Update on Mental Health, Infection Prevention, Staff Vaccine, and Testing in NHS England and NHS Improvement
In the agenda for the meeting on 20th November 2020, topics included updates on mental health, staff flu vaccine and testing, infection prevention, and nosocomial infections in NHS England and NHS Improvement. The importance of preventing COVID-19 nosocomial infections was emphasized, along with factors contributing to outbreaks in healthcare settings. Recommendations were made to address issues such as maintaining cleanliness, staff behaviors, PPE usage, workforce management, testing protocols, and patient factors. Attendees were encouraged to participate in Q&A sessions and utilize the chat function during the presentation.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
RR/App_BOD 32(i)/2020 (Agenda item: 32) Mental Health Update on IPC, prevention of nosocomial infections, staff flu vaccine and rapid testing 20thNovember 2020 NHS England and NHS Improvement
Welcome Please remain muted throughout the presentation. We invite you to UNMUTE yourselves during the Q&A part. Please use the CHAT function throughout to ask us questions and provide comments/ input, and we will try to respond to them all. Any queries you have after the meeting, please contact the team: england.mentalhealthpmo@nhs.net 2 |
Agenda Timing 12pm -12.05 Topic Introduction Speaker Claire Murdoch, National Director for Mental Health, NHSE/I Pauline Philip, National Director for Emergency and Elective Care, NHSE/I 12.05-12.15 Update on staff flu vaccine and testing 12.15-12.25 Update on IPC and prevention of nosocomial infection Lisa Ritchie, Head of IPC, NHSE/I Sue Tranka Deputy CNO for Safety and Innovation, NHSE/I All 12.25-12.45 Q&A 3 |
Preventing Covid-19 Nosocomial (Healthcare Onset) Infections 20 November 2020 NHS England and NHS Improvement
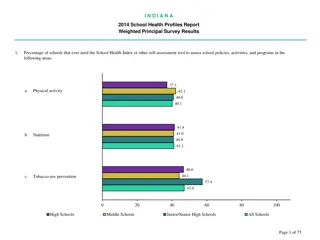
The daily data we collect shows that nosocomial infections are an issue in mental health trusts (data for 7 days up to 17 November) 5 |
Our work with NHS organisations has found a number of main outbreak provoking factors for the spread of COVID-19 in healthcare settings Estates Factors: Age of Estate; increased difficulty in maintaining bed spacing and maintaining cleanliness; air changes/ ventilation Staff social behaviours: Poor social distancing in & out of work; car sharing; unclear understanding of COVID secure Use of PPE: High level of fatigue and apathy with staff, observed not to follow PPE guidelines regarding how to wear and use PPE. Workforce: HCWs attending work with minor COVID symptoms and subsequently confirmed positive; Test and Trace system advice; A general reduction in IPC capacity, knowledge and competence across organisations; IPC influence at Board level Testing and Diagnostic Factors: unclearreporting definitions; inconsistency with testing at day 5-7; turnaround times of specimens; not considering COVID-19 symptoms as a differential diagnosis Patient Factors: COVID complacency as in hospital not wearing facemasks and not maintaining 2m social distance to each other patients with dementia who walk with purpose Other factors: cleaning of non-clinical areas; Shared equipment not always in a good state of repair. 6 |
Recent actions and our next steps are focused on supporting trusts to deliver reductions in nosocomial infections Further steps we are taking What we are doing now Additional testing on day 3 after admission (as well as on admission and day 5-7) to ensure infections are identified early to stop spread. Communication with trusts of actions to take to reduce nosocomial infections. Strengthen process of surveillance and systems: On-site IPC and panel support being provided to the North West and South East Shared learning from HOCI/ outbreak deep dive Development of national comms infographic with behavioural science to support healthcare staff (based on findings from HOCI deep dive) Focused IPC sessions for Matrons; collaboration between National IPC Team and Matrons network Webinars/workshops with regional leads e.g. IPC, Chief Nurses, Medical Directors, on importance of HOCI data collection and accuracy of reporting Board Assurance Framework and checklists revised in line with IPC guidance and HOCI data collection requirements Collaboration with specific specialties/ royal colleges in IPC guidance implementation Review and encourage clear governance structures and executive engagement with IPC o Review and produce clarity on definition of specimen collection specifically between day 5-7 o Guidance to support staff for ongoing patient screening following a positive result o Audit of data capture locally, regionally and nationally Continue to strengthen and develop IPC shared systems with the regional IPC leads, as part of building a strong and sustainable IPC workforce Development of further bespoke IPC training for matrons Support implementation of the National Standards for Cleanliness when published 7 |
To support providers, we have published ten key actions on infection prevention and control and testing Organisations 8. Patient testing: It is the board s responsibility to ensure that: a. All patients must be tested at emergency admission, whether or not they have symptoms. 1. Staff consistently practice good hand hygiene and all high touch surfaces and items are decontaminated multiple times every day once or twice a day is insufficient. b. Those with symptoms of COVID-19 must be retested at the point symptoms arise after admission. 2. Staff maintain social distancing in the workplace, when travelling to work (including avoiding car sharing) and to remind staff to follow public health guidance outside of the workplace. c. Those who test negative upon admission must have a second test 3 days after admission, and a third test 5-7 days post admission. 3. Staff wear the right level of PPE when in clinical settings, including use of face masks in non-clinical settings. d. All patients must be tested 48 hours prior to discharge directly to a care home and must only be discharged when their test result is available. Care home patients testing positive can only be discharged to CQC-designated facilities. Care homes must not accept discharged patients unless they have that person s test result and can safely care for them. 4. Patients are not moved until at least two negative test results are obtained, unless clinically justified. 5. Daily data submissions have been signed off by the Chief Executive, the Medical Director or the Chief Nurse, and the Board Assurance Framework is reviewed and evidence of reviews is available. e. Elective patient testing must happen within 3 days before admission and patients must be asked to self-isolate from the day of the test until the day of admission. 6. Where bays with high numbers of beds are in use, these must be risk assessed, and where 2m can t be achieved, physical segregation of patients is considered, and wards are effectively ventilated. Systems 7. Staff testing: Local systems must: a. Twice weekly lateral flow antigen testing for NHS patient facing staff is implemented. Whilst lateral flow technology is the main mechanism for staff testing, this can continue to be used alongside PCR and LAMP testing. 9. Assure themselves, with commissioners, that a trust s infection prevention and control interventions (IPC) are optimal, the Board Assurance Framework is complete, and agreed action plans are being delivered. b. If your trust has a high nosocomial rate you should undertake additional targeted testing of all NHS staff, as recommended by your local and regional infection prevention and control team. Such cases must be appropriately recorded, managed and reported back. 10. Review system performance and data; offer peer support and take steps to intervene as required. 8 |
Specific COVID Guidelines for mental health, learning disabilities and autism are due to be published shortly The Guidelines developed with professional leads Key Highlights: Information all in one place on GOV.UK Personal protective equipment use in mental health settings including use in restraint Screening definitions for mental health settings including ward leave scenarios Examples of COVID pathways for mental health settings Application of transmission based precautions for mental health settings 9 |
Discussion and Q&A 10 |