Study on Young Onset Colorectal Cancer in Southwest England
The study focuses on young adults under 50 diagnosed with colorectal cancer in the Somerset, Wiltshire, Avon, and Gloucestershire regions. It aims to capture data on their epidemiology, diagnostic pathways, management, and outcomes from 2009 to 2019. The background and incidence trends both globally and in the US, UK, and Europe are discussed, highlighting the rising trend of young onset colorectal cancer.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
The The S Somerset, omerset, W Wiltshire, G Gloucestershire loucestershire Y Young C Cancer (SWAG ancer (SWAG- -YOCC) Study iltshire, A Avon and oung- -O Onset nset C Colorectal YOCC) Study von and olorectal David Messenger Consultant Colorectal Surgeon University Hospitals Bristol
A retrospective multicentre observational cohort study of the diagnostic pathways, management and outcomes of adults aged under 50 years with colorectal cancer in the Somerset, Wiltshire, Avon and Gloucestershire Clinical Alliance
Aim Aim To determine the feasibility of capturing data on all adults <50 years diagnosed with colorectal cancer in the SWAG Clinical Alliance from September 2009 to September 2019 in order to describe their epidemiology, diagnostic pathways, management and outcomes
Background Background Worldwide, US, UK (English) and European incidence trends Demographic trends in young onset colorectal cancer in England Projected impact on the South West What is known about young onset colorectal cancer
Worldwide Incidence Worldwide Incidence Ferlay et al., GLOBOCAN 2012, IARC 2012 2030 1.4 million 2.2 million
US Incidence Trends US Incidence Trends Zauber, Dig Dis Sci 2017 Siegel et al., JNCI 2017
English Incidence Trends English Incidence Trends Colon Rectum Chambers et al., Br J Surg 2020
European Incidence Trends: Young adults European Incidence Trends: Young adults Driven by rise in proximal > distal tumours Vuik et al., Gut 2019
Demographic trends in England: Site Demographic trends in England: Site Chambers et al. Br J Surg 2020
Demographic trends in England: Region Demographic trends in England: Region Proximal Distal Chambers et al. Br J Surg 2020
2016 Incidence estimates: South West 2016 Incidence estimates: South West Age group (yrs) 2016 population 2015 Incidence rate (per 100,000) Estimated number of cases in 2016 % 20-29 410,100 1.5 6.2 30-39 367,700 6 22.1 4.0% 40-49 407,700 16 65.2 50-59 437,900 55 241 60-64 192,700 120 231 65-69 213,100 139 296 70-74 172,500 214 369 96.0% 75-79 124,400 295 367 80-89 154,900 394 610 90+ 37,300 350 131 Total 2,518,300 92.9 2338.5
2041 Incidence estimates: South West 2041 Incidence estimates: South West Age group (yrs) 2041 population 2041 Projected Incidence rate (per 100,000): current APC Estimated number of cases in 2041: current APC % 2041 Projected Incidence rate (per 100,000): SW-specific APC Estimated number of cases in 2041: SW-specific APC % 20-29 443,700 5.0 22.2 16.3 72.3 30-39 408,000 19.8 80.8 65.0 265 7.2% 30.0% 40-49 413,200 21.6 89.3 173 716 50-59 433,100 72.3 313 72.3 313 60-64 207,100 105 217 105 217 65-69 211,700 31.2 66.1 31.2 66.1 70-74 230,700 57.5 133 57.5 133 92.8% 70.0% 75-79 216,400 198 429 198 429 80-89 277,800 358 995 358 995 90+ 92,500 333 308 333 308 Total 2,934,200 90.4 2653.4 120 3514.4
Young onset rectal cancer: Norway Young onset rectal cancer: Norway <40 years 40 years P-value At presentation Poorly differentiated 27% 14% 0.014 N2 disease at presentation 37% 16% 0.001 Metastatic disease at presentation 38% 22% 0.019 Treated with curative intent Develop metastatic disease 56% 23% 0.003 5-year Overall Survival 54% 80% 0.029 Endreseth et al. (Norwegian Rectal Cancer Group), Dis Col Rectum 2006
Young onset colorectal cancer (sporadic): US Young onset colorectal cancer (sporadic): US Tumour location n % Group 3-year OS 5-year OS 10-year OS Overall 76.2% 66.8% 58.6% Proximal 25 17% Left 34 23% Genetic/IBD 94.6% 91.4% 87.9% Rectum 91 61% Sporadic 70.6% 61.5% 53.3% Kozak et al., Colorectal Dis 2017 Liang et al., Int J Colorectal Dis 2015 Molecular feature <50 yrs 50-59 yrs 60-69 yrs 70-79 yrs 80+ yrs CIMP-H 0% 5% 18% 28% 42% BRAF mutation 0% 2% 8% 15% 20% MSI-high 0% 14% 23% 28% 28% Chouhan et al., Dis Colon Rectum 2019
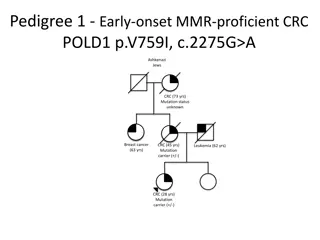
Rationale Rationale Young onset colorectal cancer is increasing Driven by increase in distal tumours in England South West experiencing >10% per annum increase in distal tumour incidence By 2041, young adults may account for up to 30% of all cases Lack of detailed understanding of characteristics of the young onset colorectal cancer population Likely more advanced at presentation No UK data
Study Design Study Design Two-phase retrospective observational cohort study Phase 1: University Hospitals Bristol, North Bristol, Royal United Hospital Phase 2: Taunton & Somerset, Yeovil District Hospital, Gloucestershire Hospitals, Weston General Hospital, Salisbury Completion of Phase 1 will demonstrate deliverability of Phase 2 All adults aged <50 years with new diagnosis of colorectal cancer are eligible
Inclusion/Exclusion Criteria Inclusion/Exclusion Criteria Inclusion criteria Aged from 18 to 49 years at the time of diagnosis between September 2009 and September 2019 Biopsy proven adenocarcinoma of the colorectum Exclusion criteria Aged under 18 years or over 49 years at the time of diagnosis Non-adenocarcinomas of the colorectum Appendiceal neoplasms Neoplasms of the anal canal or perianal region Previous diagnosis of a colorectal adenocarcinoma before September 2009
Outcome measures Outcome measures Primary outcome measure Complete multidisciplinary team (MDT) at each hospital trust Key secondary outcome measures Proportion of cases presenting as an emergency Proportion of cases with stage IV disease at presentation Proportion of cases undergoing resection with curative intent Response to neoadjuvant therapy Local recurrence, Disease free survival, Overall survival Proportion of cases with stoma at 18 months following surgery Proportion of cases in each data field submitted to the NBOCA where data entry is correct (highlighted as important outcome by ACPGBI PPI group) data collection on 90% of cases presenting via the
Sample Size Estimates Sample Size Estimates No formal power calculation is required as primary endpoint is to demonstrate completeness of data collection Average of 120 eligible cases over last 10 years per Trust Assuming 90% complete data collection Phase 1 (UHB,NBT,RUH): Phase 2 (YDH,TST,WHAT,GH,SAL): 0.9 x 120 x 3 = 324 0.9 x 120 x 5 = 540 Total = 864
Data Collection Data Collection Surgical trainees will collect data and be supported by nominated consultant PI at each Trust (Research collaborative model) Identification of cases from Somerset Cancer Registry and data submissions to NBOCA Direct date entry onto electronic case report form on REDCap database Pseudoanonymised data with unique study ID Logic checks Study period chosen to coincide with widespread use of electronic medical records 3-month data collection period anticipated for each phase
Dissemination of Results Dissemination of Results Investigators can present Trust level data at departmental meetings Data from phase 1 and 2 to be presented to key stakeholders SWAG Clinical Alliance Patient Support Groups Primary Care Groups Presentation at national/international conferences Submission to peer reviewed journals All publications will be attributed to the SWAG-YOCC group
Future Directions Future Directions Provide platform for prospective multicentre observational study Demonstration of feasibility Allow collection of additional data fields: quality of life, tissue samples Inform design of studies addressing key questions Effectiveness of neoadjuvant therapy in young adults Timing of surgery within treatment pathway Expansion of FIT usage as screening tool in young adults Allow linkage to future biomolecular and epidemiological studies
Steering Group Membership Steering Group Membership University Hospitals Bristol David Messenger, Adam Chambers North Bristol Trust Ann Lyons Royal United Hospitals Isi Tonga, Ed Courtney University of Bristol Professor Richard Martin, Professor Caroline Relton (Epidemiology) ACPGBI Professor Bob Arnott (Patient Liaison Group & NBOCA Patient Panel Chair) Nominated lead Consultant & Surgical Trainee contact at each Trust
Current Status Current Status Sponsorship obtained from University Hospitals Bristol Protocol currently undergoing peer review Ethical approval to be sought through Proportionate Review Service REDCap database built and undergoing testing