Utilizing ISBAR for Effective Clinical Communication
ISBAR is a standardized communication tool used in clinical settings to enhance communication skills during handovers and referrals. It helps in identifying the situation, background, assessment, and recommendations effectively. This tool aids in standardizing communication practices and is widely used in healthcare facilities to improve patient care outcomes.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
ISBAR ISBAR Using a standardised communication tool for clinical handover
What is ISBAR? Helps develop clinical communication skills Utilises these skills when making a telephone referral or handover Utilises questioning / prompting skills when receiving a telephone referral or handover Uses a standardised or common approach to communication Adapted from SBAR, a tool developed by the US Navy to improve communication In use in SA Health and hospitals/ambulance staff and nationally/internationally, so helps standardise communication
ISBAR tool I - IDENTIFY S - SITUATION B - BACKGROUND A - ASSESSMENT R - RECOMMENDATIONS
I - Identify Who you are Eg: I am the Registered Nurse and I am in charge here at the moment. I have known the resident for 3 weeks/2 years etc. I am the Enrolled Nurse for this wing and have been looking after x this morning I am a carer who knows x well and have concerns about his condition (on the phone) I am a Registered Nurse from Ananda Aged Care (Findon or HV) looking after X
I - Identify Who the resident is: Use a minimum of 3 forms of identification e.g. - Name/Age/Diagnosis (or Main medical background) And preferably: - Who is the GP and are they aware of the situation? - Who is the family/Substitute Decision Maker etc, and are they aware of the situation? - Plus social background if known
I IDENTIFY examples Doris, likes to be called Peggy, is an 81 year old married lady, who has mild dementia, severe COPD needing oxygen, heart failure, mobile with frame, and has been at Ananda 3 weeks on respite care. Her GP is Dr Smith who is not answering calls, her family are Leslie and Fred who are here now. Bill, is a 91 year old with Alzheimer s Disease which makes him very forgetful of short term things, occasional responsive behaviours eg wandering/trying to elope, chronic pain from osteoarthritis, gout and is very active and mobile. He has no family we know and his GP, Dr Smith has asked for us to call an ambulance for urgent review of
S - SITUATION What is going on? If urgent, make this clear at the start What are you ringing, asking about? What has made you think help is needed? What do you need staff following you to be aware of and watch out for and why? What do you want the other person to do advise me, help me come now!!! Know the situation .have the observations, medical background, medication history has a medication been missed etc?
S SITUATION examples I am calling you to attend a resident, Mr Jones. He is a 56 year old man, who came back to Ananda 3 days post total knee replacement who has developed tachycardia/a fast heart with a blood pressure of 105/66. He looks pale and feels unwell. I would like you to come and assess this patient please as I am concerned he is medically unstable. He is not for CPR in the event of cardiac arrest. Can you please monitor Emily closely overnight, she is a 72 year old resident who was admitted from hospital yesterday and her observations are fine (BP 120/80, HR 77 regular, SpO2 99% on room air) though she looks pale and appears mildly confused. This appears new for her and I d like you to check her hourly, document and respond to any changes overnight. Dr Smith is aware and says ring him if any changes in vital signs or call ambulance if concerned. She is for CPR in the event of cardiac arrest.
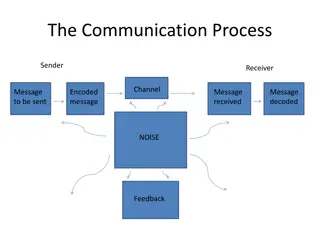
B - BACKGROUND Tell the story Say I ll tell you the story I ll give you the background information Provide RELEVANT information only. Deciding what is relevant is a skill that comes with experience Don t forget less is often more you may get the message across better with less information Include aspects of history, examination, investigations and management where relevant Have the details to hand, be clear what it is you are asking for especially via phone, they cannot see what s gone on
A- ASSESSMENT State what you think is going on. Give your interpretation of the situation This is NOT about providing your diagnosis of the patient only a qualified medical practitioner can do this Don t leave the receiver to guess what you are thinking - Stating the obvious is helpful here - Include your degree of certainty ( I think that This happened before and what happened was ., - Be objective (facts rather than guesses)
A- ASSESSMENT the resident is febrile with a temperature of 39 degrees Celsius The resident has improved but I am concerned they are still short of breath The resident has rated their pain at 8/10 despite 2.5 mg Morphine one hour ago Their observations are stable in their normal range but their cognitive ability has changed, they are more confused than is normal for them and they have slightly slurred speech, which is new. Have all clinical information ready and documented wherever possible
R RECOMMEND/REQUEST State what you want from the receiver We would be grateful for your opinion regarding the need for transfer I need help urgently, are you able to come now? if not, who should I call? Ask questions What would be the most appropriate pain relief we can administer until you are able to come and assess the resident? What would you like ., what tests, what action etc I suggest we do this, and if this happened we do that
FINALLY What you say for Situation may be a concise summary of what you say for Assessment and Request. This repetition is helpful, as it emphasises the key purpose of the referral, as well as why it is important they come NOW! Sometimes the receiver will lead the conversation you can still use ISBAR as a guide Don t forget, the receiver may not be familiar with ISBAR Practice makes perfect use the ISBAR documentation form to help you organise the information you are going to convey At the end of any handover or referral, especially by phone check the other person understands and you are agreed what is going to happen: So just to clarify and so a second nurse can hear: you do not want me to call an ambulance, you want us to give 2.5mg morphine stat, apply 2L/minute nasal oxygen and repeat the obs, including a BGL and urine if we an get it? We will call the family immediately and you will come in asap to review the resident?
SUMMARY OF ISBAR STEPS Identify - Yourself and role / Resident with three identifiers Situation - What is going on with the patient? Background - What is the clinical background/context? Assessment - What do I think the problem is? Recommendation - What do I recommend? What do I request? Check back for shared understanding Assign and accept responsibility/accountability