Understanding Mental Health Perceptions in Ugandan Communities
Depression ranks high in disability burden in Uganda, but mental health data is scarce. A study explored community perspectives on mental health in urban, rural, and fishing communities in Wakiso and Hoima districts. Participants shared experiences and perceptions regarding mental health disorders, highlighting the impact of external stressors.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
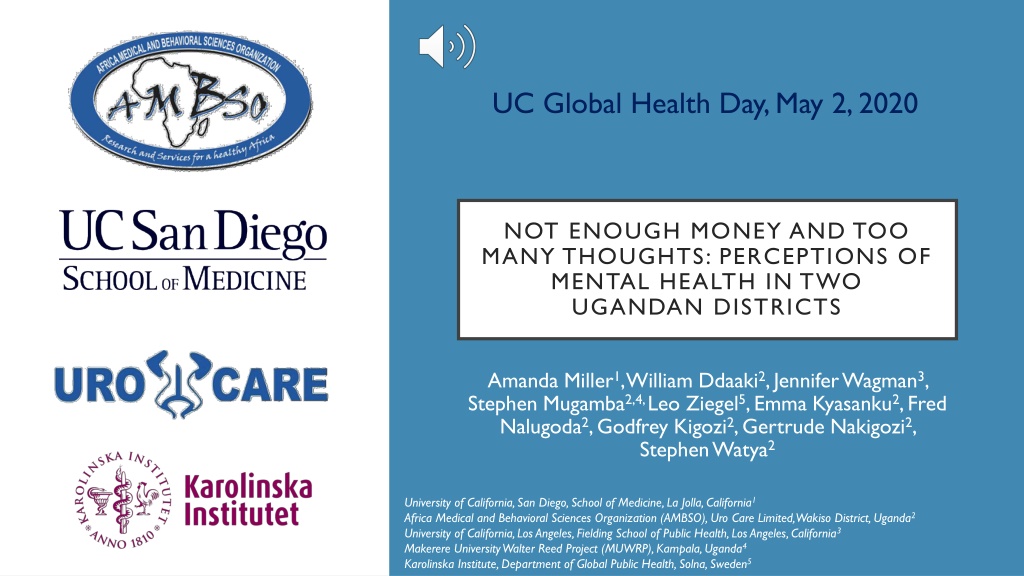
UC Global Health Day, May 2, 2020 NOT ENOUGH MONEY AND TOO MANY THOUGHTS: PERCEPTIONS OF MENTAL HEALTH IN TWO UGANDAN DISTRICTS Amanda Miller1, William Ddaaki2, Jennifer Wagman3, Stephen Mugamba2,4, Leo Ziegel5, Emma Kyasanku2, Fred Nalugoda2, Godfrey Kigozi2, Gertrude Nakigozi2, Stephen Watya2 University of California, San Diego, School of Medicine, La Jolla, California1 Africa Medical and Behavioral Sciences Organization (AMBSO), Uro Care Limited, Wakiso District, Uganda2 University of California, Los Angeles, Fielding School of Public Health, Los Angeles, California3 Makerere University Walter Reed Project (MUWRP), Kampala, Uganda4 Karolinska Institute, Department of Global Public Health, Solna, Sweden5
BACKGROUND METHODS Depression is the second leading cause of disability adjusted life years (DALYs) in the African region and the third leading cause of disability in Uganda. [1,2] Between November 2018 and October 2019, we conducted 3 focus groups (one with community leaders, one with drug users and one with sex workers) and 31 in-depth interviews Participants were men and women, 14-54 years of age in 5 communities across two districts in Uganda. Mental health data from sub-Saharan Africa is scarce. What is available is mostly from the healthcare providers or focused on perceptions and specific mental health disorders (MHD). perspectives of Purposive sampling was used to capture perspectives from a wide range of community members (e.g. community leaders, substance users, fisherfolk, younger and older residents). understandings of We sought to address this gap by exploring how mental health is understood by men and women residing in urban, semi-urban, rural and fishing communities in two districts in Uganda: Wakiso and Hoima districts. Data were collected in the local languages of Luganda and Runyoro by trained and experienced local qualitative research staff. Coding was completed using Dedoose qualitative software and analysis and synthesis of the coded content was undertaken by four researchers.
Participants felt MHDs were present in their community and some shared first-hand experiences. Yes, I have seen very many people affected with mental health disorders here including myself. [male, 29 years, rural community] [ ] I have experienced some of these symptoms for instance keeping silent and losing appetite more especially when am lacking what to feed my children, their father divorced me and am the one responsible for their education, feeding and medical care, you can imagine such a situation when you are a woman. [Female, 35-49 years, fishing community,] RESULTS A few participants in Wakiso district mentioned that while they observed symptoms of MHDs in neighbors, this was a private matter that could not be broached by non-immediate family members. There were 61 participants (n=30 for the focus group discussions and n=31 for the in-depth interviews). I think [persons experiencing MHDs] are there among people in this community but because people don t talk about their problems, it is really very difficult for me to tell that such people are affected although we hear that they are there. [female sex worker, 26 years, urban community]
Participants perceived external stressors leading to too many thoughts, such as poverty, substance use, living with an illness (such as HIV) and poor relationships in the community as the primary cause of MHDs. The other barrier is diseases, when you are diagnosed with a killer disease like cancer and HIV, you don t feel jolly and free, and this limits you from achieving good mental health. [Female, 35-49 years, fishing community] Participants described recognizable symptoms among community members that they felt were indicative of a MHD., including withdrawal from friends and family, forgetfulness, weight loss, poor hygiene, changes in behavior, decreased self-control, headache and sadness. Some of the common symptoms I usually see is that someone who used to bath is no longer bathing now, someone who used to wash clothes is no longer washing. Actually, that person is no longer embarrassed even if there [are] young children he uses vulgar words. Then I just know that he is suffering from mental problems. [male, drug user in focus group, rural community] Participants were not explicitly asked if mental health services and resources existed in their community. For this reason, none were noted during the interviews despite the recognized need. RESULTS
CONCLUSIONS AND RECOMMENDATIONS: MHDs were perceived as being present across community types in Uganda. A few individuals mentioned that it was difficult to ask people about their mental health because people don t talk about issues outside the immediate family. Participants perceived MHDs as being primarily driven by external stressors, with less awareness of biological and genetic factors that may leads to MHDs, highlighting a gap in community mental health literacy. Additional research is needed to explore acceptable low cost, sustainable community level interventions (e.g. provision of relevant educational resources as well as therapeutic and psychiatric services) that could be implemented in this setting to address common MHDs, such as depression and anxiety. Thank you to the study participants, without whom this research could not have been completed!