Torsemide vs. Furosemide in Heart Failure Management Study Overview
This study compares the long-term effects of torsemide versus furosemide in the management of heart failure. Torsemide may offer advantages such as more consistent oral bioavailability and longer action duration. The study aims to determine if torsemide reduces mortality by 20% compared to furosemide. The primary objective is to evaluate the impact of these loop diuretics on clinical outcomes in hospitalized HF patients. Enrollment began in June 2018, with 2973 consented participants. Recruitment ended in March 2022, with follow-up concluding in July 2022.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
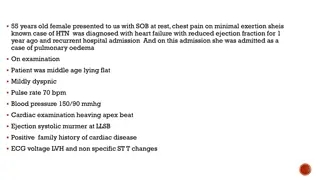
#AHA22 TORSEMIDE COMPARISON WITH FUROSEMIDE FOR MANAGEMENT OF HEART FAILURE Robert J. Mentz, MD On Behalf of the TRANSFORM-HF Investigators and Participants Supported through cooperative agreements from the NHLBI (U01-HL125478 and U01-HL125511)
Background LOOP DIURETICS are routinely used to manage congestion in patients with heart failure (HF) FUROSEMIDE is the most commonly used loop diuretic TORSEMIDE may offer advantages over furosemide More consistent oral bioavailability and longer duration of action Anti-aldosterone effects and anti-fibrotic myocardial effects Prior observational studies have suggested potential outcome benefits Whether torsemide improves clinical outcomes compared with furosemide in patients with HF is unknown. Murray MD, et al. Am J Med 2001;111(7):513-20. Cosin J, et al. Eur J Heart Fail 2002;4(4):507-13. Buggey J, et al. Am Heart J 2015; 169(3):323-33.
Primary Objective: Compare the treatment strategy of torsemide vs. furosemide on long-term clinical outcomes among patients hospitalized with HF through a pragmatic trial Design Regardless of EF Long-term plan for loop diuretic (60 US Sites) Hospitalized Patients with HF 1:1 Randomization Open-Label Dosing per Clinician Furosemide Torsemide DCRI Call Center (30 d, 6 m, 12 m) National Death Index Routine Clinical Follow-up No in-person study visits Primary Endpoint: Primary Hypothesis: Torsemide reduces mortality by 20% vs. furosemide Event-Driven 721 Death Events (85% power) All-Cause Mortality Secondary Endpoints: All-cause Mortality + All-cause Hospitalization Total Hospitalizations Health-related Quality of Life (KCCQ) Symptoms of Depression (PHQ-2) ClinicalTrials.gov Identifier: NCT03296813 Greene SJ, Mentz RJ, et al. JACC Heart Fail 2021; 9(5):325-335.
Study Execution Consented N = 2973 ENROLLMENT BEGAN June 2018 Excluded (N = 112, 3.8%) Did not meet eligibility (N=33) Discharged (N=30) PI decision (N=27) Patient decision (N=19) Death (N=3) 1,000 Patients Aug 2019 2,000 Patients Oct 2020 2,800 Patients Jan 2022 Randomized* N = 2859 Feb 2022 DSMB Meeting Recommend Ending Recruitment Sufficient Sample Size RECRUITMENT ENDS March 4, 2022 FOLLOW-UP ENDS July 29, 2022 Torsemide N = 1431 Furosemide N = 1428 Withdrawal of Consent N = 53 (3.8%) Withdrawal of Consent N = 60 (4.2%) All-Cause Mortality All-cause Mortality + All-cause Hospitalization Total Hospitalizations *Excludes 2 patients randomized twice (first randomization used)
Baseline Characteristics Torsemide (N=1431) 64 14 35% 58% 33% Furosemide (N=1428) 65 14 39% 59% 35% Characteristics Age (yr) Women White race Black race Newly diagnosed HF EF 50% 41-49% 40% NT-proBNP (pg/mL) Ischemic etiology 30% 22% 6% 65% 29% 23% 5% 63% LVEF 40% (N=1836) 3994 (1938, 8850) 30% 3833 (1936, 7807) 27% HFrEF Therapy Beta-blocker ACE/ARB/(ARNI) MRA SGLT2i 82% Systolic blood pressure (mmHg) Body mass index (kg/m2) eGFR (ml/min/1.73 m2) 118 19 32 10 59 25 119 21 32 9 60 26 68% (25%) 44% 8% Presented as %, Mean SD or median (IQR)
Loop Diuretic & Dosing Torsemide (N=1431) Furosemide (N=1428) Baseline Characteristics Loop diuretic prior to admission 964 (67%) 956 (67%) Furosemide 78% 81% Torsemide 15% 12% Bumetanide 7% 7% Total daily dose* (mg) 66 65 66 58 Torsemide (N=1431) Furosemide (N=1428) Randomized Loop Diuretic Discharge total daily dose* (mg) 80 70 79 56 *Furosemide equivalents (1 mg bumetanide = 20 mg torsemide = 40 mg furosemide)
Primary Endpoint: All-Cause Mortality HR 1.02 (95% CI, 0.89 to 1.18); P-value 0.77 Furosemide: 374 events (26.2%); 17.0 per 100 pt-yr Torsemide: 373 events (26.1%); 17.0 per 100 pt-yr Consistent across all pre-specified subgroups including Age, Gender, Race, EF, HF chronicity, GFR Median follow-up: 17.4 months (IQR: 8.0 to 29.0)
All-Cause Mortality or Hospitalization (12 mos) HR 0.92 (95% CI, 0.83 to 1.02); P-value 0.11 Furosemide: 704 events (49.3%); 107.6 per 100 pt-yr Torsemide: 677 events (47.3%); 99.2 per 100 pt-yr
Total Hospitalizations (12 mos) RR 0.94 (95% CI, 0.84 to 1.07) 1200 987 940 1000 Furosemide Torsemide 800 600 400 Among 577 (40.4%) Participants Among 536 (37.5%) Participants 200 0 Total Hospitalizations (N)
On-Treatment Analysis (Pre-Specified) Known diuretic status On randomized therapy Torsemide N = 1431 Furosemide N = 1428 Unknown Loop Status (N=40) Death (N=4) Known Loop Status (N=1384) Different Loop (N=75) Crossover (N=53) 3.8% No Loop (N=41) 3.0% Unknown Loop Status (N=57) Death (N=3) Known Loop Status (N=1371) Different Loop (N=112) Crossover (N=96) 7.0% No Loop (N=36) 2.6% 5.4% Cross-over 2.8% No Loop On-Treatment at Discharge N = 1223 On-Treatment at Discharge N = 1268 Unknown Loop Status (N=351) Death (N=56) Known Loop Status (N=1016) Different Loop (N=92) Crossover (N=81) 8.0% No Loop (N=76) 7.5% Unknown Loop Status (N=325) Death (N=63) Known Loop Status (N=1031) Different Loop (N=102) Crossover (N=57) 5.5% No Loop (N=67) 6.5% 6.7% Cross-over 7.0% No Loop On-Treatment at 30 Days N = 848 On-Treatment at 30 Days N = 862 On-Treatment at Discharge 0.99 (0.85, 1.15) P=0.86 0.91 (0.81, 1.01) P=0.082 On-Treatment at 30 Days 0.96 (0.78, 1.18) P=0.69 0.89 (0.78, 1.02) P=0.10 ITT Analysis 1.02 (0.89, 1.18) P=0.76 0.92 (0.83, 1.02) P=0.11 All-cause mortality All-cause mortality or all-cause hospitalization
Limitations and Future Opportunities Cross-overs and diuretic discontinuation would bias toward neutral results Dose was left to clinician discretion which may have influenced results All-cause outcomes may have been too imprecise for measuring differences especially during the COVID-19 pandemic Assumed treatment effect was large (especially with evolution of GDMT) No assessment of other adverse events (e.g., worsening renal function, electrolyte abnormalities or non-hospitalization events) Future work will characterize how non-adherence and dose may have affected these findings
Pragmatic Trial Insights Broad eligibility criteria and streamlined study protocol embedded within routine care supported the inclusion of diverse participants Pragmatic elements lowered traditional barriers for patient and site participation supported robust enrollment rates (even during the COVID-19 pandemic) Opportunities to enhance patient adherence and engagement at follow-up In this context, this real-world comparative-effectiveness study provides results that are generalizable to routine clinical practice
Conclusions and Implications A strategy of torsemide had similar effectiveness compared with a strategy of furosemide for the clinical outcomes of mortality and hospitalization in patients hospitalized with heart failure. Clinical time should be spent focusing on appropriate diuretic dosing and prioritizing guideline-directed medical therapy (GDMT) initiation / titration. Insights from the pragmatic trial design and execution inform future studies aiming to assess real-world comparative effectiveness.
Thank you! TRANSFORM-HF Investigator Teams, Sponsor, DSMB & Participants EXECUTIVE COMMITTEE, NHLBI AND COORDINATING CENTER Velazquez EJ (Co-PI, CCC), Mentz RJ (Co-PI, CCC), Anstrom KJ (Co-PI, DCC), Eisenstein EL (Co-PI, DCC), Pitt B (Chair), Greene SJ; NHLBI: Desvigne-Nickens P, Ketema F, Kim D and Sachdev V; CC: Morgan S, Settles S, Sapp S, Harrington A, Seow H. DATA AND SAFETY MONITORING BOARD Vaughan D (Chair), Chan EC, D Agostino RB, Dube MP, Johnson M, Parrillo J, Penn MS, Rose EA SITE INVESTIGATORS AND THEIR TEAMS Abbate A, VCU Adams KF, UNC Adler AA, Methodist Alexy T, U Minnesota Ambrosy AP, KP Nor Cal Arhinful JS, Cox Health Axsom KM, Columbia Banerjee D, Queen s Med Bell AC, Wellspan Bhatt K, Emory Clark JM, Main Line Davis W, Adv CV DeWald T, Duke Dunlap SH, Augusta D Urso M, Monument Eberly AL, Greenville Fang JC, U Utah Ferguson AD, Indiana Friedman D, Adventist Gaglianello NA, MCW Gottlieb SS, VA Med Center Goyal P, Weill Cornell Grafton GF, Henry Ford Guglin M, Indiana - Methodist Haas DC, Abington Hall ME, U Mississippi Hasni S, Drexel Haught WH, The Heart Ctr Heroux AL, Loyola Herre JM, Sentara Norfolk Hummel SL, Michigan Krim SR, Ochsner Lala-Trindade A, Mount Sinai Larned JM, Holy Cross Lev YA, Jefferson McCulloch MD, Intermountain Meadows JL, West Haven VA Mizyed AM, Saint Joseph Mercy Mody FV, VA Greater LA Muneer B, Fox Valley Murthy S, Montefiore Psotka MA, Inova Ramasubbu K, Brooklyn Methodist Rich JD, Northwestern Robinson MT, Case Western Rommel JJ, New Hanover Ruiz Duque EA, U Iowa Sherwood M, Baylor Shetty S, AtlantiCare Skopicki HA, Stony Brook Smart F, Univ Med Ctr NO Smith BA, U Chicago Stevens GR, Northwell Tabtabai SR, Saint Francis Tang WHW, Clev Clinic Tejwani LK, Novant Health Testani J, Yale Vader JM, Washington U Vilaro JR, U Florida William P, U Arizona