Vascular Team Approach in Unstable Angina with Complex Vascular Disease
A 73-year-old patient with COPD, hypertension, and hyperlipidemia presents with severe lower extremity ischemia, leading to a plan for urgent aorto-bifemoral bypass. The clinical examination and test results revealed critical limb ischemia and extensive vascular disease requiring intervention from cardiology and vascular teams for risk optimization and treatment. The patient's complex condition necessitates a multidisciplinary approach for management.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Vascular Team Approach in a patient with Unstable Angina due to ULMCA disease, Bilateral Subclavian Stenosis and Limb Threatening Lower Extremity Ischemia dependent on Winslow s pathway Mariam Baig, MD; Maryna Popp, DO; Hassan Alkhawam, MD; Emad Zakhary, MD; Kartik Mani, MD FSCAI* . John Cochran VA Medical Center, St. Louis MO *Washington University St. Louis MO
Disclosures The presenter has no financial disclosures with one or more organizations that could be perceived as a real or apparent conflict of interest in the context of the subject of this presentation K.Mani MD FSCAI : VA Employee. Current research funding: NIH NIDDK P30 DK020579 Investigator, ECLIPSE trial (CSI Medical) Co-investigator, BEST CLI (NIH) Co-investigator, CREST-2 (NIH)
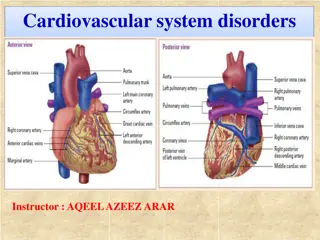
Clinical Presentation 73/M with a history of COPD/HTN/HLP and no known prior CADpresenting to vascular surgery with cold feet and severe bilateral buttock, thigh, calf and instep cramping with minimal activity. Occasional rest pain. No ulcers Physical exam notable for pulseless and cool lower extremities with delayed capillary refill, with hair loss and skin atrophy consistent with PAD.
Test results Ankle-brachial index : Right - 0.45 (toe prs 24 mmHg) ; Left - 0.35 (toe prs 17 mmHg) CT angiogram: Infra-renal aortic occlusion extending to bilateral external iliac arteries. Reconstitution in the CFA bilaterally via Inf. epigastric A collaterals and weak hypogastric collateralization Infrainguinal vessels patent with moderate femoral popliteal and tibioperoneal disease. Moderate vascular calcification in distal vascular tree limits exam.
Plan Plan for urgent aorto-bifemoral bypass due to evidence of critical limb ischemia on ABI with clinical examination evidence of poor perfusion. Referred to anesthesia for pre-operative evaluation During routine pre-operative evaluation, patient reports substernal chest pressure with minimal activity Resting EKG shows LVH with marked ST abnormalities Referred to cardiology/vascular team clinic for pre- operative risk optimization
Cardiology/Vascular Team Clinic Findings Echocardiogram demonstrated normal biventricular systolic function and grade II diastolic dysfunction Vascular surgery clinic exam findings confirmed, but in addition, patient noted to have bilateral carotid and supraclavicular bruits Bilateral radial pulses somewhat diminished, right side markedly so. No evidence of prior digital ulceration or atrophy. Given abnormal baseline EKG, marked angina with very low activity and high risk surgery planned, decision taken to proceed directly to cardiac cath. Radial approach (usual practice) emphasized due to aortic occlusion.
Cardiac catheterization Thready radial pulse noted. Bilateral wrists prepped 5F Slender radial sheath used for radial access with ultrasound guidance per routine. Patient fully heparinized per routine. Wire noted to arrest in the RSCA. Support 5F JR4 Convey guide advanced over J wire into RSCA for angiographic evaluation. CTO RSCA with atretic RIMA and severe ostial R Vert. A lesion. Lesion probed with a Grand Slam guidewire and noted to traverse the lesion with some manipulation.
Cardiac catheterization 5f JR4 guide advanced into aorta to perform left heart catheterization for LVEDP and RCA angiogram (not shown). Moderate 60% tandem lesions and diffuse disease in RCA. 5F RBL4 guide used for LCA angio (shown). Heavily calcified proximal vessels LMCA 40% ostial, 70% distal LMCA LAD 70% ostial, 80% proximal LCx 80% proximal, 80% mid Ramus Marginalis 80% proximal LSCA cannulated with RBL4 guide and selective angio shows severe proximal LSCA stenosis (30 mmHg gradient) with 8mm LIMA
Now what? Elderly patient with advanced COPD with CLI (Rest pain with poor limb perfusion without tissue loss) due to abdominal aortic occlusion Severe bilateral subclavian disease (right CTO, left severe with large LIMA consistent with Artery of Winslow physiology) CCS4 angina with distal LMCA trifurcation, proximal LAD, circ and ramus disease with moderate RCA disease. Normal LV function.
Team discussion : Anesthesia, Vascular, CT surgery and Int. Cardiology Medical management of CLI/CAD likely fatal from both (Cardiology/Anesth). Aortobifem surgery (Vascular) for management of CLI with preop ? Medical therapy alone ? CABG for ULMCA disease (CT surgery) ? conduits (occluded RSCA/atretic RIMA, severe LSCA disease with LIMA to LEIA collaterals maintain LE viability) ? Aortic cross clamping ? ULMCA PCI (Interventional Cardiology) ?Single or multiple stent approach ?Hemodynamic support ?Atherectomy ?Access right or left radial - ?potential for LE arterial compromise if LSCA compromised ?RSCA stent/PTA
Decision Not a candidate for medical optimization for high risk vascular surgery Patient evaluated and turned down by two different cardiac surgical teams due to inability to use LIMA/RIMA and aortic cross clamp with prohibitive risk of postoperative vascular complications. Given absence of acute tissue loss, plan for preoperative ULMCA PCI with use of minimal stents with close post PCI monitoring for worsening LE ischemia or tissue loss. Planned for elective aortibifem after 6 mo. of DAPT or as needed for worsened ischemia
Interventional cardiology planning No large bore access feasible given bilateral subclavian disease. Severe emphysema excluded thoracotomy for aortic access. Plan right radial attempt and re-cross CTO with PVI of the RSCA 7F slender radial access to allow for bifurcation PCI of ULMCA Bilateral wrists prepped for alternative access. No hemodynamic support planned due to access issues. Procedural risk reviewed with patient and family.
Cardiac Catheterization Ultrasound guided access obtained in right radial 7Fr. Slender Radial sheath placed Right subclavian CTO was crossed using a support catheter and Grand Slam guidewire
Cardiac Catheterization 7F RBL4 guide placed 3 guidewires placed in LAD/LCX/Ramus ELCA performed at 80/80 from LMCA into LCX (given ability to retain SB guidewires during atherectomy) followed by PTCA only of the proximal LCx (not the mid lesion) Following PTCA of LCx, 3.5 x28 mm SYNERGY DES placed from LMCA to LAD with trapped wires (rewired after PCI) Impaired flow noted in Ramus after guidewire removal following post dilation of LMCA/LAD stent. Ramus re-crossed with Fielder FC guidewire and flow reestablished with SKB Final IVUS in all three limbs showed good stent apposition and expansion
Cardiac Catheterization 7F RBL4 guide was withdrawn over a grand slam guidewire into the axillary artery. Volcano PV visions 0.018 IVUS was used to size the subclavian artery (7mm) Vessel was directly stented with an 8x27 mm balloon expandable stent. Post IVUS showed increase in vessel size post PVI with increasing flow requiring PTA with a 9 mm balloon and some residual, non-flow limiting dissection. Very strong brachial pulse noted after device withdrawal.
Follow Up Monthly clinical follow-up was performed for 6 months with DAPT (ASA/Clopidogrel) with both Vascular Surgery and Cardiology Significant improvement in right sided pulses noted CCS1 angina following procedure noted to increase in month 3 to CCS2. Given LMCA stent and recurrent angina, left TRA performed showing patent LMCA stent as well as atherectomy and PTCA treated lesions in LCx and Ramus with stable residual mid LCx (untreated) disease Stent in RSCA widely patent with a very large RIMA noted 30mm translesional gradient stable in LSCA with LIMA to LEIA collaterals (artery of winslow) on selective angiography.
Follow Up Patient underwent aorto-bifem at 6 months after stopping clopidogrel but continuing ASA No postoperative cardiovascular issues noted without inordinate bleeding issues. Discharged home in 3 weeks, after post op rehab following hospital stay for post op ileus. Stable at 30 day follow-up after surgery
Take home points Severe PAD masks severe CAD and vice versa LE PAD is often associated with UE PAD Team based approach i.e. trust rather than competition between IC/CTS/Vasc sx is critical for good outcomes Being comfortable with endovascular approaches is key to good interventional cardiology procedures Not every ULMCA needs hemodynamic support Minimize stents in preop patients by limiting this to the LM and LAD ELCA and PTCA alone when done carefully result in stable lumen gain Sometimes, when things don t look perfect, the absence of symptoms and presence of good flow predicts good outcomes. Being comfortable to optimal radial approaches is key in these complex patients.
Questions? Email: mariam.baig@health.slu.edu