Understanding Uterine Diseases: Endometritis and Adenomyosis
Exploring diseases of the uterus such as endometritis and adenomyosis. Endometritis may result from retained products of conception or foreign bodies, leading to acute or chronic inflammation. Adenomyosis involves the invagination of endometrial tissue into the myometrium, causing hypertrophy. Learn about the symptoms, diagnosis, and implications of these conditions.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Body of uterus LEC.2 .
Learning objectives: Discuss diseases of the uterus like endometritis,adenomyosis,endometriosis Endometrial hyperplasia&there types Tumors of the endometrium&myometrium Diseases of pregnancy like H.mole,invasive mole&choriocarcinoma
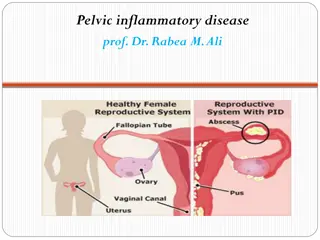
BODY OF UTERUS Endometritis This may be associated with retained products of conception subsequent to miscarriage or delivery, or a foreign body such as an intrauterine device.
Retained tissues or foreign bodies act as a nidus for infection, frequently by flora ascending from the vaginal or anal region. Endometritis is either acute or chronic depending on whether there is a predominant neutrophilic or lymphoplasmacytic response; however, components of both may be present in otherwise normal endometrium.
Generally the diagnosis of chronic endometritis requires the presence of plasma cells . Acute endometritis is frequently due to N. gonorrhoeae or C. trachomatis. Microscopically, neutrophilic infiltrate in the superficial endometrium and glands coexists with a stromal lymphoplasmacytic infiltrate.
Chronic endometritis There is a large number of plasma cells (arrows).
All forms of endometritis may present with menstrual abnormalities, infertility and ectopic pregnancy due to extension of the damaging inflammation to the fallopian tubes.Occasionally tuberculosis may present as granulomatous endometritis, frequently with tuberculous salpingitis and peritonitis.
Adenomyosis This refers to the invagination of the stratum basalis of endometrium down into the myometrium. Nests of endometrial stroma, glands, or both, are found well down in the myometrium between the muscle bundles. The latter become hypertrophied.
Accordingly, the uterine wall often becomes thickened and the uterus is enlarged and globular. Because these glands derive from the stratum basalis, they do not undergo cyclical bleeding. Nevertheless, marked adenomyosis may produce menorrhagia, dysmenorrhea, and pelvic pain before the onset of menstruation.
Adenomyosis uterus Gross appearance of uterus involved by adenomyosis. The wall is irregularly thickened and contains small hemorrhagic foci (arrow). The thickened and spongy appearing myometrial wall of this sectioned uterus is typical of adenomyosis. There is also a small white leiomyoma at the top
Adenomyosis uterus Adenomyosis occurs when endometrial glands and stroma are found in the myometrium.
Endometriosis This is characterized by the presence of endometrial glands and stroma in a location outside the endomyometrium. It occurs in as many as 10% of women in their reproductive years and in nearly half of women with infertility. It may present as a pelvic mass filled with degenerating blood (chocolate cyst).
It is frequently multifocal and may involve any tissue in the pelvis (ovaries, pouch of Douglas, uterine ligaments, tubes, and rectovaginal septum), less frequently in more remote sites of the peritoneal cavity and about the umbilicus. Three possibilities have been suggested to explain the origin of these lesions.
1. The regurgitation theory, currently the most accepted, proposes menstrual backflow through the fallopian tubes with subsequent implantation. 2. The metaplastic theory proposes endometrial differentiation of coelomic epithelium. 3. The vascular or lymphatic dissemination theory has been raised to explain extrapelvic endometriosis.
Gross features Endometriosis almost always contains functioning endometrium, which undergoes cyclic bleeding. Because blood collects in these ectopic foci, they usually appear grossly as red-blue to yellow- brown nodules. They vary in size from microscopic up to 2 cm in diameter and lie on or just under the affected serosal surface. Often individual lesions coalesce to form larger masses.
When the ovaries are involved, the lesions may form large, blood-filled cysts that are transformed into so-called chocolate cysts as the blood ages . Seepage and organization of the blood leads to widespread fibrosis, adherence of pelvic structures, sealing of the tubal fimbriated ends, and distortion of the oviducts and ovaries.
Endometriosis ovary This is a section through an enlarnged 12 cm ovary to demonstrate a cystic cavity filled with old blood typical for endometriosis with formation of an endometriotic, or "chocolate", cyst. Inner surface of cyst in a case of ovarian endometriosis. The color is typically brown.
Endometriosis ovary Ovarianendometriosis In this area endometrial tissue faithfully reproduces the appearance of normal endometrium, in terms of both glands and stroma. Lt., collection of lipofuscin-laden histiocytes below the endometriotic epithelium.
Microscopic features The histologic diagnosis depends on finding two of the following three features within the lesions: 1. Endometrial glands. 2. Endometrial stroma, or 3. Hemosiderin pigment. Extensive scarring of the oviducts and ovaries often causes sterility.
Pain on defecationreflects rectal wall involvement, and dyspareunia (painful intercourse) and dysuria reflect involvement of the uterine and bladder serosa, respectively. In almost all cases, there is severe dysmenorrhea and pelvic pain as a result of intrapelvic bleeding and periuterine adhesions.
Endometrial Hyperplasia This is an exaggerated endometrial proliferation induced by sufficiently prolonged excess of estrogen relative to progestin. The severity of hyperplasia is classified according to two parameters:- a. architectural crowding of the glands & b. cytologic atypia. Accordingly there are three categories:- 1. Simple hyperplasia. 2. Complex hyperplasia. 3. Atypical hyperplasia.
These three categories represent a spectrum based on the level and duration of the estrogen excess. The risk of developing carcinoma depends on the severity of the hyperplastic changes and associated cellular atypia. Simple hyperplasia carries a negligible risk, while a woman with atypical hyperplasia has a 20% risk of developing endometrial carcinoma. Thus When atypical hyperplasia is discovered, it must be carefully evaluated for the presence of cancer and must be monitored by repeated endometrial biopsy. Any estrogen excess may lead to hyperplasia.
Potential contributors include:- 1. Failure of ovulation, e.g. around the menopause. 2. Prolonged administration of estrogenic steroids. 3. Estrogen-producing ovarian lesions such as a. polycystic ovaries (Stein-Leventhal syndrome). b. cortical stromal hyperplasia. c. granulosa-theca cell tumors of the ovary. 4. Obesity, because adipose tissue processes steroid precursors into estrogens.
Gross features In simple hyperplasia the endometrium is diffusely thickened. In complex & atypical hyperplasia there is usually focal thickening of the endometrium. Microscopic features Simple hyperplasia involves both the glands & stroma; the normal gland to stroma ratio is maintained. The glands are proliferative and some are cystically dilated. Complex hyperplasia: there is glandular crowding with little stroma separating the proliferative glands. Typically, this is a focal process.
Simple and complex hyperplasias are further divided into atypical and non-atypical Atypical hyperplasia: characterized by atypical nuclei of the proliferative glands as evidenced by nuclear stratification, nuclear rounding and the presence of nucleoli.
Diffuse endometrial hyperplasia The prominent folds of endometrium in this uterus (opened to reveal the endometrial cavity) are an example of hyperplasia. The hyperplasia involves both endometrial glands and stroma.
Complex endometrial hyperplasia without atypia Glands are lined
Atypical endometrial hyperplasia Nuclear and cytoplasmic differences are present between atypical glands (upper Rt.) and residual normal endometrial glands (center).
Tumors of the Endometrium and Myometrium The most common neoplasms of the body of the uterus are:- 1. Endometrial polyps, 2. Smooth muscle tumors, and 3. Endometrial carcinomas. All tend to produce bleeding from the uterus as the earliest manifestation.
Endometrial Polyps are usually sessile, hemispheric lesions up to 3 cm in diameter. Larger polyps tend to be pedunculated & may project from the endometrial mucosa into the uterine cavity & sometimes through the cervix into the vagina. Microscopically, they are composed of basalis-type, often cystically dilated glands with a rather fibroblastic stroma. Small muscular arteries are often prominent.
Endometrial polyp The uterus has been opened anteriorly through cervix and into the endometrial cavity. High in the fundus and projecting into the endometrial cavity is a small endometrial polyp. Such benign polyps may cause uterine bleeding. Huge endometrial polyp filling the endometrial cavity. There is also a smaller polyp and
Endometrial polyp LP mic Cystically dilated glands and a fibrous stroma with thick-walled vessels.
Leiomyomas are benign tumors that arise from the smooth muscle cells in the myometrium. Because of their firmness they are also called fibroids. They are the most common benign tumor in femalesand are found in 30% to 50% of women during reproductive life. Estrogens and possibly oral contraceptives stimulate their growth; conversely, they shrink postmenopausally.
Gross features: They are sharply circumscribed, firm gray-white masses with a characteristic whorled cut surface. They may occur singly, but are often multiple tumors scattered within the uterus, ranging in size from small seedlings to massive neoplasms that dwarf the size of the uterus. Some are embedded within the myometrium (intramural), whereas others may lie directly beneath the endometrium (submucosal) or directly beneath the serosa (subserosal).
Leiomyomas uteri Markedly distorted uterine corpus with multiple irregular masses protruding from its surface. These are subserosal leiomyomata.
Larger neoplasms may show foci of ischemic necrosis with areas of hemorrhage and cystic softening (red degeneration). After menopause they may become densely collagenous and even calcified.
Microscopic features There are whorling bundles of smooth muscle cells. Foci of fibrosis, calcification, ischemic necrosis, cystic degeneration, and hemorrhage may be present. Leiomyomas of the uterus may be entirely asymptomatic and be discovered only on routine pelvic examination or imaging studies. The most frequent manifestation, when present, is menorrhagia. Large masses in the pelvic region may become palpable or may produce a dragging sensation. Benign leiomyomas rarely transform into sarcomas.
Leiomyoma uteri Here is the microscopic appearance of a benign leiomyoma. Normal myometrium is at the left, and the neoplasm is well- differentiated so that the leiomyoma at the right hardly appears different. Bundles of smooth muscle are interlacing in the tumor mass.
Endometrial Carcinoma (EMC) After the dramatic drop in the incidence of cervical carcinoma, EMC is currently the most frequent cancer occurring in the female genital tract. Epidemiology and Pathogenesis EMC appears most frequently around the age of 60 years. There are two clinico-pathological settings in which endometrial carcinomas arise: 1. In perimenopausal womenwith estrogen excess; these are of endometrioid type. 2. In older women with endometrial atrophy; these are of serous type.
Well-defined risk factors for endometrioid carcinoma include a. Obesity: associated with increased synthesis of estrogens in fat depots. b. Diabetes. c. Hypertension. d. Infertility: women tend to be nulliparous, often with anovulatory cycles. At least some of these risk factors point to increased estrogen stimulation, and indeed it is well recognized that prolonged estrogen replacement therapy and estrogen-secreting ovarian tumors increase the risk of this form of cancer.
Gross features EMC may be exophytic (fungating, polypoid) or infiltrative. Microscopic features The endometrioid carcinoma consists of malignant endometrial-like tubular glands of varying grades. Squamous metaplasia is frequent. Sometimes, the tumor is adeno-squamous carcinoma. Tumors originate in the mucosa and may infiltrate the myometrium and enter vascular spaces, with metastases to regional lymph nodes.
Serous carcinoma forms small tufts and papillary arrangements rather than the glands seen in endometrioid carcinoma, and has much greater cytologic atypia.They are particularly aggressive.
Endometrial adenocarcinoma The tumor shown is ) The tumor shown is extensive, nodular & highly infiltrating.
Endometrioid adenocarcinoma type, infiltrating myometrium and displaying cribriform architecture. B, Higher magnification reveals loss of polarity an
Serous carcinoma of the endometrium C, displaying formation of papillae and marked cytologic atypia. D, Immunohistochemical stain for p53 reveals accumulation of mutant p53 in serous carcinoma.
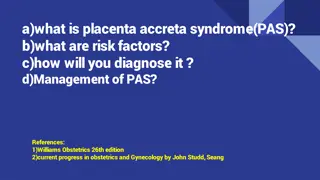
Diseases of pregnancy Gestational trophoblastic disease: 3 morphological categories: (1)Hydatidiform mole (H mole): Voluminous mass of swollen sometimes cystically dilated chorionic villi, appear grossly as grape like structure, It is of 2 subtypes: A: Complete mole: characterized by: *not permit embryogenesis & never contain fetal parts. * all chorionic villi are abnormal (hydropic changes--- cystic dilated).
the chorionic epith. cells are diploid (46XX or 46XY), it result from fertilization of empty egg by 2 sperms or diploid sperm. * Incidence of complete mole is much higher in Asian than Western countries, much more common before 20 & after 40yr. age, Clinically: painless vaginal bleeding 12-14week after conception, when discovered early by ultrasound, uterus may or may not be too large for date but no fetal parts or heart sounds present.
Lab test:increase HCG present in maternal blood & urine, when discovered in 4th month of gestation---uterine cavity filled with delicate friable masses of thin wall translucent cystic structures without fetal parts. Mic: hydropic swelling of villi & chorionic epithelia show some degree of proliferation of cyto & syncytial trophoblast .
Complete hydatidiform mole The grape-like villi of a hydatidiform mole are seen here suspended in saline. With molar pregnancy, the uterus is large for dates, but no fetus is present. HCG levels are markedly elevated. Patients with a hydatidiform mole are often large for dates and have hyperemesis gravidarum more frequently. Patients may present with bleeding, and may pass some of the grape-like villi.
Complete hydatidiform mole Histologically, the hydatidiform mole has large avascular villi and areas of trophoblastic proliferation. Of course, ultrasound confirms the diagnosis before currettage is done to evacuate this tissue seen here.