Effective Equipment Management in Medical Radiological Practices
This presentation focuses on key aspects of managing medical equipment within a Quality Management System in radiological practices. It covers topics such as the importance of quality, roles and responsibilities, equipment procurement procedures, and developing a successful Equipment Management System. Technical and non-technical stakeholders can learn how to ensure effective equipment management for improved performance and safety.
Uploaded on Oct 01, 2024 | 0 Views
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
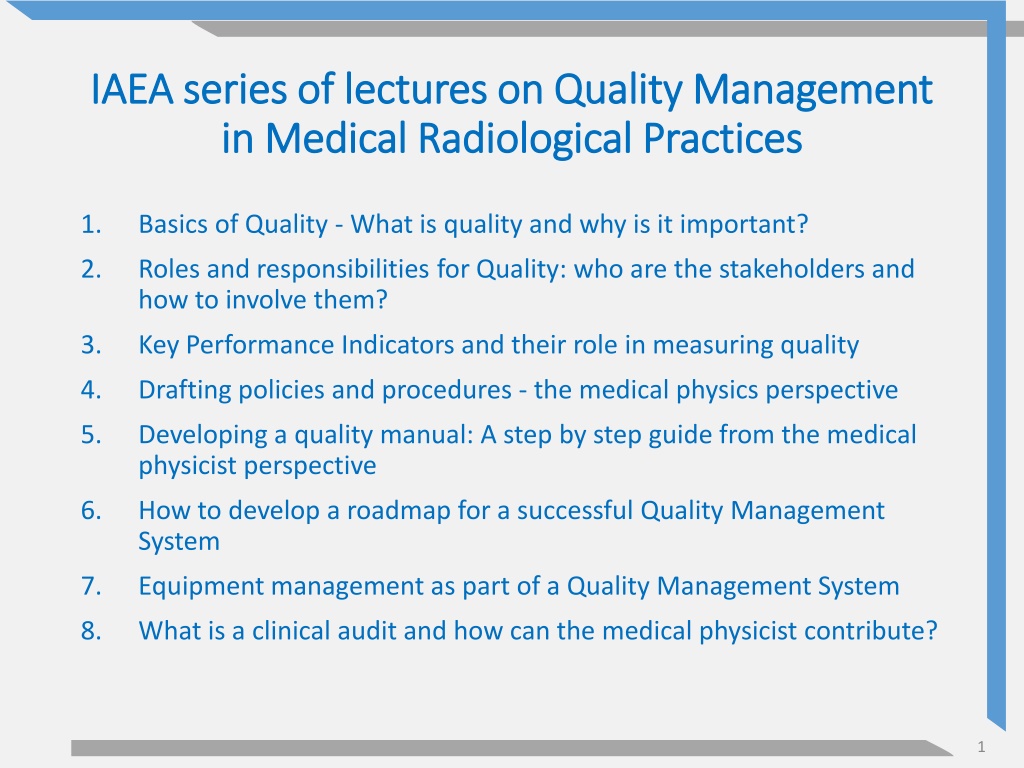
IAEA series of lectures on Quality Management IAEA series of lectures on Quality Management in Medical Radiological Practices in Medical Radiological Practices 1. Basics of Quality - What is quality and why is it important? 2. Roles and responsibilities for Quality: who are the stakeholders and how to involve them? 3. Key Performance Indicators and their role in measuring quality 4. Drafting policies and procedures - the medical physics perspective 5. Developing a quality manual: A step by step guide from the medical physicist perspective 6. How to develop a roadmap for a successful Quality Management System 7. Equipment management as part of a Quality Management System 8. What is a clinical audit and how can the medical physicist contribute? 1
Equipment management as part of a Quality Management System Quality Management in Medical Radiological Practices (Diagnostic Radiology, Nuclear Medicine and Radiotherapy) 2
Objectives The objectives of this presentation are to: learn how to manage medical equipment as part of the Quality Management System understand the process with which to support use of equipment documentation using appropriate
Content What are the key properties of an equipment management system for medical radiological practices? How can a medical radiological practice develop an appropriate equipment management system? How can we monitor the equipment management system and ensure it is effective? 4
Content focus This presentation can be used by both technical and non-technical stakeholders of medical radiological practices to recognize the key elements of an effective equipment management system. The focus is on the management system rather than on the technical implementation of equipment performance and safety assessment. direct hit by OpenMoji Emoji Set is licensed under CC BY 4.0 5
Procurement procedure Equipment management starts by the medical radiological practice having in place a procedure explaining how it: Identifies requirements for new equipment; Prioritises equipment needs; Evaluates options offered by vendors; Decides on equipment to be purchased. 6
Procurement procedure example 1. Within each financial/funding cycle, there is a callout to all practice s technical and clinical leads to identify new equipment needs; 2. The leads submit their ideas for new equipment, supported by evidence e.g. in the form of risk assessments or Key Performance Indicators (KPIs); 3. The quality and safety committee reviews submissions and prioritises equipment, based on needs and budget; 7
Procurement procedure example 4. The quality and safety committee prepares a procurement plan, which is submitted to the financial department for approval; 5. The quality and safety committee asks subject- matter experts to prepare a statement of requirements for equipment to be purchased; 6. The statement of requirements is sent to equipment vendors who respond with offers, which are reviewed by the committee and experts to reach a procurement decision; 8
Statement of requirements The content of the statement of requirements for new equipment would be a reflection of the commitment of the medical radiological practice to the overall quality management system. Content of Statement of Requirements Equipment must meet the quality and safety improvement targets of the practice. Advanced Equipment must meet the specific clinical needs of the practice. Equipment must have FDA and CE approval. Basic 9
Equipment inventory As part of quality management, the medical radiological practice must prepare an inventory including equipment used in the examination and therapy of patients. The inventory should include identifiers (manufacturer, model number and serial number) for equipment and key components, for example image/radiation detectors and X ray tubes. Where applicable, the inventory would also include the software version used by the equipment. 10
Pause and Ponder What is the process of updating the equipment inventory at your medical radiological practice? Who is responsible and how often is it updated? 11
Equipment servicing Preventive maintenance is the proactive servicing of equipment, which may include cleaning, lubrication, adjustments, repairs, part replacements and software upgrades. Preventive maintenance can prevent equipment downtime and could prolong the lifetime of equipment. The medical radiological practice should have a preventive maintenance plan, which would include the annual servicing schedule and the process of record-keeping for servicing reports. 12
Equipment testing There are different levels of testing the performance and safety features of equipment, each with its own purpose and referred to as: Critical examination; Acceptance testing; Commissioning; Routine testing (constancy or quality control). Note that testing of safety features would also typically include audits of the space/area within which the equipment has been installed. 13
Equipment testing and IAEA IAEA literature provides guidance on what could be included in each level of performance and safety testing and for each modality, for example: Nuclear Medicine Physics Handbook; Diagnostic Radiology Physics Handbook; Radiation Oncology Physics Handbook. 14
Responsibility for testing An important part of equipment management would be to identify who is responsible for testing and validating that equipment meets performance and safety requirements, especially when the equipment first enters clinical use. The responsibility may be determined by legislative or accreditation requirements but, in their absence, the medical radiological practice needs to consider availability of expertise and best practice guidelines. 15
Pause and Ponder At your medical radiological practice, is equipment signed-off as suitable for clinical use by the vendor/installer or by an independent expert assessor? 16
Quality control manual Medical radiological practices should have a quality control manual to describe, as a minimum, routine testing of equipment, including: Frequency and methodology of testing; Responsibility for testing; Action levels. Although generic testing protocols from external sources can be used as references, it is advisable that each practice develops their manual taking into account specific considerations of equipment and installation area. 17
Additional documentation Work instructions and checklists would also be used to support testing and quality management of equipment. 18
Action levels Results from each test would be compared against appropriate action levels, corresponding to performance thresholds. Action levels may be values or conditions (e.g. no artefacts), referred to as: Remedial levels: benchmarks for optimal performance; Suspension levels: benchmarks for acceptable performance. Achievable, optimal performance Acceptable but sub-optimal performance Non-acceptable performance 19
Action levels Based on these action levels: Equipment operating above remedial level would be suitable for clinical use. Equipment operating below remedial level, but above suspension level, would be suitable for clinical use but would require calibration or monitoring to ensure that its performance can improve or does not deteriorate further. Equipment operating below suspension level would not be suitable for clinical use. 20
Action levels example In measuring the accuracy of kVp in general radiography equipment, the following action levels can be adopted: Remedial level: 5 kVp; Suspension level: 10 kVp. If results from tests indicate that measured and indicated kVp values differ by a maximum of 7 kVp, then the equipment can be used clinically but the engineer would need to examine and, if possible, correct the reason for deviation, at the earliest opportunity. 21
Action levels sources The medical radiological service can adopt suitable action levels recommended by: International guidelines and standards, e.g. by the IAEA or the International Electro technical Committee (IEC); National standards, e.g. by the National Electrical Manufacturers Association (NEMA) in the USA; National regulations on equipment performance requirements; Recommendations by professional societies, e.g. the American College of Radiology (ACR) or the Institute of Physics and Engineering in Medicine (IPEM); Specifications provided by the equipment manufacturer. In some cases, the practice could also use action levels based on published research or local performance baselines. 22
Pause and Ponder Which standards of equipment testing are used at your medical radiological practice? How do your action levels compare to those of other standards? 23
Record keeping procedure There should be documented evidence of any equipment testing, indicating in each case: The type of test performed (critical examination, acceptance, commissioning or routine); The date of testing; The results against the action levels; Comments and recommendations. The medical radiological practice should have a procedure stating the responsibility for record keeping and the length of time that the reports should be maintained. 24
Response procedure The medical radiological practice must have a procedure describing the response when equipment is found to fail remedial or suspension levels: How are all users notified of equipment performance issues? How is equipment taken out of clinical use? How are performance issues escalated to equipment engineers? What is the contingency plan to ensure continuity of clinical service whilst the equipment cannot be used? After the equipment is repaired, who gets notified of the work undertaken so that the practice can test and confirm that the equipment is suitable to re-enter clinical use? 25
Performance notification example Example Hospital Example Hospital QC PASSED DO NOT USE Equipment CT scanner room 4 Equipment CT scanner room 4 Reported by: Anna Hayes Tested by: John Smith Date: 31/03/2018 Date: 09/10/2019 Reporting reference DATIX 1234 Due date: 09/10/2020 Do not remove label Do not remove label 26
Pause and Ponder At your medical radiological practice, how would you know if your equipment has passed its routine testing or if there are any issues with its performance? 27
Equipment management KPIs Medical radiological practices should also monitor Key Performance Indicators (KPIs) related to equipment management, for example: Delays between due and scheduled dates of annual quality control or preventive maintenance; Percentage of days equipment is in clinical use without having passed daily quality control testing; Equipment downtime; Engineer response times when equipment is reported faulty. 28
Testing tools Testing the performance and safety features of equipment will only be effective if suitable tools are available, including testing equipment (e.g. phantoms and dosimeters) and, where required, analysis software. Regular calibration of testing equipment would need to be considered. Medical radiological practices must ensure that testing tools are appropriate for the generation of the equipment technology to be tested. 29
Pause and Ponder When new equipment is bought by your medical radiological practice, is there consideration for any new testing tools that will be required to monitor its performance? 30
Summary Medical radiological practices must ensure that they have a comprehensive equipment management system in place. Equipment management should encompass the whole equipment lifecycle and not limit itself to testing the performance and safety features of equipment. Equipment management should be supported with appropriate documentation (e.g. procedures and manuals) and monitored with suitable KPIs. 31
Resources and references INTERNATIONAL ATOMIC ENERGY AGENCY, Nuclear Medicine Physics, Non-serial Publications, 2015 INTERNATIONAL ATOMIC ENERGY AGENCY, Diagnostic Radiology Physics, Non-serial Publications, 2014 INTERNATIONAL ATOMIC ENERGY AGENCY, Radiation Oncology Physics, Non-serial Publications, 2005 32