Understanding Epidemiological Study Designs and Measures of Risks
This informative content covers various epidemiological study designs, including observational and experimental studies, clinical trials, cohort studies, and more. It explains the concept of cohorts, indications for cohort studies, and the design considerations involved. Images are included to illustrate key points visually.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Epidemiological Study Designs And Measures Of Risks (2) Dr. Khalid El Tohami
Objectives of the Lecture To describe observational study designs To describe experimental study designs and clinical trials Calculate and interpret of measures of risk
Case stud. Descriptive stud. Surveys Non intervention stud. (Observational) Ecological (correlational) Analytical stud. Cross-sectional (Prevalence) Study designs Case con. Stud. (case-reference) Randomized control Trials (Clinical trials) Intervention stud. (Experimental) Cohort stud. (Follow-up) Non-randomized trials (Quasi-experimental study)
Cohort Study Cohort study is type of analytical studies. Distinguishing features: A. Cohort identified before appearance of disease under investigation. B. Study groups observed over period of time to determine frequency of the disease. C. Study proceeds forward from cause to effect.
Concept of cohort: Cohort in epidemiology defined as a group of people who share a common characteristic or experience with in defined period time. Comparison group may be : From the general population. Or Another cohort.
Indications of cohort studies: 1. In good evidence of association between exposure &disease. 2. If exposure is rare but incidence is high among exposed. 3. If attrition of study population can minimized. 4. When funds are available.
Time Direction of inquiry Disease Exposed No disease People without the disease population Disease Not exposed No disease
Framework of a cohort study General consideration to be taken: 1. Cohorts must be free from the disease under study. 2. Both groups should be equally susceptible to the disease under study. 3. Both groups should be comparable in all possible variables. 4. Diagnostic &eligibility criteria must be defined beforehand.
Framework of cohort study disease Yes no total Cohort Exposed to putative aetiological factor A B A+B Not exposed to the factor C D C+D
After the end of follow up , if Incidence of disease in exposed (A/(A +B) > in non-exposed(C/(C+D) this suggest disease & factor are associated. Cohort studies are frequently referred to as prospective .
TYPES OF COHORT STUDIES 1. PROSPECTIVE COHORT S. 2. RETROSPECTIVE COHORT S. 3. COMBINATION
1.Prospective cohort studies:(current) In which outcome has not yet occurred at the time of investigation begins. 2.Retrospective cohort S.(historical) factors occurred before start of investigation.
3. Combination of retrospective & prospective : The cohort is identified from past records & is assessed of date for the outcome. The same cohort is followed up prospectively into future for further assessment of outcome.
Elements of a cohort study 1. Selection of study subjects. 2. Obtaining data on exposure. 3. Selection of comparison groups. 4. Follow up. 5. Analysis.
Analysis of cohort 1.Incidence rate Factor Disease Total yes A C no B D Yes No A+B C+D Among exposed = A/(A+B) Among non- exposed = C/(C+D)
2. Estimation of risk( outcome ): A. Relative risk. RR=incidence of outcome in exposed incidence in non- exposed RR measure strength of association. RR>1 mean positive association.
B. Attributable risk: is the difference in incidence rates between exposed & non- exposed. AR=I.R(exposed)-I.R(non-exp) *100 I.R(exposed)
Advantages & disadvantages of cohort studies: Advantages: 1. calculate incidence rate. 2. can study several outcomes related to exposure simultaneously. 3. provide direct estimate of relative risk. 4. can calculate dose-response ratios. 5. can minimized certain bias.
Disadvantages: 1. Takes long time. 2. Certain administrative problems are inevitable (loss of fund, experienced s). 3. Selection of comparison groups is limiting factor. 4. Changes in standard methods or diagnostic criteria.
5. Are expensive. 6. Usual lose a substantial proportion of the original cohort. 7. Study may affect people behavior. 8. Ethical problems.
Differences between cohort & case control studies: Case control study cohort study 1.proceed from ( effect to cause) Proceed from(cause to effect) 2.starts with disease Starts from risk factor 3.test if suspected cause occur more in diseased than non-diseased. Test if disease occur more in exposed than non-exposed.
Case control study Cohort study 4.involves fewer number of subjects Involves large number of subjects 5.relatively get quick results Long follow up lead to delayed results. 6.suitable for study of rare diseases Inappropriate in rare diseases or exposure. 7.yields only estimate of RR(odds ratio) Yields incidence rate, RR as well as AR 8.relatively inexpensive expensive
Experimental Study Designs In experimental studies the researcher manipulates a situation and measures its effect after that Type: 1- Randomized control trials 2- Non-randomized trials
1) RANDOMIZED CONTROLLED TRIALS Those trials are used for assessment of methods of treatment and prevention. They include: - intervention - control groups and - randomization
Features of Randomized control trials 1- Manipulation: The researcher does some intervention (Example provision of new drug) to one of the study groups. 2- Control: The researcher introduces one or more control groups to compare with the experimental group 3- Randomization: Each subject have an equal chance of being allocated to either of the two groups( study and comparison groups)
steps 1. Drawing a protocol. 2. Selecting comparison & experimental groups 3. Randomization. 4. Manipulation (intervention). 5. Follow up. 6. Assessment of the outcome.
RANDOMIZATION Randomization is the statistical procedure by which the participants are allocated into groups usually called study & control groups to receive or not to receive intervention.
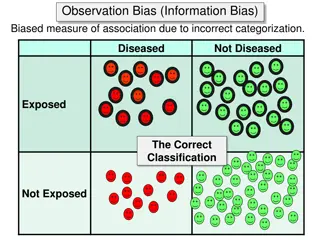
RANDOMIZATION Randomization ensures that the investigator has no control over the allocation of the participants to either the study or control group, thus eliminating the selection bias. Randomization is best done by using statistical random table.
MANIPULATION Manipulation or intervention is usually done by application or withdrawal of the suspected factor e.g. drugs, vaccine or dietary factor. This manipulation creates an independent variable (drug, or new procedure) which effect is then determined by the measurement of the final outcome which is the dependent variable e.g. incidence of disease, recovery.
FOLLOW UP This includes examination of the study & control groups subjects at defined intervals of time in standard manner under the same conditions in the same time frame till the final assessment. The main difficulties in the follow up process include: Attrition from:- death, migration, displacement and loss of interest etc
ASSESSMENT The final assessment of the trial is carried in terms of: Positive results: These include the benefits of the experimental study such as reduced incidence of the disease or severity of the disease, cost of health services or other appropriate outcome.
Negative results: These include the severity & frequency of side- effects and complications. The incidence of positive/negative results is compared in both groups and the differences are tested statistically.
a. QUASI-EXPERIMENTAL STUDY DESIGNS At least one of the characteristics of the true experiment is missing (RANDOMIZATION OR CONTROL GROUP) Example: effect of health education of the level of participation of village population in an immunization campaign.
Blinding. Blinding is carried in three ways: 1. Single blind trial: The participant is not aware whether he belongs to the study or control group.
2. Double blind trial: Neither the doctor nor the participant is aware of the group allocation and treatment received. 3. Triple-blind trial: The participant, the investigator& the person analyzing the data are all blind. This is the ideal but double-blinding is the most commonly used.
DISADVANTAGES OF EXPERIMENTAL STUDIES They are costly. Ethical problems. Feasibility is difficult.
Summary What are the different study designs Enumerate measures of the risk