Tracheostomy Team Initiative & Management Inconsistencies
Tracheostomy team initiatives, led by experienced professionals, play a crucial role in delivering coordinated and effective care for patients with tracheostomies. A multidisciplinary tracheostomy team creates a supportive environment, collaborates on weaning procedures, and educates staff and patients. However, inconsistencies exist in tracheostomy management, such as timing of placement, indications, and technique variances between surgical and percutaneous methods, highlighting the need for thorough evaluation and standardized protocols.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
TRACHEOSTOMY TEAM INITIATIVE CREATED BY: KAHLA GRAHAM M.S. CCC-SLP, BCS-S AMANDA WEISSBERG M.S., CCC-SLP
WHAT IS A TRACHEOSTOMY TEAM? Tracheostomy care can be one of the best examples of multidisciplinary care, with many different medical, nursing and allied health teams being required to deliver coordinated and effective care (Bonvento, et al., 2017, p.392). Review by experienced people may reduce tracheostomy complications that delay recovery whilst a multidisciplinary team allows consensus decisions regarding tracheostomy weaning and decannulation to be made and enacted without the delays associated with multiple separate reviews (Tobin & Santamaria, 2008, p.6).
ROLE OF A MULTIDISCIPLINARY TRACHEOSTOMY TEAM (MDT) Create a supportive environment for this complex patient population requiring the highest level of care to maximize patient safety and prevent adverse medical events. Collaborate, monitor, and review mechanical ventilation weaning and decannulation procedures. Determine appropriateness for cuff deflation, downsizing, speaking valve, and/or capping. Provide appropriate referrals to other disciplines. Educate and train patient and medical staff. Develop collaborative protocols to optimize tracheostomy care. (Bonvento, et al., 2017)
INCONSISTENCIES WITH TRACHEOSTOMY MANAGEMENT Timing of tracheostomy placement (early vs late) Early tracheostomy may be associated with earlier mobility, decreased intensive care unit (ICU) length of stay (LOS), and quality of life (QOL) Early tracheostomy does not appear to decrease the risk of complications such as ventilator acquired pneumonia (VAP), weaning from mechanical ventilation, or hospital LOS Indication and rationale for tracheostomy Difficult airway, prolonged mechanical ventilation, poor secretion management Can also promote verbal communication, patient comfort, and access to oral nutrition Tracheostomy technique (surgical vs percutaneous) Percutaneous tracheostomy placement is performed at bedside does not require in-depth surgical training Percutaneous placement is associated with reduced cost and fewer infectious complications; however, there is a risk of potential morbid complications such as esophageal perforation, aortic injury, and tracheal laceration (Freeman, 2017; Morris et al., 2014)
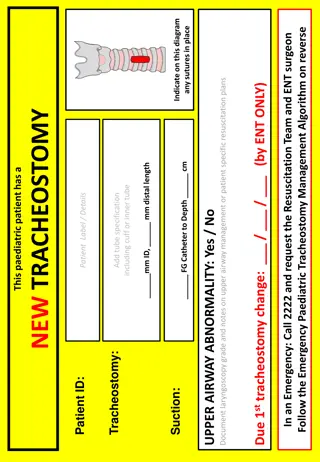
INCONSISTENCIES WITH TRACHEOSTOMY MANAGEMENT Continuity of care with tracheostomy Increased number of percutaneous tracheostomies can result in a loss of follow up by the service that performed the initial tracheostomy (de Mestral et al., 2011) Capping and decannulation protocols (Singh et al., 2017) Qualitative metrics for readiness: cough productiveness, secretion management, swallowing Quantitative metrics for readiness: peak cough flow (PCF), maximum expiratory pressure (MEP), peak inspiratory flow rate (PIFR) Method of decannulation: one-step vs multi-step Patient and RN education/training Timing of communication and swallow evaluations (Bartow et al., 2018) (Bartow et al., 2018; de Mestral et al., 2011; Singh et al., 2017)
EVIDENCE FOR MULTIDISCIPLINARY TEAM Decannulation Time Length of Stay (LOS) Reduced Adverse Events Speaking Valve Use for Communication
EVIDENCE FOR MULTIDISCIPLINARY TEAM Decannulation Time Research has shown a decrease in the mean number of days to decannulation after establishment of MDT: Decreased from 50.4 to 28.4 days (de Mestral et al, 2011). Decreased from 41.9 to 35.4 days (LeBlanc et al., 2010). Decreased from 21 to 11 days (Cetto et al., 2011). One study found a decrease in total timewith tracheostomy, decreased from a mean of 34 to 25 days (Cetto et al., 2011). MDT can also decrease the number of days to decannulation after ICU discharge from a mean of 14 to 9 days (Tobin & Santamaria, 2008).
EVIDENCE FOR MULTIDISCIPLINARY TEAM Length of Stay (LOS) Studies have also demonstrated a decrease in the mean number of days of length of stay after the implementation of MDT: Decreased from 107.81 to 69.94 days (Le Blanc et al, 2010). Decreased from 60 to 41.5 days (Cameron et al., 2009). Decreased from 19.16 to 14.14 total days in ICU (Cetto et al., 2011). Decreased from 30 days (in 2003) to 19 days (in 2006) after discharge from ICU (Tobin & Santamaria, 2008).
EVIDENCE FOR MULTIDISCIPLINARY TEAM Reduced Adverse Events Reduction of tracheostomy-related emergency calls after implementation of MDT (Cameron et al., 2009). Reduction of 58 to 9 critical incidents (Cetto et al., 2011). Decrease in the incidence of tube blockage/mucous plugging and number respiratory distress calls (p = 0.16 and p = .039, respectively) (de Mestral et al., 2011). Reduction in number of adverse medical events from 32% of patients (6/9) to 24% of patients (18/75) after implementation of MDT (Parker et al., 2007). Adverse events included: accidental decannulation, blockage, infection, and other (i.e., neck swelling, hematoma, incorrect tracheostomy/tube size).
EVIDENCE FOR MULTIDISCIPLINARY TEAM Speaking Valve Use for Communication Significant increase (p < .001) in number of patients who received a speaking valve from 19.4% to 67.4% of patients with tracheostomies (de Mestral et al., 2011). Significant increase ( p = .004) in speaking valve use from 33% to 71% of patients with tracheostomies (Le Blanc et al., 2010). Le Blanc et al. (2010) found that the use of PMVs almost doubled after initiation of the tracheostomy team (p. 364).
EVIDENCE FOR MULTIDISCIPLINARY TEAM Cost Benefit Analysis Cost benefit of reduced ICU LOS Amount of money saved across all patients with tracheostomies with ICU LOS reduction when comparing 2004 (pre-MDT) and 2008 (post-MDT) $235,922 (Pandian et al., 2012) Cost benefit per patient Amount of money saved in direct patient cost per patient when comparing 2016 (pre-MDT) to 2018 (post- MDT) $2,452 (Harper et al., 2020) Cost benefit per admission Amount of money saved in total admission cost per patient when comparing 2011-2013 (pre-MDT) to 2013-2015 (post-MDT) $81,432 (Holmes et al., 2019) Decreased cost of admission after implementation of MDT. *all amounts represent median values in dollars
MEMBERS OF THE MDT Core Members Physician: Intensivist, Trauma, Otolaryngologist, Pulmonologist (MD) Speech-Language Pathologist (SLP) Respiratory Therapist (RT) Mid-level Providers APN PA CNS MD SLP RT Patient Other Potential Members Nurse Practitioners, Physician Assistants, Clinical Nurse Specialists Nursing Staff, Nurse Educator, Wound Care Nurse Registered Dietician (RD), Social Worker (SW), Case Manager (CM) (Bartow et al., 2018; Mah et al., 2017; de Mestral et al., 2011)
EXAMPLE I MODEL OF MDT Type of Hospital Trauma Tier II Size of Hospital 375 bed Team Members Intensivist (chief/leader), RT, SLP, and RN Rounding Frequency Bi-weekly Communication Type Shared Document; Weekly email update via team leader Documentation RN completes daily flow sheet. Trach/care and suctioning schedule followed. Policies & Procedures Decannulation Protocol: Tolerate capping for > 24 hours; independently cough secretions. At least size 6 trach prior to decannulation. Downsizing Protocol: Team decision dependent upon secretion amount and upper airway patency.
EXAMPLE II MODEL OF MDT Type of Hospital Trauma Tier I Size of Hospital 1,000 bed Team Members Pulmonologist, RT, SLP Rounding Frequency Weekly Communication Type Shared patient list and flowsheet documentation on EMR. Documentation Trach care and suctioning schedule followed and documented in EMR by RN and team members. Policies & Procedures Coordinated care: Bundled order set s/p tracheostomy for SLP, RT, and RN trach care. Downsizing/Decannulation: Algorithms outlining criteria due to medical complexity.
ROLE OF THE SLP ON THE MDT SLPs have knowledge and expertise of the anatomy and physiology of the aerodigestive tract. SLPs are equipped to provide education and training not only to patients, but to other members of the medical team. MDT can decrease time to SLP consult for evaluation and intervention. Verbal and non-verbal communication evaluation and intervention Instrumental swallow evaluation and intervention Assessment of upper airway patency and secretion management Tracheostomy and speaking valve troubleshooting Patient, caregiver, and medical staff education and training Patient advocacy Facilitate communication and collaboration amongst members of the team (Bartow et al., 2018; Frank et al., 2007; Mah et al., 2017)
SWALLOWING FOR TRACHEOSTOMY PATIENTS According to Bergl et al. (2018), 83% of tracheostomy patients have been found to silently aspirate, highlighting the importance of instrumental swallowing assessment. Instrumental Swallowing Studies SLP to conduct instrumental swallowing study. Video Fluoroscopic Swallowing Study (VFSS) Fiberoptic Endoscopic Evaluation of Swallowing (FEES) Utilizing instrumental assessments for evaluation of the swallow post tracheostomy is warranted due to the complexity of this patient population and high rates of aspiration and silent aspiration (Skoretz et al, 2020).
Swallowing for Tracheostomy Patients DYSPHAGIA OCCURS IN 11% TO 93% OF PATIENTS FOLLOWING TRACHEOSTOMY. Characteristics of Dysphagia Breathe swallow pattern is impaired; we typically swallow mid-expiration to serve as protective mechanism (Prigent et al., 2011). Decreased sensation Reduced subglottic pressure, hyolaryngeal excursion, secretion management Change in cough function Edema If the cuff is inflated silent aspiration is found to be more frequent Silent aspiration rates were 22.6% for cuff inflated versus 7.2% for individuals in the cuff deflated condition (Ding & Logemann, 2005). (Ding & Logemann, 2005; Prigent et al., 2011, Skoretz et al., 2020)
INTERVENTION OF VERBAL AND NON-VERBAL COMMUNICATION Increased Non-Verbal Communication According to the Joint Commission (2010) the patient has the right to communication made as a priority. Providing patient low or high-technology communication assist (e.g., alphabet board, communication board, iPad) is shown to: Prevent adverse events during hospitalizations (Bartlett, et al., 2008). Improve overall QOL to decrease frustration, anger, and withdrawal from treatment (Magnus & Turkington, 2006).
INTERVENTION OF VERBAL AND NON-VERBAL COMMUNICATION Earlier Speaking Valve Introduction Statement from participant in Freeman- Sanderson (2018) study: It was a relief; just so, so good being able to speak ... It was so good to be able to communicate normally instead of trying to mouth words. It was just so much easier (p. 13). All participants in the study confirmed loss of their voice had a significant impact on their ability to effectively communicate. Three research articles reported >2x increase of speaking valve use percentage after implementation of multidisciplinary team. (Speed & Harding, 2013)
IMPROVING QUALITY OF LIFE FOR PATIENTS In a study by Gaspar and colleagues (2015), only 57.1% of nurses felt well-prepared to communicate with patients with tracheostomies. Communication is a multidisciplinary role and an MDT can provide training to medical staff to support communication (Magnus & Turkington, 2006). Lack of voicing impacts patient self-esteem, participation in care, emotional stability, and communication quality of life. I would say mainly stressed and helpless Most of the time I felt trapped (Freeman-Sanderson et al., 2018, p.13) Self-esteem and overall quality of life improves upon restoration of voicing (Freeman-Sanderson et al., 2018).
GETTING STARTED Coordinate physician leader/champion (i.e., MD) and determine multidisciplinary team members. Members may be hospital dependent relative to size and roles. Determine frequency of meetings/rounds. Select mode(s) of communication (i.e., email, shared document, folder, phone conference). Create standardization of patient-centered care. Examples: Vent weaning Decannulation Speaking Valve Consider timeline of realistic implementation of tracheostomy team into hospital system.
TAKEAWAY Multidisciplinary tracheostomy teams promote a collaborative approach and facilitate communication amongst healthcare professionals. The team members and systematic operations of a tracheostomy team are dependent on the institution and the patient population. Multidisciplinary tracheostomy teams can benefit weaning from mechanical ventilation, decannulation, length of stay, cost of admission, and patient quality of life.
REFERENCES Bartlett, G., Blais, R., Tamblyn, R., Clermont, R. J., & MacGibbon, B. (2008). Impact of patient communication problems on the risk of preventable adverse events in acute care settings. CMAJ: Canadian Medical Association journal, 178(12), 1555 1562. doi:10.1503/cmaj.070690 Bartow, C., Collins, N., Kopp, E., & Guillamondegui, O. (2018). Benefits of a multidisciplinary tracheostomy team: Acute care experience. Perspectives of the ASHA Special Interest Groups, 3(13):89 100. doi:10.1044/persp3.SIG13.89 Bergl, P., Kumar, G., Zane, A., Shah, K., Zellner, S., Taneja, A., Nanchal, R. (2018). 517: Acquired dysphagia after mechanical ventilation an underrecognized and undercoded phenomenon? Critical Care Medicine, 46(1): 243. doi:10.1097/01.ccm.0000528535.80915.5b Bonvento, B., Wallace, S., Lynch, J., Coe, B., & McGrath, B. A. (2017). Role of the multidisciplinary team in the care of the tracheostomy patient. Journal of Multidisciplinary Healthcare, 10, 391 398. doi:10.2147/JMDH.S118419 Cameron, T. S., McKinstry, A., Burt, S. K., Howard, M. E., Bellomo, R., Brown, D. J., Ross, J. M., Sweeney, J. M., & O'Donoghue, F. J. (2009). Outcomes of patients with spinal cord injury before and after introduction of an interdisciplinary tracheostomy team. Critical Care And Resuscitation : Journal of the Australasian Academy of Critical Care Medicine, 11(1), 14 19. Cetto, R., Arora, A., Hettige, R., Nel, M., Benjamin, L., Gomez, C. M., Oldfield, W. L., & Narula, A. A. (2011). Improving tracheostomy care: A prospective study of the multidisciplinary approach. Clinical Otolaryngology : Official Journal of ENT-UK ; Official Journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial Surgery, 36(5), 482 488. https://doi.org/10.1111/j.1749-4486.2011.02379 de Mestral, C., Iqbal, S., Fong, N., LeBlanc, J., Fata, P., Razek, T., & Khwaja, K. (2011). Impact of a specialized multidisciplinary tracheostomy team on tracheostomy care in critically ill patients. Canadian Journal of Surgery, 54 (3), 167-172. doi:10.1503/cjs.043209
REFERENCES Ding, R., & Logemann, J. (2005). Swallow physiology in patients with trach cuff inflated or deflated: A retrospective study. Head & Neck, 27(9), 809-813. doi:10.1002/hed.20248 Frank, U., Mader, M., & Sticher, H. (2007). Dysphagic patients with tracheostomies: A multidisciplinary approach to treatment and decannulation management. Dysphagia, 22(1). 20-29. doi:10.1007/s00455-006-9036-5 Freeman, B. (2016). Tracheostomy update. Critical Care Clinics, 33(2), 311 322. https://doi.org/10.1016/j.ccc.2016.12.007 Freeman-Sanderson, A. L., Togher, L., Elkins, M., & Kenny, B. (2018). Quality of life improves for tracheostomy patients with return of voice: A mixed methods evaluation of the patient experience across the care continuum. Intensive & Critical Care Nursing, 46, 10 16. doi:10.1016/j.iccn.2018.02.004 Gaspar, M. d. R. d. F., Massi, G. d. A., Gon alves, C. G. d. O., & Willig, M. H. (2015). Nursing team and communication with tracheostomized patients. Revista CEFAC, 17(3), 734-744. doi:10.1590/1982-0216201514214 Harper, D., Buchanan, B., & Gandy, S. (2020) 1107: Analysis of the financial benefits from implementation of a multidisciplinary tracheostomy team. Critical Care Medicine, 48(1), 533. doi: 10.1097/01.ccm.0000643364.99050.54 Holmes, T. R., Cumming, B. D., Sideris, A. W., Lee, J. W., Briggs, N. E., & Havas, T. E. (2019). Multidisciplinary tracheotomy teams: An analysis of patient outcomes and resource allocation. Ear, Nose, & Throat Journal, 98(4), 232 237. doi:10.1177/0145561319840103 LeBlanc, J., Shultz, J. R., Seresova, A., de Guise, E., Lamoureux, J., Fong, N., Marcoux, J., Maleki, M., & Khwaja, K. (2010). Outcome in tracheostomized patients with severe traumatic brain injury following implementation of a specialized multidisciplinary tracheostomy team. The Journal of Head Trauma Rehabilitation, 25(5), 362 365. doi:10.1097/HTR.0b013e3181cd67ea
REFERENCES Magnus, V. S., & Turkington, L. (2006). Communication interaction in ICU--Patient and staff experiences and perceptions. Intensive & Critical Care Nursing, 22(3), 167 180. doi:10.1016/j.iccn.2005.09.009 Mah, J. W., Staff, I. I., Fisher, S. R., & Butler, K. L. (2017). Improving decannulation and swallowing function: A comprehensive, multidisciplinary approach to post-tracheostomy care. Respiratory Care, 62(2), 137 143. doi:10.4187/respcare.04878 Pandian, V., Miller, C. R., Mirski, M. A., Schiavi, A. J., Morad, A. H., Vaswani, R. S., Kalmar, C. L., Feller-Kopman, D. J., Haut, E. R., Yarmus, L. B., & Bhatti, N. I. (2012). Multidisciplinary team approach in the management of tracheostomy patients. Otolaryngology--Head and Neck Surgery: Official Journal of American Academy of Otolaryngology-Head and Neck Surgery, 147(4), 684 691. doi:10.1177/0194599812449995 Parker, V., Shylan, G., Archer, W., McMullen, P., Morrison, J., & Austin, N. (2007). Trends and challenges in the management of tracheostomy in older people: The need for a multidisciplinary team approach. Contemporary Nurse, 26(2), 177 183. doi.10.5172/conu.2007.26.2.177 Singh, R. K., Saran, S., & Baronia, A. K. (2017). The practice of tracheostomy decannulation - A systematic review. Journal of Intensive Care, 5, 38. doi:10.1186/s40560-017-0234-z Skoretz, S. A., Anger, N., Wellman, L., Takai, O., & Empey, A. (2020). A systematic review of tracheostomy modifications and swallowing in adults. Dysphagia, 35(6), 935 947. doi:10.1007/s00455-020-10115-0 Speed, L., & Harding, K. E. (2013). Tracheostomy teams reduce total tracheostomy time and increase speaking valve use: A systematic review and meta-analysis. Journal of Critical Care, 28(2). doi:10.1016/j.jcrc.2012.05.005 Tobin, A. E., & Santamaria, J. D. (2008). An intensivist-led tracheostomy review team is associated with shorter decannulation time and length of stay: A prospective cohort study. Critical Care (London, England), 12(2), R48. doi: 10.1186/cc6864