Understanding Orthomyxoviruses and Influenza: A Detailed Overview
Explore the characteristics, structure, gene functions, replication process, and virulence factors of Orthomyxoviruses, specifically focusing on the diverse types of Influenza viruses and their impact on human health. Learn about the group-specific and type-specific antigens, as well as the replication cycle involving viral protein synthesis and RNA transcription in the nucleus.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Enveloped RNA Viruses Enveloped RNA Viruses ORTHOMYXOVIRSES ORTHOMYXOVIRSES Influenzaviruses Influenzaviruses
ORTHOMYXOVIRUSES Influenza Virus Pleomorphic RNA virus, genome consists enveloped virus,with haemagglutinin& neuraminidase spikes. 3 types: A, B, and C Type A undergoes antigenic shift and drift. Type B undergoes antigenic drift only and type C is relatively stable. of 8 segments 2
ORTHOMYXOVIRUSES HA - hemagglutinin NA - neuraminidase helical nucleocapsid (RNA plus NP protein) lipid bilayer membrane polymerase complex M1 protein type A, B, C : NP, M1 protein sub-types: HA or NA protein 3
Influenza viruses have both group-specific and type-specific antigens. 1.The internal ribonucleoprotein is the group-specific antigen that distinguishes influenza A, B, and C viruses. 2.The hemagglutinin and the neuraminidase are the type-specific antigens located on the surface. Antibody against the hemagglutinin neutralizes the infectivity of the virus (and prevents disease), whereas antibody against the group-specific antigen (which is located internally) does not. Antibody against the neuraminidase does not neutralize infectivity but does reduce disease by decreasing the amount of virus released from the infected cell and thus reducing spread of the virus to adjacent cells. An important determinant of the virulence of this virus is a nonstructural protein called NS 1 encoded by the genome RNA of influenza virus. NS 1 has several functions, but the one pertinent to virulence is its ability to inhibit the production of interferon mRNA. As a result, innate defenses are reduced and viral virulence is correspondingly enhanced.
Influenza replication Replication of influenza A virus. After binding (1) to sialic acid-containing receptors, influenza is endocytosed and fuses (2) with the vesicle membrane. Unlike for most other RNA viruses, transcription (3) and replication (5) of the genome occur in the nucleus. Viral proteins are synthesized (4), helical nucleocapsid segments form and associate (6) with the M1 protein-lined membranes containing M2 and the HA and NA glycoproteins. The virus buds (7) from the plasma membrane with 11 nucleocapsid segments. (-), Negative sense; (+), positive sense; ER, endoplasmic reticulum.
The virion RNA polymerase transcribes the eight genome segments into eight mRNAs in the nucleus. Synthesis of the eight mRNAs occurs in the nucleus .Most of the mRNAs move to the cytoplasm, where they are translated into viral proteins. Some of the viral mRNAs remain in the nucleus, where they serve as the template for the synthesis of the negative-strand RNA genomes for the progeny virions.
The helical ribonucleoprotein assembles in the cytoplasm, matrix protein mediates the interaction of the nucleocapsid with the envelope, and the virion is released from the cell by budding from the outer cell membrane at the site where the hemagglutinin and neuraminidase are located. The neuraminidase releases the virus by cleaving neuraminic acid on the cell surface at the site of the budding progeny virions. Influenza virus, hepatitis delta virus, and retroviruses are the only RNA viruses that have an important stage of their replication take place in the nucleus
where do new HA and NA come from? ~18 types HA ~9 types NA all circulate in birds pigs can be infected by avian and human influenza viruses 10
Influenza A reservoir Wild aquatic birds are the main reservoir of influenza A viruses. Virus transmission has been reported from wild waterfowl to poultry, sea mammals, pigs, horses, and humans. Viruses are also transmitted between pigs and humans, and from poultry to humans. Equine influenza viruses have recently been transmitted to dogs.
ANTIGENIC DRIFT HA and NA accumulate mutations RNA virus immune response no longer protects fully sporadic outbreaks, limited epidemics 12
ANTIGENIC SHIFT new HA or NA proteins pre-existing antibodies do not protect may get pandemics 13
Past Antigenic Shifts 1918 H1N1 Spanish Influenza 20-40 million deaths 1957 H2N2 Asian Flu 1-2 million deaths 1968 H3N2 Hong Kong Flu 700,000 deaths 1977 H1N1 Re-emergenceNo pandemic At least 18 HA subtypes and 9 NA subtypes occur in nature. Up until 1997, only viruses of H1, H2, and H3 are known to infect and cause disease in humans.
why do we not have influenza B pandemics? so far no shifts have been recorded no animal reservoir known 15
Influenza pathogenesis Pathogenesis of influenza A virus. The symptoms of influenza are caused by viral pathologic and immunopathologic effects, but the infection may promote secondary bacterial infection. CNS, Central nervous system.
TRANSMISSION AEROSOL 100,000 TO 1,000,000 VIRIONS PER DROPLET 18-72 HR INCUBATION SHEDDING 17
Pathogenesis & Immunity After the virus has been inhaled, the neuraminidase degrades the protective mucus layer, allowing the virus to gain access to the cells of the upper and lower respiratory tract. The infection is limited primarily to this area because the proteases that cleave the hemagglutinin are located in the respiratory tract. Despite systemic symptoms, viremia rarely occurs. The systemic symptoms, such as severe myalgias, are due to cytokines circulating in the blood. There is necrosis of the superficial layers of the respiratory epithelium. Influenza virus pneumonia, which can complicate influenza, is interstitial in location. Immunity depends mainly upon secretory IgA in the respiratory tract. IgG is also produced but is less protective. Cytotoxic T cells also play a protective role. 18
PROTECTION AGAINST RE-INFECTION IgG and IgA IgG less efficient but lasts longer antibodies to both HA and NA important antibody to HA more important (can neutralize) 19
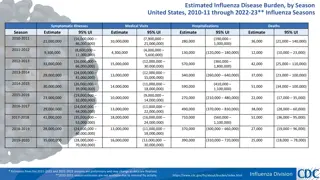
Influenza Sixth leading cause of death Death in the elderly is about 1/1000 cases or 36,000 deaths per year Hospitalization in the elderly is about 1/250 cases
CLINICAL FINDINGS SEVERITY VERY YOUNG ELDERLY IMMUNO- COMPROMISED HEART OR LUNG DISEASE 21
SYMPTOMS FEVER HEADACHE MYALGIA COUGH RHINITIS OCULAR SYMPTOMS 22
PULMONARY COMPLICATIONS CROUP (YOUNG CHILDREN) PRIMARY INFLUENZA VIRUS PNEUMONIA SECONDARY BACTERIAL INFECTION Streptococcus pneumoniae Staphlyococcus aureus Hemophilus influenzae 23
NON-PULMONARY COMPLICATIONS Myositis (rare, > in children, > with type B) Cardiac complications Recent studies report encephalopathy Reye s syndrome : : a child's blood sugar level typically drops while the levels of ammonia and acidity in his or her blood rise. liver - fatty deposits brain edema vomiting, lethargy, coma Guillian-Barr syndrome :peripheral nervous system involved and muscle weakness. 24
MORTALITY MAJOR CAUSES OF INFLUENZA VIRUS- ASSOCIATED DEATH: BACTERIAL PNEUMONIA CARDIAC FAILURE 90% OF DEATHS IN THOSE OVER 65 YEARS OF AGE 25
Laboratory Diagnosis Detection of Antigen - a rapid diagnosis can be made by the detection of influenza antigen from nasopharyngeal aspirates and throat washings, Seputum by immunofluorescence test( IFT) and ELISA. Virus Isolation - virus may be readily isolated from nasopharyngeal aspirates and throat swabs. GROW IN TISSUE CULTURE OR EGGS , Serology - a retrospective diagnosis may be made by serology. CFT(complet fixation test) most widely used. hemagglutination inhibition ( HAI) and Enzyme immunoassay (EIA) may be used to give a type-specific diagnosis PCR,RT-PCR
Avian Influenza H5N1 An outbreak of Avian Influenza H5N1 occurred in Hong Kong in 1997 where 18 persons were infected of which 6 died. The source of the virus was probably from infected chickens and the outbreak was eventually controlled by a mass slaughter of chickens in the territory. All strains of the infecting virus were totally avian in origin and there was no evidence of reassortment. Avian H5N1 has spread to humans So far human cases in Asia and Africa 331 cases (12-1-03 through 10-17-07) 203 (61%) fatal Have been a few instances where may have spread human-to-human So far no sustained spread in humans H9N2 :Several cases of human infection with avian H9N2 virus occurred in Hong Kong and Southern China in 1999. The disease was mild and all patients made a complete recovery Again, there was no evidence of reassortment
The ability of the H5N1 strain to infect chickens (and other effectively than humans is due to the presence of a certain type of viral receptor throughout the mucosa of the chicken respiratory tract. In contrast, humans have this type of receptor only in the alveoli, not in the upper respiratory tract. This explains why humans are rarely infected with the H5N1 strain. However, when the exposure is intense, the virus is able to reach the alveoli and causes severe pneumonia. birds) more
The virulence of the H5N1 strain is significantly greater than the H1N1 and H3N2 strains that have been causing disease in humans for many years. This is attributed to two features of the H5N1 strain, namely, relative resistance to interferon and increased induction of cytokines, especially TNF. The increase in cytokines is thought to mediate the pathogenesis of the pneumonia and acute respiratory distress syndrome (ARDS) seen in H5N1 infection.
The H5N1 strain is sensitive to the neuraminidase inhibitors, oseltamivir (Tamiflu) and zanamivir (Relenza), Tamiflu is the drug of choice for both treatment and prevention. There is no human vaccine available against the H5N1 strain, but there is one available for use in avian species. In 2008, the FDA approved an inactivated vaccine against H5N1 influenza virus but, as of this writing, it is not available to the public.
Swine flu Highly contagious acute respiratory disease in pigs caused by several strains of swine influenza virus A (H1N1, H1N2, H3N1, H3N2) Outbreaks & sporadic human infection occasionally Reported Symptoms are similar to seasonal influenza (asymptomatic to severe pneumonia) Mild cases may escape recognition People usually get swine influenza from infected pigs, however sometimes human cases lack history of contact Human-to-human transmission has occurred but limited to close contacts and close groups of people.
Swine flu Pigs also can be infected with Avian Influenza &human seasonal influenza viruses. Pigs can be infected with more than one virus type which allow genes from viruses to mix. This is known as reassortment of genes & a new influenza virus is formed.
Swine Influenza Virus Infection in Humans In April 2009, a novel swine origin strain of influenza A (H1N1) virus (swine-origin influenza virus, S-OIV) caused an outbreak of human influenza, which appeared first in Mexico, then in the United States, followed by spread to 208 countries by December 2009. Symptoms are in general mild, with the few fatalities occurring in medically compromised patients. There was no outbreak of swine influenza in pigs prior to this human outbreak. Eating pork does not transmit the virus. 33
Swine Flu differs from Human Flu The H1N1 swine flu viruses are antigenically very different from human H1N1 viruses and, therefore, vaccines for human seasonal flu would not provide protection from H1N1 swine flu viruses www.medicalppt.blogspot.com FOR MORE LECTURES
Vaccination 1) Inactivated split/subunit vaccines are available against influenza A and B . 2) Formalin fixed wild type virus approved for parenterally administered vaccination. Trivalent: two current A strains and one current B strain 3) Live attenuated vaccine now available ( Flumist ) Temperature sensitive recombinant bearing relevant HA and NA genes.
Prevention The vaccine is normally trivalent, consisting of one A H3N2 strain, one A H1N1 strain, and one B strain. The strains used are reviewed by the WHO each year. The vaccine should be given to debilitated and elderly individuals who are at risk of severe influenza infection. Amantidine can be used as an prophylaxis for those who are allergic to the vaccine or during the period before the vaccine takes effect.
The vaccine should be given to people older than 50 years of age, children 6 to 23 months of age, and to those with chronic diseases, particularly respiratory and cardiovascular conditions. It should also be given to health care personnel who are likely to transmit the virus to those at high risk. In 2009, the recommendation was expanded to include immunization of children 5 to 18 years of age.
Summary: influenza Structure Negative sense segmented ssRNA genome, helical nucleocapsid, enveloped Pathogenesis respiratory transmission replication in nucleus; budding no spread (usually) innate and antibody response important; antigenic shift and drift local symptoms from cell killing; systemic symptoms from immune response; exaggerated disease in young and elderly; viral and bacterial pneumonia complications Diagnosis culture, hemadsorbtion, viral antigen detection Treatment/prevention amantidine and rimantidine target matrix; zanamivir and oseltamivir target NA killed and live vaccines need constant updating



![Preventing Influenza at [Name of Critical Access Hospital]](/thumb/233818/preventing-influenza-at-name-of-critical-access-hospital.jpg)