Understanding Meningitis: Causes, Symptoms, and Treatment
Learn about meningitis, an inflammation of the membranes surrounding the brain and spinal cord. Discover the etiology, types (bacterial and viral), symptoms, and treatment options for this condition.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Meningitis 1stWeek Neurosurgical Co-Assistant Tutorial with dr. M. Deni Nasution, Sp.BS
Definition Meningitis membranes (meninges) surrounding the brain and spinal cord is an inflammation of the Mayo Clinic Diseases and Condition, January 6th 2016
Waxman SG. 2017. Clinical Neuroanatomy 28th Edition. McGraw-Hill Education: USA. p277
Etiology Meningitis usually results from a viral infection, but the cause may also be a bacterial infection. Less commonly, a fungal infection may cause meningitis. Meningitis can also result from noninfectious causes. Bacterial infection are the most serious and life threatening. Mayo Clinic Diseases and Condition, January 6th 2016
Bacterial Meningitis (= Acute Pyogenic Meningitis) The main bacteria responsible vary depending on age and/or context: A. Meningitis in a non-epidemic context: Children 0 3 months: Children 7 days: Gram-negative bacilli (Klebsiella spp, E. coli, S. marcesens, Pseudomonas spp, Salmonella spp) and group B streptococcus Children > 7 days: S. pneumoniae accounts for 50% of all bacterial meningitis, L. monocytogenes Children 3 months 5 years: S. pneumoniae, H. influenza B and N. meningitidis Children > 5 years and adults: S. pneumoniae and N. meningitidis Grouzard V, Rigal J, Marianne S. 2016. Clinical Guidelines. Medicins Sans Frontieres: Paris. p175
Bacterial Meningitis (= Acute Pyogenic Meningitis) The main bacteria responsible vary depending on age and/or context: B. Meningitis in an epidemic context: In the Sahelian region during the dry season, epidemics of meningococcal meningitis (Neisseria meningitides A or C or W135) affect children from 6 months of age, adolescents, and adults. In these regions, whether during epidemics or not, all the above pathogens can be found, especially in young children. Grouzard V, Rigal J, Marianne S. 2016. Clinical Guidelines. Medicins Sans Frontieres: Paris. p175
Viral Meningitis A group of viruses known as enteroviruses is responsible for most viral meningitis cases in the United States. These viruses tend to circulate in late summer and early fall. Viruses such as herpes simplex virus, HIV, mumps, West Nile virus and others also can cause viral meningitis. Mayo Clinic Diseases and Condition, January 6th 2016
Fungal Meningitis Fungal meningitis is relatively uncommon and causes chronic meningitis. Occasionally it can mimic acute bacterial meningitis. However, this form of meningitis isn't contagious from person to person. Cryptococcal meningitis is a common fungal form of the disease that affects people with immune deficiencies, such as AIDS. It's life-threatening if not treated with an antifungal medication. Mayo Clinic Diseases and Condition, January 6th 2016
Other Causes Meningitis can also result from noninfectious causes, such as chemical reactions, drug allergies, some types of cancer and inflammatory diseases such as sarcoidosis. Mayo Clinic Diseases and Condition, January 6th 2016
Pathophysiology Most cases of meningitis are caused by an infectious agent that has colonized or established a localized infection elsewhere in the host. Potential sites of colonization or infection include the skin, the nasopharynx, the respiratory tract, the gastrointestinal (GI) tract, and the genitourinary tract. The organism invades the submucosa at these sites by circumventing host defenses (e.g., physical barriers, local immunity, and phagocytes or macrophages). Hasbun R. 2016. Meningitis. Medscape Drugs & Diseases
Pathophysiology An infectious agent (ie, a bacterium, virus, fungus, or parasite) can gain access to the CNS and cause meningeal disease via any of the 3 following major pathways: Invasion of the bloodstream (ie, bacteremia, viremia, fungemia, or parasitemia) and subsequent hematogenous seeding of the CNS A retrograde neuronal (eg, olfactory and peripheral nerves) pathway (e.g. Naegleria fowleri or Gnathostoma spinigerum) Direct contiguous spread (eg, sinusitis, otitis media, congenital malformations, trauma, or direct inoculation during intracranial manipulation) Invasion of the bloodstream and subsequent seeding is the most common mode of spread for most agents. This pathway is characteristic of meningococcal, cryptococcal, syphilitic, and pneumococcal meningitis. Hasbun R. 2016. Meningitis. Medscape Drugs & Diseases
Clinical Features Children over 1 year and adults - Fever, severe headache, photophobia, neck stiffness. - Brudzinski s sign and Kernig s sign. - Petechial or ecchymotic purpura (usually in meningococcal infections). - In severe forms: coma, seizures, focal signs, purpura fulminans. Grouzard V, Rigal J, Marianne S. 2016. Clinical Guidelines. Medicins Sans Frontieres: Paris. p175
Clinical Features Children under 1 year The classic signs of meningitis are usually absent. - The child is irritable, appears sick with fever or hypothermia, poor feeding or vomiting. - Other features include: seizures, apnea, altered consciousness, bulging fontanelle (when not crying); occasionally, neck stiffness and purpuric rash. Grouzard V, Rigal J, Marianne S. 2016. Clinical Guidelines. Medicins Sans Frontieres: Paris. p176
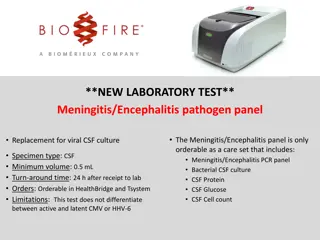
Diagnosis Medical history Physical exam Diagnostic tests Mayo Clinic Diseases and Condition, January 6th 2016
Diagnostic Tests Blood Cultures To see if any microorganism growing, particularly bacteria. Imaging CT-Scan or MRI of the head may show swelling or inflammation. X-rays or CT-scans of the chest or sinuses may also show infection in other areas that may be associated with meningitis. Lumbar Puncture Mayo Clinic Diseases and Condition, January 6th 2016
Lumbar Puncture Grouzard V, Rigal J, Marianne S. 2016. Clinical Guidelines. Medicins Sans Frontieres: Paris. p176
Treatment (Non Epidemic Context) Antibiotic therapy Duration of antibiotic therapy: 1) According to the pathogen: H. influenza: 7 days S. pneumoniae: 10-14 days Group B streptococcus and Listeria: 14-21 days Gram-negative bacilli: 21 days 2) If the pathogen is unknown Children < 3 months: 2 weeks beyond the first sterile CSF culture or 21 days Children > 3 months and adults: 10 days. Consider extending treatment or alternative diagnoses if fever persists beyond 10 days. Grouzard V, Rigal J, Marianne S. 2016. Clinical Guidelines. Medicins Sans Frontieres: Paris. p177
Treatment (Non Epidemic Context) Additional treatment - Dexamethasone reduces the risk of hearing loss in patients with H. influenza or S. pneumoniae. Dexamethasone IV: Children > 1 month and adults: 0.15 mg/kg (max. 10 mg) every 6 hours for 2 days and should be started before or with the first dose of antibiotic, otherwise, the treatment offers no benefit. - Ensure that the patient is well fed and well hydrated (infusions or nasogastric tube if necessary) - Seizures - Coma: prevention of bed sores, care of the mouth and the eyes, etc. Grouzard V, Rigal J, Marianne S. 2016. Clinical Guidelines. Medicins Sans Frontieres: Paris. p178
Treatment (Epidemic Context) Antibiotic therapy - Children under 2 months Ceftriaxone IV or IM for 7 days 100 mg/kg once daily - Children over 2 months and adults Ceftriaxone IV or IM for 5 days Children 2 months to < 5 years: 100 mg/kg once daily (max. 2 g/day) Children 5 years and adults: 2 g once daily Grouzard V, Rigal J, Marianne S. 2016. Clinical Guidelines. Medicins Sans Frontieres: Paris. p179
Treatment (Epidemic Context) Additional treatment - Dexamethasone is not indicated - Ensure that the patient is well fed and well hydrated (infusions or nasogastric tube if necessary) - Coma: prevention of bed sores, care of the mouth and the eyes, etc. Grouzard V, Rigal J, Marianne S. 2016. Clinical Guidelines. Medicins Sans Frontieres: Paris. p178