Musculoskeletal Pelvis & Perineum Overview
Explore the anatomy of the pelvis and perineum, including the osseous pelvis structure, features, ligaments, and pelvic regions. Learn about the division of the abdominopelvic cavity and key neurovascular structures in this comprehensive PowerPoint presentation.
Download Presentation
Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
Presentation Transcript
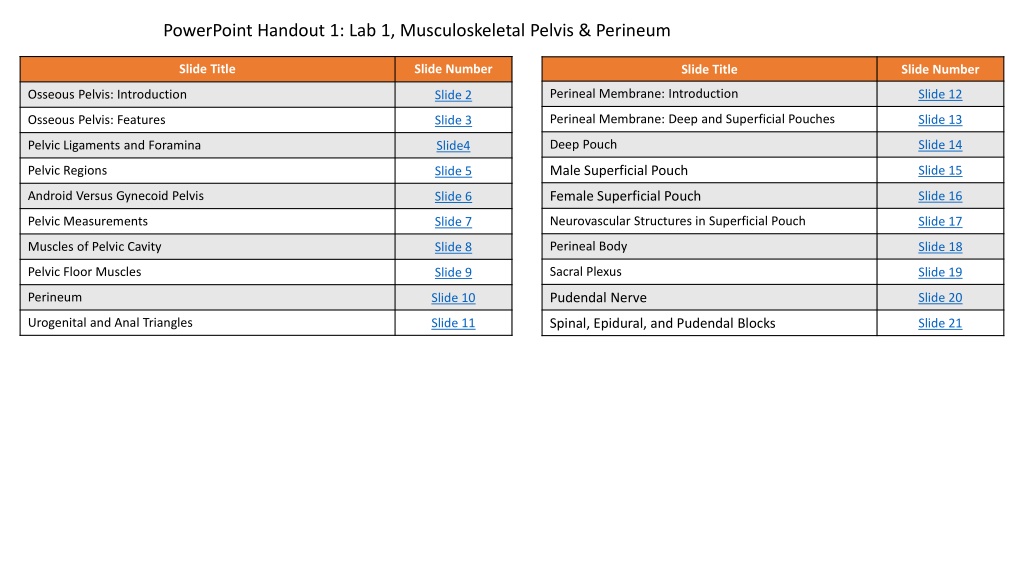
PowerPoint Handout 1: Lab 1, Musculoskeletal Pelvis & Perineum Slide Title Slide Number Slide Title Slide Number Perineal Membrane: Introduction Slide 12 Osseous Pelvis: Introduction Slide 2 Perineal Membrane: Deep and Superficial Pouches Slide 13 Osseous Pelvis: Features Slide 3 Deep Pouch Slide 14 Pelvic Ligaments and Foramina Slide4 Male Superficial Pouch Slide 15 Pelvic Regions Slide 5 Female Superficial Pouch Android Versus Gynecoid Pelvis Slide 16 Slide 6 Neurovascular Structures in Superficial Pouch Pelvic Measurements Slide 17 Slide 7 Perineal Body Muscles of Pelvic Cavity Slide 18 Slide 8 Sacral Plexus Pelvic Floor Muscles Slide 19 Slide 9 Pudendal Nerve Perineum Slide 20 Slide 10 Urogenital and Anal Triangles Spinal, Epidural, and Pudendal Blocks Slide 11 Slide 21
Osseous Pelvis: Introduction The pelvis is the region of the body surrounded by a ring of bones that structurally connects the vertebral column to the lower extremity. The axial skeleton and the appendicular skeleton both contribute bones to the pelvis. The axial skeleton's contribution to the pelvis is the sacrum and the coccyx. The appendicular skeleton's contribution to the pelvis is the right and left hip bones (pelvic bones or os coxae), which are joined anteriorly by the fibrocartilaginous pubic symphysis. The mature hip bones are formed by the fusion of three bones. Ilium Ischium Pubis Posterior Anterior
Osseous Pelvis: Features Osteology of the pelvis Anterior superior iliac spine (ASIS) Anterior inferior iliac spine Pelvic brim Sacral promontory Sacral ala Iliopectineal (iliopubic) line Superior margin pubic symphysis Ischial spine Ischial tuberosity Ischiopubic ramus Pubic arch Pubic tubercle Acetabulum Obturator foramen Pubic symphysis It is important to note that the pubic tubercles and the anterior superior iliac spines are in the same vertical plane when the pelvis is in its anatomical position. Anterior Inferior Iliac Spine Pubic Arch Iliopectineal (iliopubic) ine Ischiopubic Ramus
Pelvic Ligaments and Foramina Pelvic ligaments Obturator membrane Sacrotuberous ligament Sacrospinous ligament Anterior and posterior sacroiliac ligaments Pelvic foramina whose boundaries are formed partially by ligaments Greater sciatic foramen Lesser sciatic foramen Obturator canal
Pelvic Regions The pelvic brim divides the abdominopelvic cavity into the abdominal cavity superiorly and the and the pelvic cavity inferiorly. The abdominal cavity is the space between the diaphragm and the pelvic brim (pelvic inlet). The pelvic cavity is the space between the pelvic brim (pelvic inlet) and the muscular pelvic floor. The pelvic brim divides the pelvis into two regions. The greater pelvis (aka: false pelvis) is the space within the pelvis between the level of the iliac crests and the pelvic brim. The space within the greater pelvis is a component of the abdominal cavity. The lesser pelvis (aka: true pelvis) is the space between the pelvic brim (pelvic inlet) and the pelvic diaphragm (muscular floor of the pelvis). The space within the lesser pelvis is a component of the pelvic cavity. Iliac Crest False pelvis Pelvic Brim (Inlet) True pelvis
Android Versus Gynecoid Pelvis An android (male-like) pelvis can be differentiated from a gynecoid (female-like) pelvis by comparing the shape of the pelvic inlet, the size and shape of the pelvic outlet, and the subpubic angle (See Table 1). Table 1 Female Male
Pelvic Measurements The size of the lesser pelvis is important in obstetrics because it determines, to a large extent, the capacity for vaginal childbirth. Several measurements, determined radiographically or manually during pelvic examination, are used to assess the size of the lesser pelvis and its suitability for a vaginal delivery. The interspinous distance is the transverse distance between the ischial spines, which is typically the narrowest diameter of the birth canal. The transverse diameteris the distance between the inner edges of the ischial tuberosities. The true (anatomical) conjugate diameter is the distance between the sacral promontory and the most superior point on the pubic symphysis. This distance can only be measured on radiographs. The obstetrical conjugate diameter is the shortest distance between the sacral promontory and the pubic symphysis. This distance cannot be measured directly during the pelvic examination but can be calculated by first determining the diagonal conjugate diameter (see below). The diagonal conjugate diameter is the distance between the sacral promontory (palpated by the middle finger) and the anterior surface of the pubic symphysis' inferior margin. This distance can be determined during a pelvic examination, which is then used to calculate the obstetrical conjugate. Once the diagonal conjugate is measured, the examiner subtracts 1.5 to 2 cm from the diagonal conjugate measurement. Obstetrical Conjugate Diagonal Conjugate Obstetrical conjugate calculated after hand withdrawn. (Example: 13.5 cm (Diagonal) 2 cm = 11.5 cm (Obstetric)
Muscles of Pelvic Cavity Pelvic muscles contribute to the walls and floor of the pelvic cavity. Lateral walls Obturator internus muscle: The obturator internus muscle inserts on the internal surface of the obturator membrane and passes through the lesser sciatic foramen to insert on the greater trochanter of the femur. Within the pelvis, the obturator internus muscle is covered in thick fascia called the obturator fascia. Posterior walls Piriformis muscle: The proximal attachment of the piriformis muscle is on the anterior aspects of the S2-4 vertebral segments and passes through the greater sciatic foramen to its distal attachment on the greater trochanter of the femur. Floor The pelvic floor (pelvic diaphragm) is a funnel--shaped structure composed of the following muscles: levator ani and coccygeus (next slide). Pelvic Diaphragm
Pelvic Floor Muscles https://3d4medic.al/8K6xxapi The following muscles form the funnel-shaped pelvic floor (pelvic diaphragm). Levator ani (consisting of 3 muscles) Puborectalis muscle Pubococcygeus muscle Iliococcygeus muscle: (Note that the iliococcygeus muscle has its origin on the tendinous arch, which is continuous with the obturator fascia.) Coccygeus (ischiococcygeus) muscle The coccygeus muscle's superior border is adjacent to the inferior border of the piriformis muscle. Its origin is on the ischial spine and the pelvic surface of the sacrospinous ligament. It inserts onto the lateral margin of coccyx and the most inferior portion of sacrum.
Perineum The funnel-shaped pelvic floor (diaphragm) forms a physical boundary between the pelvic cavity and the perineum. The perineum is a diamond-shaped region of the body wall inferior to the pelvic diaphragm between the buttocks and thighs. Its borders consist of the following structures. Anterior: inferior border of pubic symphysis Anteriolateral margin: ischiopubic ramus Posteriolateral margin: sacrotuberous ligament Posterior: tip of coccyx The pelvic floor contains openings for important structures to pass between the pelvic cavity and the perineum. The urogenital hiatus is an anterior opening in the pelvic floor through which structures pass to enter the in the urogenital triangle of the perineum. Note that different structures pass through this hiatus in males as compared to females In males the urethra passes from the lesser pelvis to the perineum via the urogenital hiatus. In females the urethra and vagina pass from the lesser pelvis to the perineum via the urogenital hiatus. rectal hiatus (anal aperture) The rectal hiatus (anal aperture) is a posterior opening of the pelvic floor through with the anal canal passes to enter the anal triangle region of the perineum.
Urogenital and Anal Triangles The diamond-shaped perineum can be further subdivided into two triangular regions (urogenital triangle and anal triangle) by an imaginary line connecting the two ischial tuberosities. Take note that the two triangles are not in the same plane when the pelvis is in anatomical position. The urogenital triangle is the anterior triangular region of the diamond-shaped perineum In anatomical position, the urogenital triangle is oriented in a horizontal plane. The urogenital triangle contains the urethra and external genitalia. The anal triangle is the posterior triangular region of the diamond-shaped perineum In anatomical position, the anal triangle is oriented in a plane that is almost vertical. The anal triangle contains the anal canal, anus, external anal sphincter, inferior rectal nerve (branch of pudendal nerve), and the fat-filled ischioanal fossa. Urogenital Triangle rectal hiatus (anal aperture) Anal Triangle
Perineal Membrane: Introduction The perineal membrane is an important fascial layer within the urogenital triangle. Its attachments are on the ischial tuberosities and the ischiopubic rami. The posterior margin of the perineal membrane is NOT attached to bone but is anchored at its midline to the perineal body. The perineal membrane creates an important boundary that separates the perineum into two spaces. (See next slide for details.) A deep space (pouch) superior to the perineal membrane A superficial space (pouch) inferior the perineal membrane
Perineal Membrane: Deep and Superficial Pouches Figure 2 The perineal membrane separates the urogenital triangle into two pouches (spaces). By definition, the deep perineal pouch (space) is the space located between the perineal membrane and the fascia covering the inferior side of the pelvic floor (diaphragm) muscles (Figure 1). However, there are many inconsistencies in diagrams as to what constitutes the deep perineal space. I think it is easiest to consider the deep space as consisting of two subregions. Fibromuscular region: This is the thin region of muscle resting on the superior side of the perineal membrane. In older textbooks, this is a structure that was described as the urogenital diaphragm. (Some present authors call this the perineal membrane. ) This region of the deep space contains skeletal muscle, neurovascular structures, and the bulbourethral glands in males. The anterior recess of the ischioanal fossa is an anterior continuation of the fat- filled ischioanal fossa. The anterior recess is located between the fibromuscular portion of the deep pouch and the levator ani muscles. The medial region of the anterior recess is smaller in size compared to the lateral region. The superficial perineal pouch (space) is located between the perineal membrane and membranous superficial fascia (Colles fascia). Figure 1 Pelvic Diaphragm Deep Pouch (A Recess Ischioanal Fossa) Deep Pouch (Fibromuscular Region) Urogenital Diaphragm Superficial Pouch Colles Fascia Perineal Membrane
Deep Pouch Male Deep Perineal Space The fibromuscular region of the the deep pouch differs by gender. Male deep Pouch Deep transverse perineal muscle Urethra passes through the deep space External urethral sphincter Bulbourethral glands Internal pudendal artery and branches Dorsal nerve of penis Female Deep Pouch Deep transverse perineal muscle Urethra and vagina passes through the deep space External urethral sphincter Compressor urethrae muscle Urethrovaginalis sphincter muscle Internal pudendal artery and branches Dorsal nerve of clitoris Female Deep Perineal Space Note on Anatomical Terminology: The perineal membrane is sometimes referred to as the inferior fascia of the urogenital (UG) diaphragm. However, the UG diaphragm is a structure now considered to no longer exist. It was described as a single (thin) layer of skeletal muscle sandwiched between the deep fascia of the pelvic diaphragm, which inferiorly is the perineal membrane and superiorly the superior fascia of the urogenital diaphragm." However, evidence of the superior fascia is lacking. In addition, the external urethral sphincter (sphincter urethrae muscle) was previously thought to be the principle content of the deep pouch. However, the external urethral sphincter is now recognized to be contained within the wall of the urethra and extends superiorly beyond the thin region that was formerly identified as the urogenital diaphragm. External Urethral Sphincter
Male Superficial Pouch The following structures are located within the male superficial pouch. The superficial transverse perineal muscles extend from the ischial tuberosities and the rami to the perineal body medially. They function to stabilize the perineal body. The root of the penis (bulb and crura) and muscles (ischiocavernosus and bulbospongiosus) surroundingthe root are in the superficial pouch. Details of these structures will be explained in a future lab. Bulb + Crura = Root surrounds crura surrounds bulb
Female Superficial Pouch The following structures are located within the female superficial pouch. The superficial transverse perineal muscles extend from the ischial tuberosities and the rami to the perineal body medially. They function to stabilize the perineal body. The greater vestibular (Bartholin's) glands The bulbs of the vestibule, the crura, and muscles (ischiocavernosus and bulbospongiosus) surrounding the bulb and crura are all located in the superficial pouch. Details of these structures will be explained in a future lab.
Neurovascular Structures in Superficial Pouch The following neurovascular structures are located within the superficial pouch. Perineal branches of internal pudendal artery Perineal branches of pudendal nerve
Perineal Body The perineal body is an important fibromuscular structure maintaining the integrity of the pelvic floor. It is located in the midline of the body along the posterior border of the perineal membrane where the urogenital and anal triangles meet. It is a central attachment point for the following structures/muscles. Perineal membrane Anterior muscle fibers of levator ani External anal sphincter Bulbospongiosus muscle External urethral sphincter Superficial and deep transverse perineal muscles Sphincter urethrovaginalis (females) CLINICAL ANATOMY: The perineal body is especially important in women because it is the final support of the pelvic viscera. Disruption of the perineal body can result in loss of support and prolapse of pelvic viscera. Coccygeus Obturator Internus Levator Ani
Sacral Plexus The sacral plexus is located anterior to the piriformis muscle in the pelvic cavity. It is composed of the S1-S4 ventral rami that enter the pelvic cavity by passing through the anterior sacral foramina. The sacral plexus receives nerve fiber contributions from the lumbar plexus via the lumbosacral trunk to form the lumbosacral plexus. The lumbosacral trunk consists of some axons from the L4 ventral ramus and all the axons from the L5 ventral ramus. The lumbosacral trunks enter the pelvic cavity by passing inferiorly across the sacral alae.
Pudendal Nerve Lumbosacral plexus branches See MSI Labs 4 and 5 to review the branches of the lumbosacral plexus that supply the lower extremity. The pudendal nerve branches from the S2-S4 ventral rami of the sacral plexus. It exits the pelvic cavity inferior to the piriformis muscle via the greater sciatic foramen. It passes around the sacrospinous ligament to enter the lesser sciatic foramen. It then courses through the ischioanal fossa along its lateral wall within the fascia of the obturator internus muscle called the pudendal (Alcock s) canal. Branches The inferior rectal nerves supply the external anal sphincter and skin of perianal region inferior to pectinate line. The perineal nerve branches from the pudendal nerve and ultimately divides into two branches. The superficial perineal nerve branch becomes the posterior scrotal nerve (male) or labial nerves (female) providing sensation to those areas. The deep perineal (motor) nerve branch supplies muscles of the perineum and pelvic floor (external urethral sphincter, bulbospongiosus, ischiocavernosus, and levator ani muscles). The pudendal continues as the dorsal nerve of the penis or clitoris, which penetrates the perineal membrane to provide sensory innervation to the skin of the penis or clitoris.
Spinal, Epidural, and Pudendal Blocks CLINICAL ANATOMY: Spinal Block vs Epidural Block A spinal block is the delivery of anesthesia into the CSF of the subarachnoid space by a single injection. The anesthesia usually begins to take effect within 1 minute and results in anaesthetizing the body below, and sometimes above, the site of injection. After administration, the patient may not be able to move his or her lower extremities until the anesthetic wears off. A headache may follow the procedure, which is most likely a result of CSF leakage at the injection site. An epidural block is the administration of an anesthetic and analgesic into the epidural space through a catheter. This method provides greater control of prolonged pain relief because of continuous, controlled infusion. To anesthetize the lower extremity and pelvis, this procedure can be done in the same location as a lumbar puncture. If the anesthesia is introduced into the sacral canal via the sacral hiatus (caudal epidural block), only the S2-S4 nerve roots are anesthetized (birth canal, pelvic floor, and external genitalia). This procedure spares the lower extremity, which is why it is a popular choice for participatory child birth. However, it must be administered in advance of the actual delivery. CLINICAL ANATOMY: A pudendal nerve block is a common anesthesia technique for perineal anesthesia during obstetric procedures, including vaginal birth during the second stage of labor, vaginal repairs, and anorectal surgeries such as hemorrhoidectomies. The pudendal nerve is anesthetized where it enters the lesser sciatic foramen, 1 cm inferior and medial relative to the attachment of the sacrospinous ligament to the ischial spine. This procedure can be accomplished by the following approaches: transvaginal (figure), transperineal, or perirectal.