The Low FODMAP Diet for Managing IBS
Irritable Bowel Syndrome (IBS) is a common condition that affects millions of people, with symptoms like abdominal pain, bloating, and altered bowel habits. The Low FODMAP diet is a promising approach to managing IBS by reducing certain types of carbohydrates that can trigger symptoms. This diet involves eliminating high-FODMAP foods and gradually reintroducing them to identify triggers. Understanding the causes of IBS, such as gut-brain interactions and food intolerances, is crucial for effective management. Implementing the Low FODMAP diet in practice can greatly benefit individuals suffering from IBS.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Low FODMAP Diet Latest Treatment of IBS Laura Manning, MPH, RD, CDN Susan and Leonard Feinstein Center for IBD Department of Gastroenterology Mount Sinai Medical Center
Agenda 1. What is IBS and possible causes 2. Review-How do we digest short chain carbs 3. What is the Low FODMAP diet 4. How to implement it in your practice 1
Irritable Bowel Syndrome (IBS) A condition characterized by abdominal pain, bloating, flatus and altered bowel habits1. - Induced by intestinal luminal distention in addition to visceral hypersensitivity. - Dietary factors may alter luminal distention with increased water and gas volume, causing diarrhea. - Other symptoms: tiredness, heartburn, nausea, fogginess. 1. Camillieri, M. Am J Physiol Gastrointest Liver Physiol, 2012. 2
Facts about Irritable Bowel Syndrome (IBS) Affects 25 to 45 million people in US, more common in females. Usually under the age of 50 Possible cause: disturbance in the gut-brain- nervous system interact. Impacts physical, emotional, financial and social well being. Typically brought on by stress. Few seek medical care- 20-40% of GI visits are due to IBS.* 3 *International Foundation for Functional Gut Disorders (IFFGD) https://www.aboutibs.org/site/what-is-ibs/facts/
Allergy vs. Intolerance Food Allergy- the reproducible adverse reaction arising from specific immune responses occurring from specific food antigens. IgE mediated Food Intolerance- Similar reactions that occur without evidence of immunologic mechanisms.2 (causing IBS) 5 2. Boettcher E, Crowe SE. Am J Gastroenterology, 2013.
Possible causes Malabsorption of carbohydrates causing onset of symptoms.3 Non Celiac Gluten Sensitivity (NCGS)- new clinical condition.4 3. Sheparhd SJ, et al. Clin Gastroenterol Hepatol, 2008 4. Biesiekierski JR, et al. Am J Gastroenterol, 2011 6
Current Food Trends Fructose-Our intake of fructose is increased to 22% of daily caloric intake-High fructose corn syrup (HFCS) in soda, candy and food products. Fructans- due to a wheat-heavy culture. Inulin- added in Functional Foods , formulas! Polyols- sugar free additives to lower calories and to protect teeth (gums and mints). 7
Fructose and Fructans Largest amount in North American and Western European diets 8
Changes in gut bacteria Patients with IBS may have lower Lactobacillus and Bifidiobacterium species in their intestinal flora.5 High meat and dairy diets are shown to change gut flora 5. Kassinen A, et al. Gastroenterology. 2007 9
Alteration of Gut Bacteria High antibiotic use, especially in children C-sections High animal protein and dairy diet Intestinal surgeries: ICR, bariatric Celiac disease Motility disorders: gastroparesis Inflammatory Bowel Disease (IBD) Post infectious IBS: gastroenteritis Small Intestinal Bacterial Overgrowth (SIBO) 11
Maybe they cant digest certain carbohydrates? FIBER- long chain, non-digestible carbs in small intestine. Important for stool formation an proper bowel function STARCH- long chain carbs completely digested in the small intestine. SUGARS- short chain carbs that may or may not be easily digested. Depends on the type . 12
How are they not digested Malabsorbed and pull water (osmotic shift) in to the small intestine and cause diarrhea. When sugars reach the large intestine, they ferment by bacteria and cause gas. The gas can slow movement through the bowel causing constipation. Additionally: nausea, bloating, and cramps. 13
14 http://www.ncbi.nlm.nih.gov/core/lw/2.0/html/tileshop_pmc/tileshop_pmc_inline.html?title=Click%20on%20image%20to%20zoom&p=PMC3&id=3966 170_GH-11-739-g002.jpg
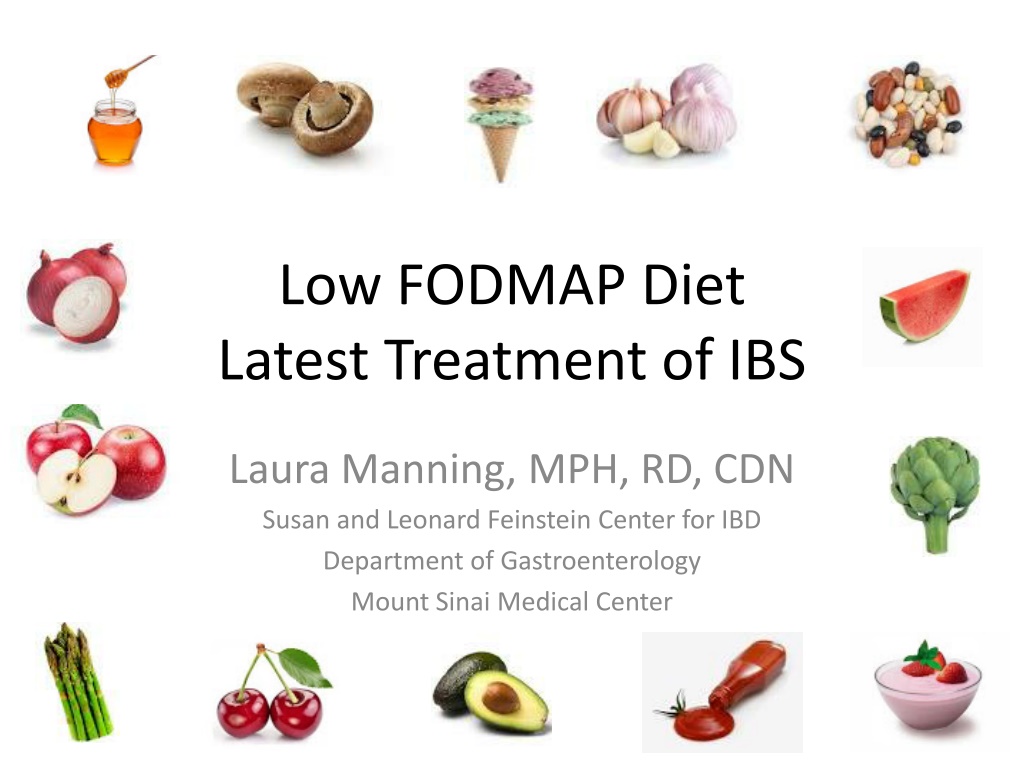
Fermentable Oligo-Di- Monosaccharides and Polyols (FODMAPs) A heterogeneous group of poorly absorbed, short-chain carbohydrates, which seem to be possible IBS symptom inducers. Restricting these from the diet could produce beneficial effects. Term coined in 2005 by a group of Australian researchers at Monash University claiming that these forms of carbs may worsen symptoms of IBS and IBD.6 15 6. Gibson PR, Shepard SJ. Aliment Pharmacol Ther. 2005.
Shepard, SJ. Et al. J Am Diet Assoc. 2006 Using a retrospective study-74% of patients reported symptom improvement utilizing the Low FODMAP diet regimen. 16
Halmos EP, Gastroenterology. 2014 Crossover study where patients with IBS effectively reduced functional GI symptoms when on a Low FODMAP diet. * FODMAPs are not the cause of functional bowel disorders, but will act as a trigger. 17
FODMAPs Lactose- dairy Fructose- fruits Fructans/GOS- wheat, beans Polyols- sugar alcohols 18
Digestion of Fructose Free fructose, a simple sugar, requires no digestion. -Absorbed in the small intestine in 2 ways: 1. Co transport with GLUT-2 (a glucose/ fructose transporter). If equal amounts of glucose are available , fructose is efficiently taken up after sucrose hydrolysis. 2. And by alternative transporter GLUT 5 in excess fructose amounts which is present in the border of enterocytes in small intestine. * If fructose load is very large, malabsorption likely will occur 20
Fructose Malabsorption 40% of the population are considered to have fructose malabsorption.7 We can typically digest fruits if they have a 1:1 ratio of glucose to fructose. On the diet, 1 serving per day. 21 7. Douard V. J Physiol. 2013.
Fructose Fruits: Apples, cherries, mangoes, pears, watermelon Vegetables: asparagus, artichokes, sugar snap peas Honey, HFCS More intensified in dried fruits and overall volume amounts 22
Lactose A di-saccharide (Glucose and Galactose) - Requires lactase enzyme to break it down in small intestine - Typically occurs in quantities greater than 7g 1. Varying enzymes amounts in the gut are influenced by: Genetics Ethnic background Gut disorders 23
Lactose Milk: cow, goat and sheep Yogurt Ice cream Custard Soft Cheeses: Ricotta, cottage 24
Oligosaccharides Fructans and Galactans (GOS) Fructans and Galactans are the storage carbohydrate of many vegetables Fructose polymer with a glucose terminal end - We do not have the enzymes to break these down and therefore are rapidly fermented, causing gas and bloating - Typically a great pre-biotic! 25
Fructans Peach, persimmon, watermelon Artichokes, asparagus, Brussels sprouts, chicory, fennel, garlic, onions, leeks Wheat, rye, barley Pistachios, cashews Beans Inulin 26
GOS Beans- raffinose - Lacking the enzyme a-galactosidase Baked beans, kidney beans, chick peas, Brussels sprouts and cabbage 27
Polyols The sugar alcohols/ sugar substitutes: Only 1/3 is absorbed in small intestine - By passive diffusion dependent on molecular size and pore size in the small intestine. Sorbitol, Mannitol, Xylitol, Erythriol, Isomalt Foods: Apples, apricots, cherries, blackberries, plums, mushrooms, cauliflower Laxatives 28
A Bucket Effect- all FODMAPs are consumed at once causing a cumulative effect! 29
Typical meal Breakfast: Frosted Mini Wheats and milk, tea with honey Lunch: wheat bread with turkey and American cheese and an apple, cranberry juice Snack: regular, peach flavored yogurt and pretzels Dinner: pasta with tomato sauce and meatballs with a side of asparagus Snack: handful of cashews 30
Loaded with FODMAPs Breakfast: Frosted Mini Wheats and milk, tea with honey Lunch: wheat bread with turkey and American cheese and an apple, cranberry juice Snack: regular, peach flavored yogurt Pretzels Dinner: pasta with tomato sauce and meatballs with a side of asparagus Snack: Handful of cashews 31
High FODMAP Foods & Crossover Lactose Fructose Fructans/ GOS Polyols Milk Artichoke Artichoke Cauliflower Yogurt Asparagus Garlic Mushrooms Ice cream Tomatoes Onions Peas Ricotta Apples Beans Apples Cottage Cherries Apples Pears Custard Figs Figs Plums Pears Plums Watermelon Watermelon Wheat Sorbitol Agave Inulin Xylitol Honey Pistachios HFCS Watermelon 32
Variations to consider Clinical testing at Monash Univ. Formal list constructed from mechanical testing of foods Different levels in foods depending on ripeness Different volume of carb load per person Different levels of tolerance per person Some foods have not been tested yet 33
Further Modifications Change the texture of the diet based on the patient symptoms. Ex: IBS-D - Cook all vegetables, no salads - Have nut butters over nuts - Lower fat overall - No fruits on an empty stomach 34
Low FODMAP Diet-Best approaches Work with a dietitian familiar with the diet Step 1: Elimination Phase. A global restriction will have better outcomes versus choosing 1-2 categories to limit.7 A temporary diet: 2-6 weeks max Step 2: Reintroduction Phase. Intro of one category at a time to test intolerance and volume limits 35
Low FODMAPs Lactose: Aged cheese, LF dairy, Brie, Mozzarella, kefir, LF yogurt- plain, rice milk, coconut milk Fructose: (1 serving per meal) bananas, blueberries, strawberries, grapes, honeydew, cantaloupe, maple syrup, table sugar Fructans/GOS: bok choy, bell peppers, Swiss chard, carrots, spinach, zucchini, GF breads, GF pasta, potatoes, quinoa, oats, polenta, 10-15 nuts: almonds, macadamia, peanuts, pine nuts, pumpkin seeds, flax and chia seeds. Firm tofu, tempeh Polyols: banana, blueberry, cantaloupe, coconut, lemon, limes, papaya, rhubarb, table sugar, maple syrup, aspartame, stevia 36
Moderate FODMAPs Fructans: (limited to 1 choice per meal) beet root- 4 slices, broccoli-1/2 cup, butternut squash-1/4 cup, peas -1/3 cup, pomegranate-1/2 small, sweet corn-1/2 cob, canned pumpkin -1/4 cup, canned chickpeas-1/4 cup, canned lentils-1/2 cup Polyols: (limited to 1 choice per meal) avocado-1/8, celery-1/4 stalk, sweet potato-1/2 cup Beverages: espresso, tea: black/white/green/mint, Alcohol: (limited to 1 drink per day) most wine and beer, vodka, gin and whisky 37
Proficient Label Reading! A label may contain a high FODMAP ingredient, but look where it falls on the list 38
What about Fats and Proteins? All fats are fine- no carb in them The following proteins are acceptable: - Poultry, beef, lamb, pork, eggs and fish - Nuts, limited to a handful. Nut butters, 2 TBS - Firm tofu, tempeh, seitan 40
Elimination phase- Sample diet Snack cup lactose free cottage cheese 8 cherry tomatoes Dinner 3 ounces baked salmon 1 cup cooked zucchini Medium baked potato 1.5 tbsp sour cream 2 cups raw spinach cup sliced bell pepper 1 tsp evoo 1 tbsp balsamic vinegar Breakfast: 1 cup corn flakes 1 cup lactose free milk ripe banana 1 cup coffee with lactose free milk and 1 tsp sugar Snack Handful of almonds Lunch 2 slices spelt sourdough bread 2 ounces of turkey 1 tablespoon real mayo Lettuce and tomato cup fresh blueberries cup baby carrots Drinks: water, allowable tea 41
Adding Flavor Garlic infused oils- cook garlic in oil and remove Herbs: (keep em fresh) basil, cilantro, coriander, rosemary, parsley, tarragon, thyme Stock- made without garlic and onions 42
Eating out Review menus ahead of time on line and have a plan of action Give instruction about how you would like food to be cooked- baked, broiled, lemon and herbs. Bring snacks, avoid being un-prepared when starving 43
Possible Negative Implications Avoid eliminating whole food groups May be low fiber content - Work in chia seeds, psyllium husk, ground flax and allowable whole grains Limited intake of Prebiotics may not be beneficial for extended periods of time, decreasing concentrations of bifidiobacteria. 8 44 Staudacher, et al. J Nutr, 2012.
Reintroduction Phase 1. As soon as the person starts to feel like their symptoms have significantly lessened, start introducing foods back into to the diet- one category at a time 2. Do not use foods that cross over categories 3. Introduce a small amount, once a day for three days 4. Check in to see if there is any reoccurrence if no, return to Low FODMAP diet and start the next category! 5. Keep a log of symptoms as you go 45
Sample Re-Intro Fructanswheat, garlic and onions should be tested separately Monday, Tuesday, Wednesday- add 1 teaspoon of chopped garlic to one meal ONCE a day. If ok, resume Low FODMAP diet and go to next category Fructose Thursday, Friday, Saturday- add 1-2 tsp of honey once a day. 46
Re-Intro Lactose- drink cup of milk Polyols- test Sorbitol and Mannitol separately - Sorbitol, have 1 peach - Mannitol, have cup mushrooms once a day GOS- have cup of kidney beans * If person failed a challenge, resume low FODMAP diet and wait three days without symptoms. 47
Diet Of Info! Person walks away with information on how to manage their condition and can choose to alter their diet as needed. * Gives a sense of empowerment! 48
Important movers and shakers in the Low FODMAP method: Patsy Catsos, MS, RDN, LD Kate Scarlatta, RD Monash University, Aurtralia:http://www.med.monash.edu/cecs/ gastro/fodmap/ Mark Pimentel, MD The New IBS Solution 49

![READ [PDF] Dash diet Cookbook for beginners: 365 days of simple, healthy, low-s](/thumb/2057/read-pdf-dash-diet-cookbook-for-beginners-365-days-of-simple-healthy-low-s.jpg)
![[✔PDF✔⚡] Renal Diet Cookbook for the Newly Diagnosed: The Complete Guide to](/thumb/68079/pdf-renal-diet-cookbook-for-the-newly-diagnosed-the-complete-guide-to.jpg)