Understanding Patient Perspectives on Screening for Social Determinants of Health (SDOH) in Healthcare Settings
This project, led by Dr. Amy Huebschmann and shared by Dr. Emilia De Marchis and the UCSF SIREN group, explores the screening for Social Determinants of Health (SDOH) and offering assistance in healthcare settings from the patient's viewpoint. It delves into the acceptability of SDOH screenings to patients and caregivers, alongside the interest in social risk assistance in diverse healthcare settings. The study, funded by The Commonwealth Fund, sheds light on the importance of addressing social risks within healthcare systems caring for Medicaid/Medicare patients.
- Patient Perspectives
- Social Determinants of Health
- Healthcare Settings
- SDOH Screening
- Patient Interest
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Screening for Social Determinants of Health (SDOH) and offering SDOH assistance in health care settings: Patient Perspectives Amy Huebschmann, MD, MS With attribution for project leadership and slides shared by Emilia De Marchis, MD, MAS and UCSF SIREN group April 15, 2020
Funding & Disclosures Funder: The Commonwealth Fund UCSF Social Interventions Research & Evaluation Network (SIREN) led this multi- site research project University of Colorado Internal Medicine clinic served as one of 10 national sites of study that had not previously conducted SDOH screenings (Huebschmann site PI)
Policy Push for Social Risk (SDOH) Screening in Health Care
Patient Interest in Health Care- Based Assistance Social Risks Social Risk Screening Results Interest in Social Care Assistance
Patient Interest in Health Care- Based Assistance Social Risks Interest in Social Care Assistance Social Risk Screening Results
Patient Interest in Health Care- Based Assistance with Social Risks Social Risk Screening Results Interest in Social Care Assistance
Patient Interest in Health Care- Based Assistance Social Risks Social Risk Screening Results Interest in Social Care Assistance ?
Aims presented today Within diverse primary care and emergency care health systems caring for >50% Medicaid/Medicare patients: 1.Determine the acceptability of health care- based SDOH/social risk screening to patients and their caregivers 2. Examine the frequency and predictors of interest in SDOH/social risk assistance in diverse health care setting De Marchis E, et al. Part 1: A Quantitative Study of Social Risk Screening Acceptability in Patients and Caregivers. Am J Prev Med, 2019.
Hypothesized Factors Associated with Acceptability (Aim 1) and Interest in Assistance (Aim 2) Burden of social risks Prior exposure to social risk screening in health care setting Trust in provider Surveyed in safety net setting Experience of discrimination in health care setting
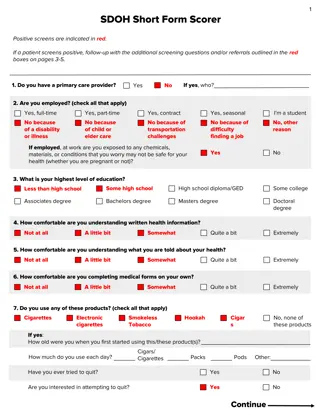
Methods: SDOH Screening tool Centers for Medicare/Medicaid Accountable Health Communities national demonstration Developed 10-item social risk screening tool covering 5 actionable domains Transportation Food Housing Utilities Abuse https://innovation.cms.gov/files/worksheets/ahcm-screeningtool.pdf
Methods: Interest in SDOH assessment Would you like to receive assistance with any of the following issues? (Check all that apply). Transportation Food Housing Utilities Abuse
Methods Primary care Emergency department
Aim1: Survey Measures of Acceptability 1. Do you think it is appropriate to be asked these questions about your social and economic needs at [ this clinic or this emergency department ]? 2. Would you be comfortable having these kinds of needs included in your health records (also known as your medical record or chart)?
Results Assess for eligibility (n=1771) Excluded (n=681) - Declined (n=488) - Did not meet criteria (n=193) Began survey (n=1090) Did not complete (n=32) Completed at least 50% of survey (n=1054) Responded to question about interest in assistance (n=1021)
Results: Participant Demographics Survey only (n=1021) % 71 78 38 17 Female Adult patient FPL <101% Spanish speaker Race/Ethnicity Non-Hispanic White Non-Hispanic Black Hispanic 37 21 33 Abbreviations: FPL, Federal Poverty Limit
Aim 1 Results - Acceptability 83% of primary care and 75% of emergency department respondents thought screening was very or somewhat appropriate Only 7% reported screening as inappropriate 66% of primary care and 62% of emergency department respondents were very or somewhat comfortable with screening information being in their EHR 20% reported being uncomfortable with recording information in the EHR De Marchis E, et al. Part 1: A Quantitative Study of Social Risk Screening Acceptability in Patients and Caregivers. Am J Prev Med, 2019.
Acceptability Results: Multivariable Model Acceptability Appropriateness aOR (95% CI) EHR Integration aOR (95% CI) Prior social risk screening 1.82* (1.16 - 2.88) - Surveyed in safety-net setting 1.71* (1.23 - 2.38) - Complete trust in clinician 1.55* (1.00 2.40) Prior health care discrimination 0.66* (0.45 - 0.95) - Prior assistance with social risks - 1.47* (1.04-2.07) Clustering by health care site; model included region, self-reported health, positive social risk screening results
Aim 2: Rates of positive SDOH Screen Survey only (n=1021) % Participant response to AHC social risk screening tool Housing instability/problem Food insecurity Transportation problem Utilities problem Personal safety concern Overall number of positive social risk screening domains No reported risks 1-2 reported risk 3-5 reported risks 52 41 20 13 2 35 47 17
Aim 2: Interest in assistance by +SDOH screen 53% 100% 93% 100% 77% 80% 56% 60% 32% 40% 9% 20% 0% 0 1 2 3 4 5 Number of Positive Social Risk Domains Interest in assistance
Results: Rates of interest in assistance 100% 80% 60% 35% 37% 40% 35% 40% 11% 20% 8% 8% 4% 5% 2% 0% Screened positive Screened negative
Preliminary Results: Multivariable model Interest in Assistance Screened Positive aOR (95% CI) Screened Negative aOR (95% CI) Number of social risks - 2.40 (1.68, 3.32)* Non-Hispanic Black vs. White 0.57 (0.18, 1.88) 3.78 (2.00, 7.17)* Low income vs. High 7.82 (2.96, 20.44)* 12.38 (2. 94, 52.15)* Fair/poor health vs. Good 1.50 (0.92, 2.46) 4.22 (1.09, 16.31)* Prior screening for social risks 1.42 (0.90, 2.26) 2.35 (1.47, 3.74)* Answering questions about interest in assistance first 1.52 (0.49, 4.70) 1.48 (1.05, 2.07)* Adjusting for age, sex, education, language, participant type, trust, experience of discrimination prior experience with social risk screening/assistance, acceptability of screening, health care setting *p<0.05
Limitations Cross-sectional Excluded patients who did not speak or read English or Spanish Limited to 10 included sites Acceptability and Interest in assistance asked as part of a research study
Conclusions Acceptability of SDOH screening is very high among patients, but a significant minority would not want the answers recorded in the health record. Congruence between positive screening and interest in assistance is higher among: those with multiple social needs, of lower income, and in those asked about interest in assistance before being screened for social risks. People we are more likely to miss if we don t explicitly ask about interest in assistance (negative SDOH screen/+interest in assistance): those in poorer health and of lower income
Future Directions Screen for interest in assistance rather than social risk, per se? Use of tools that guide patients towards resources/assistance in the process of screening? Myownhealthreport.org (select other clinic) UCSF Siren network has excellent resources for implementing screening on their website (sirenetwork.ucsf.edu) and a free monthly e-newsletter
Thank you! Research team: Emilia DeMarchis, MD, MPH Danielle Hessler, PhD Caroline Fichtenberg, PhD Elena Byhoff, MD, MSc Alicia Cohen, MD, MSc Eric Fleegler, MD, MPH Nicholas Gavin, MD Mark Ommerborn, MPH Cheryl Clark, MD, ScD Laura Gottlieb, MD, MPH
Thank you! University of Arkansas Boston Medical Center Brigham & Women s Hospital University of Chicago University of Colorado Dartmouth Medical Center Hennepin Health Center La Familia Medical Center New York University Sirenetwork.ucsf.edu
Thank you! Questions/Comments: amy.Huebschmann@cuanschutz.edu @ahuebschmann