 TBL >2x ULN 90 63 0.77 Sensitivity, % Specificity, % AUROC *whichever higher 1. Robles Diaz M, et al, Gastroenterology 2014;147:109 18; 2. Hayashi PH, et al. Hepatology, 2017; 66:1275 85. EASL CPG DILI. J Hepatol 2019;70:1222 61.
Hys law: a sensitive and specific predictor of a drugs potential to cause severe liver injury In the late 1960s, Hyman Zimmerman discovered a combination of jaundice and drug-induced hepatocellular injury was associated with a 10 50% fatality rate from liver failure Temple s definition of Hy s Law cases used by the FDA in drug development: ALT >3x ULN and TBL >2x ULN without significant ALP increase New Hy s Law proposed by the Spanish DILI Registry: nR [(ALT or AST*/ULN)/(ALP/ULN)] >5 and TBL>2 ULN1 new R ratio for Hy s law better identified risk for death compared with the original Hy s law2 In an independent population cohort ALT >3x ULN; TBL >2x ULN 90 44 0.67 nR 5; R 5; TBL >2x ULN 83 67 0.74 TBL >2x ULN 90 63 0.77 Sensitivity, % Specificity, % AUROC *whichever higher 1. Robles Diaz M, et al, Gastroenterology 2014;147:109 18; 2. Hayashi PH, et al. Hepatology, 2017; 66:1275 85. EASL CPG DILI. J Hepatol 2019;70:1222 61.
Guidelines Key recommendations
Topics Click on a topic to skip to that section 1. 2. 3. 4. 5. 6. 7. Definition and classification of liver injury Diagnosis Genetic testing Therapy Management of drug-induced acute liver failure Preventing DILI Specific phenotypes EASL CPG DILI. J Hepatol 2019;70:1222 61.
Definition and classification of liver injury Serum aminotransferases (ALT/AST), ALP, and TBL levels remain the mainstay for detecting and classifying liver damage in suspected DILI Recommendations General DILI should be classified as hepatocellular, cholestatic or mixed according to the pattern of elevation of liver enzymes based on the first set of laboratory tests available in relation to the clinical event Aminotransferases ALT, ALP and TBL are the standard analytes to define liver damage and liver dysfunction in DILI. AST values can reliably substitute ALT in calculating the pattern of injury when the latter is unavailable at DILI recognition, whereas GGT is less reliable as an ALP substitute Persistently elevated TBL and ALP in the second month from DILI onset should be used as a marker for chronic DILI Grade of evidence Grade of recommendation Extrapolation from level 2 studies B Extrapolation from level 2b studies C Level 1b studies B EASL CPG DILI. J Hepatol 2019;70:1222 61.
Diagnosis of DILI relies largely on exclusion of alternative causes of liver damage Recommendations Laboratory work-up Tests for HCV-RNA and ant-HEV IgM (or HEV-RNA) are suggested in patients with suspected DILI to exclude acute hepatitis C and/or E, particularly in those cases not compatible with the drug signature of the suspected causative agent and/or with high transaminase levels Grade of evidence Grade of recommendation Extrapolation from level 2 studies C Imaging An abdominal ultrasound should be undertaken in all patients suspected of DILI. The use of additional imaging studies relies on the clinical context Level 2a B Liver biopsy Liver biopsy may be considered during the investigation of selected patients suspected to suffer DILI, as liver histology can provide information that can support the diagnosis of DILI or an alternative diagnosis Level 5 D Liver biopsy may be performed in patients suspected to have DILI when serology raises the possibility of AIH Level 4 studies C Liver biopsy may be considered in patients when suspected DILI progresses or fails to resolve on withdrawal of the causal agent as the liver histology may provide prognostic information assisting clinical management Level 4 C EASL CPG DILI. J Hepatol 2019;70:1222 61.
Diagnosis: determining causality Causality assessment may increase objectivity in the evaluation of suspected DILI Recommendations Causality assessment methods and scales CIOMS can be used to assess causality, guiding a systematic and objective evaluation of patients suspected to have DILI Grade of evidence Grade of recommendation Level 2b studies C Positive rechallenge with suspected drug is strong proof of causality1 Recommendations Rechallenge Deliberate rechallenge with the causative drug in clinical practice is not advocated, unless the clinical scenario demands such an exposure, as it can cause more severe hepatotoxicity Controlled rechallenge after an episode of liver injury is, however, considered justified in relation to oncology and anti-TBC therapy, as they generally do not result in severe recurrence of hepatotoxicity Level 4 C Level 1b studies B 1. Andrade RJ, et al. Expert Opin Drug Saf 2009;8:709 14. EASL CPG DILI. J Hepatol 2019;70:1222 61.
Genetic testing Genetic testing in DILI with a number of drugs using GWAS has identified several common variants in HLA alleles implicating the immune system Recommendations HLA genotyping should be utilised in selected clinical scenarios where genetic tests assist the diagnosis and management of patients HLA genotyping may be used to support the diagnosis of DILI due to specific drugs or distinguish DILI from AIH. Further validation of genetic testing is required before routine implementation can be recommended Grade of evidence Grade of recommendation Extrapolation from level 1 studies B Level 5 D EASL CPG DILI. J Hepatol 2019;70:1222 61.
Diagnosis: a stepwise approach Abnormal biochemistry/acute hepatitis DILI suspicion Features supporting toxic aetiology Skin involvement, kidney injury, previous DILI episodes Careful enquiry of exposure to HDS, drugs, OTC drugs* Discontinue non-essential drugs/HDS treatment Potential pitfalls Lack of information (eg. dose, duration), several medications, hidden HDS and OTC drug intake Search in hepatotoxicity resources (Liver tox) Calculate biochemical pattern of liver injury Hepatocellular R 5 Mixed 2 > R < 5 Cholestatic 2 ???/??? ???/??? (?) *record start and stop dates; hepatic vascular disease, chronic hepatitis, fibrosis, microvesicular steatosis EASL CPG DILI. J Hepatol 2019;70:1222 61.
Diagnosis: a stepwise approach Abnormal biochemistry/acute hepatitis DILI suspicion Features supporting toxic aetiology Skin involvement, kidney injury, previous DILI episodes Careful enquiry of exposure to HDS, drugs, OTC drugs* Discontinue non-essential drugs/HDS treatment Potential pitfalls Lack of information (eg. dose, duration), several medications, hidden HDS and OTC drug intake Search in hepatotoxicity resources (Liver tox) Calculate biochemical pattern of liver injury Hepatocellular R 5 Mixed 2 > R < 5 Cholestatic 2 ???/??? ???/??? (?) Search for alternative causes *record start and stop dates; hepatic vascular disease, chronic hepatitis, fibrosis, microvesicular steatosis EASL CPG DILI. J Hepatol 2019;70:1222 61.
Diagnosis: a stepwise approach Abnormal biochemistry/acute hepatitis DILI suspicion Features supporting toxic aetiology Skin involvement, kidney injury, previous DILI episodes Careful enquiry of exposure to HDS, drugs, OTC drugs* Discontinue non-essential drugs/HDS treatment Potential pitfalls Lack of information (eg. dose, duration), several medications, hidden HDS and OTC drug intake Search in hepatotoxicity resources (Liver tox) Calculate biochemical pattern of liver injury Hepatocellular R 5 Mixed 2 > R < 5 Cholestatic 2 ???/??? ???/??? (?) Search for alternative causes Viral infections (HAV, HBV, HCV, HEV, EBV, CMV) Alcohol-related liver disease, hepatic ischaemia Autoantibody titres, IgG *record start and stop dates; hepatic vascular disease, chronic hepatitis, fibrosis, microvesicular steatosis EASL CPG DILI. J Hepatol 2019;70:1222 61.
Diagnosis: a stepwise approach Abnormal biochemistry/acute hepatitis DILI suspicion Features supporting toxic aetiology Skin involvement, kidney injury, previous DILI episodes Careful enquiry of exposure to HDS, drugs, OTC drugs* Discontinue non-essential drugs/HDS treatment Potential pitfalls Lack of information (eg. dose, duration), several medications, hidden HDS and OTC drug intake Search in hepatotoxicity resources (Liver tox) Calculate biochemical pattern of liver injury Hepatocellular R 5 Mixed 2 > R < 5 Cholestatic 2 ???/??? ???/??? (?) Search for alternative causes Viral infections (HAV, HBV, HCV, HEV, EBV, CMV) Alcohol-related liver disease, hepatic ischaemia Autoantibody titres, IgG Benign/malignant biliary obstruction Primary biliary cholangitis Primary sclerosing cholangitis *record start and stop dates; hepatic vascular disease, chronic hepatitis, fibrosis, microvesicular steatosis EASL CPG DILI. J Hepatol 2019;70:1222 61.
Diagnosis: a stepwise approach Abnormal biochemistry/acute hepatitis DILI suspicion Features supporting toxic aetiology Skin involvement, kidney injury, previous DILI episodes Careful enquiry of exposure to HDS, drugs, OTC drugs* Discontinue non-essential drugs/HDS treatment Potential pitfalls Lack of information (eg. dose, duration), several medications, hidden HDS and OTC drug intake Search in hepatotoxicity resources (Liver tox) Calculate biochemical pattern of liver injury Hepatocellular R 5 Mixed 2 > R < 5 Cholestatic 2 ???/??? ???/??? (?) Search for alternative causes Viral infections (HAV, HBV, HCV, HEV, EBV, CMV) Alcohol-related liver disease, hepatic ischaemia Autoantibody titres, IgG Benign/malignant biliary obstruction Primary biliary cholangitis Primary sclerosing cholangitis Consider liver biopsy if Negative or incomplete rechallenge Acute or chronic atypical presentation Autoimmune hepatitis *record start and stop dates; hepatic vascular disease, chronic hepatitis, fibrosis, microvesicular steatosis EASL CPG DILI. J Hepatol 2019;70:1222 61.
Therapy Toxic liver damage is still an orphan hepatic disease with respect to therapy Most important initial step in terms of management of suspected DILI is to discontinue the implicated agent Recommendations Specific therapies Cholestyramine: a short administration may be used to decrease the course of hepatotoxicity induced by very selected drugs, such as leflunomide and terbinafine Carnitine may be used to decrease the course of valproate hepatotoxicity The efficacy of NAC to improve the severity of liver injury from drugs other than paracetamol may not be significantly substantiated The efficacy of UDCA to reduce the severity of liver injury may not be significantly substantiated Grade of evidence Grade of recommendation Level 4 C Level 4 Inconclusive Level 4 Inconclusive Level 4 C D D EASL CPG DILI. J Hepatol 2019;70:1222 61.
Management of drug-induced acute liver failure DILI is the most common cause of acute liver failure in western countries1,2 Recommendations In case of drug-induced ALF, liver transplantation should be considered as a therapeutic option Adults with idiosyncratic drug-induced ALF should receive NAC early in the course (coma grade I II) Grade of evidence Grade of recommendation Consistent level 2 studies B Extrapolation from level 1b study B In idiosyncratic DILI, routine use of corticosteroid treatment may not be substantiated Level 4 studies C 1. Ostapowitz G, et al. Ann Intern Med 2002;137:947 54; 2. Wei G, et al. J Intern Med 2007;262:393 401. EASL CPG DILI. J Hepatol 2019;70:1222 61.
Preventing DILI Pre- and post-marketing surveillance of drugs using liver biochemistry is warranted to decrease the incidence of DILI Recommendations Systematic monitoring of liver tests can be necessary for drugs with known DILI liability in clinical development. In the postmarketing setting, drugs with a relevant risk may have a boxed warning for hepatotoxicity, in which case intensified monitoring and surveillance of liver function is indicated Hy s law should be considered to identify patients at risk of progressing to severe DILI in the setting of clinical trials. Thresholds for interrupting or stopping treatment with a study drug as recommended by the FDA are intended as guidelines for studies in drug development and may be adapted depending on individual risk-benefit assessment. Grade of evidence Grade of recommendation Inconclusive level 2b studies D Consistent level 2b studies B EASL CPG DILI. J Hepatol 2019;70:1222 61.
Specific phenotypes: AIH A number of drugs have been associated with drug-induced AIH A syndrome that shares many features of idiopathic AIH In cohorts of cases with the diagnosis of AIH, 2 9% were considered to be drug-induced Conversely, drug-induced AIH accounts for 9% of all DILI Recommendations Suspected drug-induced AIH should be evaluated in detail including causality assessment, serology, genetic tests and liver biopsy whenever possible Grade of evidence Grade of recommendation Extrapolation from level 2 studies B In patients with suspected drug-induced AIH and treated with corticosteroids, withdrawal of therapy once the liver injury has resolved should be accompanied by close monitoring Level 2a studies B EASL CPG DILI. J Hepatol 2019;70:1222 61.
Specific phenotypes: Cancer immunotherapy-induced DILI Immune checkpoint inhibitors act by increasing anti-tumour immune response supressed in cancer The break in tumour tolerance is associated with inflammatory side effects and an increase in immune-related adverse events, including hepatotoxicity Statement Immune checkpoint inhibitors can induce immune related hepatotoxicity in a substantial proportion of patients, with CTLA-4 inhibitors (ipilimumab) being more hepatotoxic than PD-L1 agents (nivolumab), and combination treatments carrying a greater risk Level 1a studies Recommendations It is suggested that decisions regarding corticosteroid treatment of immune mediated hepatitis associated with immune checkpoint inhibitors are made by a multidisciplinary team involving hepatologists if DILI is sufficiently severe based on clinical and histological assessment Grade of evidence Grade of recommendation Level 2 studies C EASL CPG DILI. J Hepatol 2019;70:1222 61.
Specific phenotypes: Secondary sclerosing cholangitis Strictures of the bile tract may result from ischaemia or drug toxicity1 Recommendations Diagnosis of drug-induced secondary sclerosing cholangitis can be considered in patients with a cholestatic pattern of DILI with slow resolution of liver injury and characteristic changes in the biliary system demonstrated on MRCP or ERCP Grade of evidence Grade of recommendation Extrapolation from level 2 studies C 1. Gudnason HO, et al. Dig Liver Dis 2015;47:502 7. EASL CPG DILI. J Hepatol 2019;70:1222 61.
Specific phenotypes: Granulomatous hepatitis Hepatic granulomas are reported in 2 15% of liver biopsies1 Of those with granulomatous hepatitis, 2.5% are considered drug-related Recommendations Diagnosis of drug-related granulomatous hepatitis is suggested to involve expert evaluation of liver histology as well as exclusion of specific infections, inflammatory and immunological conditions that are well recognized causes of hepatic granulomata Grade of evidence Grade of recommendation Level 5 D 1. Drebber U, et al. Liver Int 2008;28:828 34. EASL CPG DILI. J Hepatol 2019;70:1222 61.
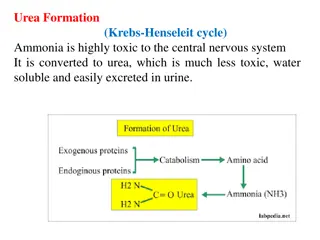
Specific phenotypes: Acute fatty liver Rare form of acute hepatotoxicity related to microvesicular steatosis Manifested with hypoglycaemia, lactic acidosis, hyperammonaemia and cerebral oedema Dramatically rapid development of organ failure precedes clinical syndrome With an acute rise in liver enzymes and jaundice An index of suspicion is crucial in identifying the drug aetiology when approaching a patient with anicteric hepatic encephalopathy Recommendations Acute drug-induced fatty liver can be recognized based on its distinct clinicopathological characteristics in people exposed to drugs such as valproate that are known to interfere with mitochondrial function Grade of evidence Grade of recommendation Level 2 Studies C EASL CPG DILI. J Hepatol 2019;70:1222 61.
Specific phenotypes: Drug-associated fatty liver disease (DAFLD) NAFLD is associated with accumulation of fat in >5% of hepatocytes With or without inflammation and fibrosis In those with moderate or lower alcohol consumption <21 units in men and <14 units in women, per week Certain drugs may be one of the aetiologies behind a proportion of secondary NAFLD Cases not associated with characteristic features of metabolic syndrome Where no risk factors are obvious Recommendations Particular drugs such as amiodarone, methotrexate and tamoxifen and the chemotherapeutic agents 5-fluorouracil and irinotecan, should be considered as risk factors for fatty liver disease and decisions to continue or withdraw the medication relies upon the benefits of the treatment against the risk of progressive liver disease Grade of evidence Grade of recommendation Extrapolation from level 1 studies B EASL CPG DILI. J Hepatol 2019;70:1222 61.
Specific phenotypes: Nodular regenerative hyperplasia Drugs can injure endothelial cells of sinusoids and portal venules1 Wide spread vascular changes lead to diffuse nodularity within the hepatic parenchyma Withdrawal of associated medication has been shown to lead to histological resolution Otherwise, management is focused on surveillance and prevention of manifestations of portal hypertension Recommendations Drugs may be considered as risk factors for nodular regenerative hyperplasia and when possible it is suggested that the specific drug that has been associated is withdrawn Grade of evidence Grade of recommendation Extrapolation level 4 studies D 1. Vernier-Massouille G, et al. Gut 2007;56:1404 9. EASL CPG DILI. J Hepatol 2019;70:1222 61.
Specific phenotypes: Liver tumours Causal association between hormonal therapy and liver tumours is supported by epidemiological data Statements Oral contraceptives may be considered risk factors for the development of liver tumours Consistent level 2 studies Androgens and androgenic steroids particularly in the context of treating bone marrow failure, may be considered risk factors for the development of liver tumours Level 5 Recommendations Withdrawal of medications is suggested where possible with continued monitoring until regression of adenoma or definitive treatment Grade of evidence Grade of recommendation Inconsistent level 4 evidence D EASL CPG DILI. J Hepatol 2019;70:1222 61.
Future prospects New biomarkers Unresolved issues Unmet needs
Beyond serum ALT: Exploratory circulating biomarkers for DILI Immune cell Necrosis Hepatocyte HMGB1 HMGB1 ALT Hepatocyte injury Keratin-18 (FL) mIr-122 M-CSF1 Regeneration Keratin-18 (CC) GLDH HMGB1-acetyl Mitochondrial dysfunction Apoptosis Immune cell activation Kullak-Ublick G. DILI Conference XVII, 2017; Session IV. EASL CPG DILI. J Hepatol 2019;70:1222 61.
SAFE-Ts new liver safety biomarkers Nine new liver safety biomarkers supported by the EMA and/or FDA for exploratory use in clinical drug development: Marker Total HMGB1 Hyperacetylated HMGB1 Osteopontin Total keratin 18 Caspase-cleaved keratin 18 M-CSFR1 miR-122 GLDH SDH Application Mechanism (necrosis), prognosis Mechanism (immune activation), prognosis Prognosis Mechanism (necrosis), prognosis Mechanism (apoptosis), prognosis Mechanism (immune activation), prognosis Detection, mechanism (hepatocyte leakage) Detection, mechanism (mitochondrial injury) Detection Kullak-Ublick G. DILI Conference XVII, 2017; Session IV. EASL CPG DILI. J Hepatol 2019;70:1222 61.
Unresolved issues and unmet needs Epidemiology Big data analysis Estimates of socioeconomic burden of DILI and its impact on quality of life Robust case-control or population-based cohort studies to evaluate the risk of HDS- related liver injury, botanical identification and chemical analysis Pathogenesis Identify the factors that unmask or prevent liver injury as well as the determinants of severity of DILI in subjects otherwise genetically predisposed Diagnosis and outcome Discovery, evaluation and validation of biomarkers, which can distinguish self-resolving elevation of liver enzymes related to drugs from those with a potential to evolve into symptomatic DILI Better prediction of DILI subjects at risk of ALF, including prognostic biomarkers Therapy Randomized controlled trials to evaluate the effect of specific interventions on the clinical outcomes of DILI Prediction Algorithms that reliably predict the DILI liability considering drug host factors EASL CPG DILI. J Hepatol 2019;70:1222 61.