Tissue Viability and Pressure Ulcer Prevention Practices in Healthcare
Helen Harris, a Tissue Viability Nurse Specialist, oversees the management and advice for service users with complex wounds, advanced therapies, and pressure ulcer prevention cases. Her role includes developing strategies, policies, and procedures for Tissue Viability services, catering to a population of approximately 437,000 individuals. The focus is on preventative care through risk assessment, care planning, skin assessment, and repositioning strategies for at-risk individuals.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
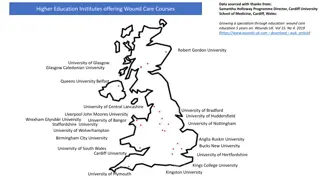
Tissue Viability Good Preventative Practice Helen Harris Tissue Viability Nurse Specialist
What is Tissue Viability? Management and advice for service users with complex wounds Management of advanced therapies Support complex pressure ulcer prevention cases Responsible for all TV strategy, policy and procedure
Service provision Anyone with a complex need who is registered with BANES or South Glos GP 3 community hospitals Care home support Approx 437,000 population
Tissue Viability - Prevention Pressure ulcers Incontinence dermatitis General skin care
Pressure ulcer prevention Grade 3 and 4 threshold for safeguarding Multiple grade 2 s considered Multiple patients in one setting
Good Preventative care Risk assessment Consider reliability Use clinical judgement Must be re-evaluated when condition changes Must only be a aide memoir Poor predictor in wheelchair users and maternity The clinician who carries out and signs the risk assessment is responsible for devising prevention strategies
Care Planning Care plan must be implemented for anyone high risk to include Outcome of risk assessment The need for additional pressure relief at risk sites Their mobility and ability to reposition Co-morbidities Patient preference
Skin assessment All risk areas Any areas of discomfort Variations in heat / moisture / firmness
Repositioning Adults at risk should be encouraged to reposition at least every 6 hours and high risk at least every 4 hours Assist those that can t Document the frequency of repositioning required
Equipment Utilise high specification foam for those patients in hospitals / nursing homes or assessed as high risk in the community Use heel protectors for those at risk Utilise dynamic systems for those where static systems are not sufficient
Incontinence dermatitis Severe cases predominantly avoidable in a 24 hours setting Good continence management Use of appropriate barrier creams
General Tissue Viability Good skin management Use of appropriate moisturisers Good documentation including evaluation of any treatment or prevention plans Appropriate and timely referral on taking into consideration patient choice
Summary Personalised care planning taking into account patient choice Evaluation of any care plans in a timely manner Clear and accurate documentation
Thank you Any questions?

 undefined
undefined