Understanding Medicare, Medigap & Part D with Blue Harbor Benefits
Blue Harbor Benefits, led by Joseph K. Morgan and Melissa Tower, is a reputable insurance brokerage offering expertise in Medicare, Medigap, and Part D. They simplify the complexities of insurance, catering to businesses of all sizes across the U.S. Their team's vast industry experience ensures clients receive tailored and informed solutions for their health insurance needs. Learn about the various aspects of Medicare, including Part A's coverage for inpatient services, through this informative guide provided by Blue Harbor Benefits.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Medicare, Medigap, & Part D Joseph K. Morgan & Melissa Tower Blue Harbor Benefits
Blue Harbor Benefits: Who Are We? One of the largest independent insurance brokerage offices in the Mid-Atlantic, servicing businesses of all sizes across the country We are licensed throughout the U.S. and broker through all major insurance carriers Our staff averages 20+ years of industry experience and specializes in streamlining the complexities of the insurance world to help you make the best decision(s) for you and your family Our individual market expert, Melissa Tower, has over 15 years of experience in the health insurance arena and helps clients both over and under 65 find the best solutions for their health insurance needs. She also holds her Registered Health Underwriting (RHU) designation and Life and Health Insurance License. Our founder, Joe Morgan, has over 30 years of experience, and holds his Life and Health Insurance License as well his Chartered Retirement Planning Counselor (CRPC) designation among many other titles and designations. He prides himself on Blue Harbor s reputation as being a one-stop-shop for all your insurance wants and needs.
What is Medicare?
Medicare: what, when, how, & how much? Our goal today is to demystify and explain all things Medicare in order to help you prepare yourselves to make the best decision. There are two ways to purchase Medicare: Traditional Medicare Medicare Advantage By the end of this discussion, we hope you will understand each of these and all they entail. ***Numbers presented are based on 2023 date and are subject to change
What is traditional Medicare? Medicare is the federal health insurance program for: People 65 or older Some younger people with disabilities People with end-stage renal disease Medicare has 3 parts: Part A: hospital insurance Part B: medical insurance Part D: prescription drug coverage Medicare Supplement: not a part of the federal program, but still essential Covers all or part of what A & B do not Issued by private insurers (e.g. CareFirst, Mutual of Omaha, AARP) Benefits are regulated by the gov t Medicare Advantage, aka Part C Rolls parts A & B, plus Medicare Supplement into 1 plan Part D is included as well, but not always
Medicare Part A Medicare Part A is considered basic inpatient coverage. It covers stays at: hospitals mental health facilities skilled nursing facilities Part A covers an assortment of inpatient services, including but not limited to: Semi-private room Blood transfusions Skilled nursing care supplies and equipment operating & recovery room hospitals mental health facilities skilled nursing facilities semi-private room blood transfusions skilled nursing care supplies and equipment rehabilitation facilities hospice home healthcare hospital meals special care units drugs (as a part of inpatient treatment)
Medicare Part A: Deductible & Coinsurance Part A has a benefit period deductible of $1,600. A benefit period begins the day you are admitted to a facility as an inpatient and ends when you have gone 60 consecutive days without receiving any inpatient care. After the deductible is met, Medicare pays for the first 60 days of your benefit period in full.
Medicare Part A: Deductible & Coinsurance If you remain in the hospital for more than 60 days, you will be responsible for coinsurance as follows: Days 61-90: $400/day coinsurance > 90 days: lifetime reserve days 60 additional days to be used over the course of your lifetime $800 coinsurance per each lifetime reserve day Once reserve days are used, all costs become your responsibility. To begin a new benefit period, you must stay out of the hospital for 60 consecutive days. Beginning a new benefit period means paying the Part A deductible again.
What does Medicare Part A NOT cover? Routine dental, vision, and hearing Maintenance medications/prescriptions Private care, private nursing, and personal care Anything not deemed medically necessary or preventative Medical services provided by non-Medicare providers You may be able to file a claim for some reimbursement.
Medicare Part B Medicare Part B is comprehensive coverage for outpatient services, durable medical equipment, and doctor s visits. Covered Services include but are not limited to: Doctor visits Lab tests, X-rays, Blood work Mental healthcare Certain outpatient services you receive in the hospital are also covered. For example: Outpatient Surgeries Diagnostic imaging Chemotherapy chemotherapy doctor visits lab tests, x-rays, blood work mental healthcare ambulance services durable medical equipment (i.e. wheelchairs & hospital beds) dialysis administered drugs outpatient surgeries diagnostic imaging
Medicare Part B: Deductible & Coinsurance Deductibles: There is a $226 annual deductible that must be met before Part B will cover outpatient services. Coinsurance: After the deductible, you will be responsible for 20% of covered services.
Medicare Part B: Late Enrollment Penalty The penalty is 10% per month for each full 12-month period that you do not enroll in Part B. 10% of base amount ($160.90) in the first year 20% of the base amount in the second year 30% of the base amount in the third year, etc. enrollment penalty (10% for each full 12-month period that you could have signed up), plus based on your income, you qualify for the Standard Part B premium ($164.90). $164.90 (Standard Part B premium) + $ 32.98 (20% of $164.90) $197.90 (Part B premium for this year rounded to the nearest $0.10) Example: If you waited 2 full years (24 months) to sign up for Part B and didn t qualify for a Special Enrollment Period, you ll have to pay a 20% late The Late Enrollment Penalty NEVER goes away.
What does Medicare Part B NOT cover? Dental, vision, hearing and prescription drug benefits Anything not deemed medically necessary or preventative (e.g. cosmetic surgery) Medical services provided by non-Medicare providers Although you may be able to file a claim for some reimbursement Inpatient services (these are covered under Part A) Other services not covered under Part B include: Long term nursing home care for more than 100 days Acupuncture, Naturopathy, etc. Cosmetic surgery Care outside the United States
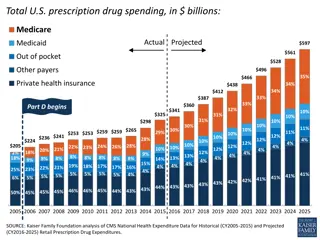
Medicare Part D Medicare Part D is also known as Medicare s prescription drug coverage Coverage is sold by private insurance companies. Coverage and rates vary based on the plan you choose.
The stages of Medicare Part D: Initial Coverage Coverage Gap Catastrophic Coverage You will pay deductible and/or copays until the cost of medication(s) reaches $4,660. This includes what you pay and what the Part D plan pays. You will pay no more than 25% of the cost for medications. You will exit the coverage gap when your total out-of-pocket costs reach $7,400. Once you exit the Coverage Gap, you will pay a maximum of 5% for medications for the rest of the year.
Medicare Part D: Deductibles & Coinsurance Deductibles: Most Part D plans have deductible Deductibles vary, but no drug plan may have a deductible more than $505. Many plans offer coverage on certain medications before the deductible is met. Coinsurance: Once deductibles have been met you may pay coinsurance for some medications. Coinsurance is determined by what stage you are in and what the pharmacy charges for a medication.
Open Enrollment for Medicare Part D: Open enrollment is from October 7 through December 15 each year. Changes during Open Enrollment will be effective on January 1st. If your plan isn t meeting your needs, you can change it during Open Enrollment periods. There are certain situations where you can make a change to your plan outside of Open Enrollment, such as: You make a permanent move and your Part D plan does not have coverage in your new location. Your Part D plan terminates.
Medicare Part D: Late Enrollment Penalty If you do not enroll in a Part D plan when you are initially eligible, you may be subject to late enrollment penalties. The penalty is 1% of the National Base Beneficiary Premium ($32.74) for each month. The penalty is not calculated using your actual premium. NBBP changes each year. Your penalty amount may also change each year. After you join a Medicare drug plan, the plan will tell you if you owe a penalty and what your premium will be. This monthly penalty is added for as long as you have Medicare drug coverage, even if you switch plans. Example: If you waited 14 months after you were eligible for Medicare to join a Medicare drug plan, and you didn t have creditable drug coverage, you ll have to pay a 14% late enrollment penalty in addition to your monthly plan premium. $ 32.74 (BBP) x $ 00.14 (14% = 1% for each month not enrolled in Part D) $ 4.67 (rounded to the nearest $0.10 = $4.70) $4.70 will be your monthly penalty and added to your plan s monthly premium and may change in future years.
Medicare Part D: Creditable Coverage The only way to waive Part D and avoid a fine is to have creditable drug coverage through your employer. While many group plans offer creditable coverage while you are actively employed, you should verify this with your employer prior to turning 65. If your employer s drug coverage is not considered creditable, you may want to come off the employer plan and elect Medicare at your initial eligibility date to avoid Part D penalties. Your employer should provide you with this information each year.
What does Medicare Part D NOT cover? Over-the-counters medications Prescription drugs not covered by Part D include: ED meds Cosmetic or hair growth meds Vitamins Fertility drugs
Medicare Supplement, aka Medigap A Medicare supplement is insurance sold by private companies to help cover some or all of the costs not covered by Medicare. E.g. deductibles, copayments, and coinsurance Every Medicare Supplement policy must follow strict federal and state laws. Insurance companies can only sell standardized policies identified in most states by letters. E.g. the most common plan sold in our area is Plan G; the benefits on Plan G must be the same no matter which carrier you select
How does Medicare Supplement work? Medicare A and B pay the majority of costs. The supplement is the secondary payor and pays all or part of the remaining costs. No networks If the doctor/facility takes Medicare, the Medicare Supplement plan must pay. Works anywhere in the country
Are Medicare Supplement plans medically underwritten? Yes, but There are certain situations where medical underwriting is waived: For the 1st six months after enrolling in Part B You are currently enrolled in Part B and your group-sponsored plan is ending You must enroll in a Medicare Supplement plan within 6 months of your enrollment in Part B If you are already enrolled in Part B, then you have 63 days from the date your group plan ends Must provide detailed documentation proving when coverage started and ended You move out of state and the plan is involuntarily terminated Your entire plan is terminated by the carrier Underwriting makes it challenging to switch plans in future years, so it s important to consider the plan and the carrier when making your choice.
If the benefits are the same across all carriers, why not pick the least expensive? Some carriers offer a discount when you initially enroll. Discount is good for a few years, then you may be left with a premium that is exponentially more expensive. Some carriers use community rating in future years. Your rates are directly affected by the health of those in your geographic area.
Medicare Supplement: Coverage, Deductibles, & Coinsurance The following slides show three Medicare Supplement plans that we recommend based on benefits and costs.
Plan G Medicare Pays Part A Hospitalization First 60 Days 61-90 Days 91+ Days After Reserve (Add. 365 Days) Beyond Add. 365 Days) Skilled Nursing Care First 20 Days 21-100 Days 101+ Days Blood First 3 Pints Additional Amounts Hospice Care Only if Medicare's requirements are met, including a doctor's certification of terminal illness Part B Medical Expenses 1st of $226 of Approved Amount Remainder of Approved Amount Part B Excess Charge Blood First 3 Pints Next $226 of Approved Amount Remainder of Approved Amount Clinical Lab Services- Tests Parts A & B Home Healthcare- Medicare Approved Services Medically necessary skilled care services & medical supplies Durable Medical Equipment 1st $226 of Approved Amount Remainer of Approved Amounts Plan G Pays You Pay All but $1,600 All but $400/day All but $800/day $0 $0 $1,600 (Part A Deductible) $400/day $800/day 100% $0 $0 $0 $0 $0 All costs All approved amounts All but $200/day $0 $0 $0 $0 Up to $200/day $0 All costs $0 100% $0 $0 $0 100% All but very limited copay/ coinsurance for outpatient drugs & inpatient respite care $0 of Medicare approved amounts Medicare copay/coinsurance $0 $0 $226 (Part B Deductible) $0 $0 Generally 80% $0 Generally 20% 100% $0 $0 100% $0 $0 $226 (Part B Deductible) $0 $0 Generally 80% 100% Generally 20% $0 100% $0 $0 $0 80% $0 20% $226 (Part B Deductible) $0
High Deductible Plan G Plan G Pays (after $2,700 Deductible) Medicare Pays Part A You Pay Hospitalization First 60 Days 61-90 Days 91+ Days After Reserve (Add. 365 Days) Beyond Add. 365 Days) Skilled Nursing Care First 20 Days 21-100 Days 101+ Days Blood First 3 Pints Additional Amounts Hospice Care Only if Medicare's requirements are met, including a doctor's certification of terminal illness Part B Medical Expenses 1st of $226 of Approved Amount Remainder of Approved Amount Part B Excess Charge Blood First 3 Pints Next $226 of Approved Amount Remainder of Approved Amount Clinical Lab Services- Tests Parts A & B Home Healthcare- Medicare Approved Services Medically necessary skilled care services & medical supplies Durable Medical Equipment 1st $226 of Approved Amount Remainer of Approved Amounts All but $1,600 All but $400/day All but $800/day $0 $0 $1,600 (Part A Deductible) $400/day $800/day 100% $0 $0, after deductible $0, after deductible $0, after deductible $0, after deductible All costs All approved amounts All but $200/day $0 $0 $0, after deductible $0, after deductible All costs Up to $200/day $0 $0 100% $0 $0, after deductible $0, after deductible 100% All but very limited copay/ coinsurance for outpatient drugs & inpatient respite care $0 of Medicare approved amounts, after deductible Medicare copay/coinsurance $0 $0 $0, after $2,700 deductible & $226 Part B deductible Generally 80% $0 Generally 20% 100% $0 $0 100% $0 $0, after $2,700 deductible & $226 part B deductible Generally 80% 100% Generally 20% $0 Same as above $0, after $2,700 deductible & $226 part B deductible 100% $0 $0 80% $0 20% Same as above Same as above
Plan N Medicare Pays Part A Hospitalization First 60 Days 61-90 Days 91+ Days After Reserve (Add. 365 Days) Beyond Add. 365 Days) Skilled Nursing Care First 20 Days 21-100 Days 101+ Days Blood First 3 Pints Additional Amounts Hospice Care Only if Medicare's requirements are met, including a doctor's certification of terminal illness Part B Plan N Pays You Pay All but $1,600 All but $400/day All but $800/day $0 $0 $1,600 (Part A Deductible) $400/day $800/day 100% $0 $0 $0 $0 $0 All costs All approved amounts All but $200/day $0 $0 $0 $0 Up to $200/day $0 All costs $0 100% $0 $0 $0 100% All but very limited copay/ coinsurance for outpatient drugs & inpatient respite care $0 of Medicare approved amounts Medicare copay/coinsurance $226 (Part B Deductible) Medical Expenses 1st of $226 of Approved Amount Remainder of Approved Amount Part B Excess Charge $0 $0 Up to $20 copay for office visit; up to $50 copay for emergency room visit Generally 80% $0 100%, after copay $0 100% Blood First 3 Pints Next $226 of Approved Amount Remainder of Approved Amount Clinical Lab Services- Tests Parts A & B Home Healthcare- Medicare Approved Services Medically necessary skilled care services & medical supplies Durable Medical Equipment 1st $226 of Approved Amount Remainer of Approved Amounts $0 $0 100% $0 $0 $226 (Part B Deductible) $0 $0 Generally 80% 100% Generally 20% $0 100% $0 $0 $0 80% $0 20% $226 (Part B Deductible) $0
Medicare Supplement: other plans you may have heard of Plan A: This is the only Medicare Supplement plan available to Medicare enrollees under 65 collecting disability benefits. Plans F and C: No longer available to people who turned 65 or became eligible for Medicare after December 31, 2019. Other plans such as B, L and M are not as cost effective in our Marketplace.
What does Medicare Supplement NOT cover? It s important to note that Medicare Supplement policies act as supplemental insurance for Medicare, not additional coverage, so it will not cover anything that Part A and B do not cover. The exception is foreign travel; only a few plans offer it and coverage is very limited. Emergency care only Only available during the first 60 days of each trip outside the United States There is a $250 deductible, then you pay 20% $50,000 lifetime maximum benefit Strongly recommend purchasing a travel insurance policy if traveling abroad
Employer Group Plans & Medicare Depending on the premium amount you pay and the benefits, you may decide to delay your enrollment in Medicare. Here are some things to consider: If your employer has over 20 employees (TEFRA): Your group plan will be the primary insurer and Medicare pays secondary If your employer has under 20 employees (non-TEFRA): Medicare pays primary and your employer plan pays secondary
COBRA & Medicare Parts A, B, & D COBRA cannot be used in lieu of Medicare Part A, B, or D. If you are eligible for Medicare A & B, you have 8 months from the date of the COBRA triggering event to enroll. You have 2 months after you enroll in A & B to enroll in Part D. If you have Medicare first and then become eligible for COBRA, you can have both. Medicare will always pay primary, COBRA pays second. COBRA is rarely considered creditable coverage for Part D, so if you stay on COBRA for more than 63 days, you may incur a late entry penalty when you enroll in Part D If you have COBRA first and then become eligible for Medicare, your COBRA coverage should end. You will need to enroll in Medicare to avoid late entry fees. This may not be automatic so you should reach out to your COBRA administrator. ***Note: similar rules apply if you are subject to MD State Continuation (small group version of COBRA)
Scenarios Scenario #1: Bill is 64, retiring, and electing COBRA. Can he stay on COBRA once he turns 65? What should he do? He must enroll in Medicare Parts A & B within his initial eligibility period to avoid late entrant penalties. If he does not enroll in a Part D plan within 63 days of enrolling in Parts A & B, he may face late entrant penalties. He may be able to keep his COBRA, but his employer is under no obligation to extend coverage once he is enrolled in Medicare. He will need to check with his employer s plan to see how they will handle coordination of benefits. Medicare will become primary, and if he can keep COBRA, it will become his secondary insurer. date, his employer is not obligated to offer him COBRA. Scenario #3: Bob is 68 and retiring. He is enrolled in Medicare Parts A & B. Can he elect COBRA? What should he do? Medicare will be primary and COBRA will be his secondary insurer. If he does not enroll in a Part D plan within 63 days, he may face late entrant penalties. His employer is obligatedto offer him COBRA. Scenario #2: Jim is 66 and retiring. He is not enrolled in Medicare. Can he elect COBRA? What should he do? He must enroll in Medicare Parts A & B within 8 months of his retirement to avoid the penalty. Medicare would be the primary and COBRA would be the secondary. If he does not enroll in a Part D plan within 63 days of enrolling in Parts A & B, he may face late entrant penalties. If he is not enrolled in Medicare on or before the COBRA qualifying event
HSAs, Medicare, & Social Security If you enroll in Medicare Part A and/or B, you can no longer contribute to your HSA. While you can continue to spend from your HSA, you cannot set up or contribute to an HSA in any month that you are enrolled in Medicare. Do you need to stop contributing to an HSA six months before your enrollment in Medicare? If you are 6 months past your full retirement age and also signing up for Social Security retirement benefits, then yes. Social Security will give you 6 months of back pay in retirement benefits. This means that your enrollment in Part A will also be backdated by 6 months. HSA Money can be used to pay Part B, Part D and Medicare Advantage premiums. It cannot be used to pay for Medicare Supplement
When should I enroll in Medicare?
Automatic Enrollment in Medicare Parts A & B If you are collecting Social Security benefits at the time of your 65th birthday, you will be automatically enrolled in both Medicare Parts A & B. If are under 65, disabled, and have met your disability waiting period of 24 months, you will be automatically enrolled in Medicare Parts A & B. Enrollment in part D is NEVER automatic!
Enrolling in Parts A, B, & D at 65 Initial Enrollment Period* Your eligibility date is the first of the month of your 65th birthday. The earliest you can apply is 3 months prior to your eligibility date and coverage will begin on your eligibility date. If you do not apply prior to you 65th birthday, you can apply during the 3 months after and coverage will be effective on the first of the month after your application is received by Medicare. If you apply during this time frame, you will not be subject to late entry penalties. *In this scenario, coverage will never be retroactive.
Enrolling in Medicare when 65 and retiring Special Open Enrollment Period If your initial enrollment period has passed, you may be able to sign up for Parts A & B during a Special Open Enrollment Period without penalty. You can do this if you re covered under your employer s health plan or your spouse s group health plan. You can sign up: Anytime when you re covered by the group health plan In the 8 months following the end of employment or the end of coverage by the group health plan Note: If you sign up for Social Security retirement benefits at the same time you enroll in Medicare, and if you re already six months beyond your full retirement age, Social Security will give you six months of back pay in retirement benefits. This means that your enrollment in Part A will also be backdated by six months.
Oops, you forgot to enroll in Parts A & B! What now?! General Enrollment Period Runs from January 1 through March 31 each year During this time, you can sign up for Parts A and B if both of the following are true: You didn t sign up when you were initially eligible (during initial enrollment). A Special Enrollment Period does not apply. If you enroll during general enrollment, your coverage will begin on July 1. Late enrollment penalty will apply
Enrolling in Part D at 65 or when retiring Initial Enrollment Period You should enroll in Part D within 63 days of enrolling in Part B to avoid late entrant penalties.
Oops, you forgot to enroll in Part D! What now?! If you did not enroll in a Part D plan when you were initially eligible: Open enrollment runs from October 15 to December 7each year. Coverage will begin on January 1 A late enrollment penalty will apply for the months that you were not enrolled in a creditable Part D drug plan.
When should you enroll in a Medicare Supplement plan? We recommend you enroll in a Medicare Supplement Plan so the effective date coincides with your enrollment in Medicare. To avoid underwriting you must enroll within 6 months after your enrollment in a Part B plan. Can you still enroll in a Medicare Supplement Plan outside of this six-month period? YES, but if you are not enrolled in an employer plan you may face underwriting restrictions: Coverage can be denied Premiums can be increased Waiting periods can be implemented before your coverage takes effect Coverage for your pre-existing condition can be excluded
How do I enroll in Medicare?
How to enroll in Medicare Parts A & B You have several ways to enroll in Medicare Parts A & B Online: Visit SocialSecurity.gov to begin enrollment By phone: Call SSA at 1(800)772-1213 (or 1(800)325-0718 for TTY), Mon-Fri, 7 A.M. - 7 P.M. In person: Visit your local SSA office; you can find it through the SSA office locator By mail: Send a letter to your local SSA office with your name, your social security number, and the date you d like to enroll; they will send you the necessary information and any additional requests for enrolling If you already receive benefits from SSA or RRB, you ll be automatically enrolled in Medicare.
How to enroll in Medicare Part D Part D Plans vary greatly depending on the medications you take and the pharmacy you use. Not all Part D plans cover medications the same way The best way to make sure you are getting the right plan for you is to visit the official Medicare website and use their quoting tool: Go to www.medicare.gov Under Find health & drug plans, click on Find Plans Now
How to enroll in Medicare Part D Here you can create an account or continue without logging in (I always continue without logging in) Enter your home zip code and county if prompted Under plan type, click on Drug Plan (Part D) and click Start
How to enroll in Medicare Part D Under Help with your costs, select I don t get help from any of these programs, and then Next Under Tell us your search preferences, select Yes if you have medications to enter and then Next
How to enroll in Medicare Part D To add medications, you will need the following information as it appears on the prescription: Dosage Quantity Frequency Click on Add to My Drug List Repeat to add another drug, OR Click Done Adding Drugs
How to enroll in Medicare Part D Choose a pharmacy You can choose up to 5 pharmacies Click Done and plans will load
The plan selection page will look like this: You can filter by star ratings; we recommend only looking at those rated at 3 or 4 stars.